REGISTRO DOI: 10.5281/zenodo.11238602
Honassys R Rocha Silva1
ABSTRACT
Angle-closure glaucoma is a significant threat to visual health, characterized by increased intraocular pressure due to obstruction of the aqueous humor drainage angle. An effective preventive strategy is prophylactic laser iridotomy, where a small hole is artificially created in the iris, allowing intraocular fluid to flow freely between the posterior and anterior chambers, helping to control intraocular pressure. This article describes a novel technique for the photographic documentation of prophylactic laser iridotomy, which offers advantages in terms of documentation, monitoring, and follow-up for patients at risk of developing angle-closure glaucoma.
Keywords: Irodotomy, Yag Laser, Glaucoma, Smartphone Eye Photography.
INTRODUCTION
Angle-closure glaucoma is an ocular condition that can lead to irreversible vision loss if not diagnosed and treated early. An effective preventive approach is Prophylactic Laser Iridotomy, which aims to create a hole in the periphery of the iris, allowing the aqueous humor, responsible for maintaining intraocular pressure, to flow freely between the posterior and anterior chambers, helping to control this pressure1-3.
Laser iridotomy can be performed prophylactically in individuals at risk of developing an acute crisis or in patients experiencing a full-blown acute crisis4. Iridotomy also has other indications, such as in pigmentary glaucoma5 and plateau6.
Angle-closure glaucoma is a significant cause of blindness due to glaucoma7. Iridotomy is safe and can be used prophylactically in individuals at risk of angle-closure glaucoma8.
Therefore, it is crucial to document the iridotomy to ensure its functionality.
This article describes a method of documenting the result of peripheral laser iridotomy using the same equipment with which the procedure was performed, a simple and easily adoptable technique.
METHODS
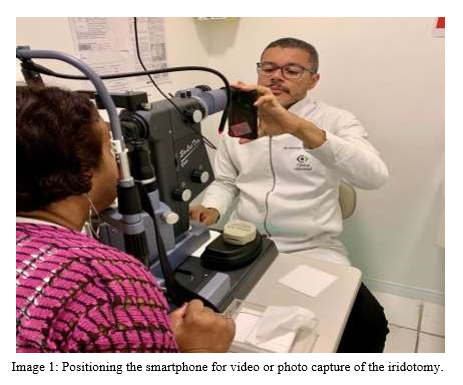
The technique for photographic documentation of prophylactic laser iridotomy involves capturing high-resolution images of the patient’s eye after the procedure, using a smartphone and the slit lamp of the laser itself. To adequately document the hole created in the iris, the following steps are followed:
1 Patient preparation: Administration of 2% Pilocarpine eye drops and anesthetic (Oxybuprocaine Hydrochloride 4mg/ml)
2 Iridotomy execution: The ophthalmologist performs the laser iridotomy, creating a small hole in the periphery of the iris. In this study, the LightMed Lightlas Yag/SLT Deux system laser was used.
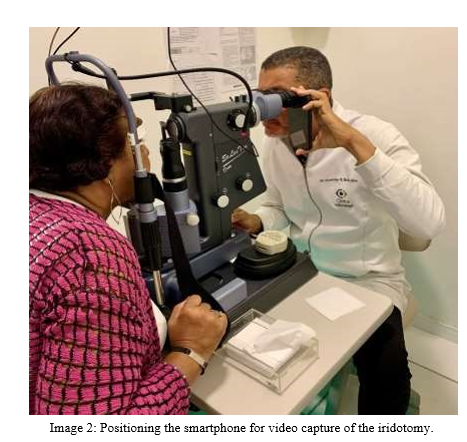
3 Preparation of the laser slit lamp: Reducing the light beam intensity of the slit lamp to a minimum and increasing the intensity of the red aiming light to the maximum.
4 Turning off the room lights: To improve image quality by avoiding corneal reflections.
5 Post-procedure image capture: The high-resolution smartphone camera is aimed at the iridotomy, touching the objective lens of the laser slit lamp. A video of the iris is then captured. A frame from this video is selected to highlight the iridotomy. The smartphone used was an iPhone 11 Pro (Apple).
6 Image processing: Not recommended to maintain originality.
7 Image recording: The images are recorded and stored in the patient’s medical record for future use.
RESULTS
The documentation was carried out using a smartphone positioned on one of the laser’s objectives, as shown in Image 1. Next, the slit lamp illumination was turned off, and the iridotomy aiming light (red) was directed to the center of the pupil. The objective is for the retina to reflect this light and backlight the newly created hole (Images 2 and 3); a video was then captured through the smartphone, and a frame from this video was selected for documentation.
The video of what was seen by the physician can be accessed at: https://vimeo.com/user16271010/iridotomyrecordtechnique?share=copy

This image can be included in the electronic medical record and sent to the patient and their ophthalmologist.
DISCUSSION
The technique for photographic documentation of prophylactic laser iridotomy offers several clinical advantages. Firstly, it provides a clear visual record of the hole in the iris, allowing precise documentation of the procedure. This is crucial for monitoring the size, position, and integrity of the hole over time.
Additionally, the recorded images can be used for educational purposes, allowing patients to understand the procedure and its benefits. The technique also facilitates communication between physicians and other healthcare professionals, improving treatment coordination.
To be considered functional, the iridotomy must be at least 150 microns in size9. In case of doubt, the photographic documentation can help determine the size of the iridotomy, although this is not the primary objective of this article.
Other methods for documenting an iridotomy include anterior segment photography, anterior segment optical coherence tomography (AS-OCT)10, and Pentacam10-12. A less accessible alternative is ultrasound biomicroscopy13. The disadvantage of this technique is the inability to document the depth of the anterior chamber of the eye, which is possible using technologies such as AS-OCT and Pentacam.
CONCLUSION
The technique for photographic documentation of prophylactic laser iridotomy represents a valuable innovation in the prevention of angle-closure glaucoma. By allowing precise and measurable documentation of the procedure, this approach contributes to effective monitoring of patients at risk. Additionally, it offers educational and communication benefits, strengthening the relationship between physicians and patients. Based on the literature review, the technique is supported by well-established ophthalmological principles and demonstrates promising clinical potential.
REFERENCES
1 Flores-Sánchez, B. C. & Tatham, A. J. Acute angle closure glaucoma. Br J Hosp Med 80, C174– C179 (2019).
2 Chan, P. P., Pang, J. C. & Tham, C. C. Acute primary angle closure–treatment strategies, evidences and economical considerations. Eye (Basingstoke) vol. 33 Preprint at https://doi.org/10.1038/s41433-018-0278-x (2019).
3 Wright, C., Tawfik, M. A., Waisbourd, M. & Katz, L. J. Primary angle-closure glaucoma: An update. Acta Ophthalmologica vol. 94 Preprint at https://doi.org/10.1111/aos.12784 (2016).
4 Lee, J. W., Lee, J. H. & Lee, K. W. Prognostic factors for the success of laser iridotomy for acute primary angle closure glaucoma. Korean J Ophthalmol 23, (2009).
5 Reistad, C. E. et al. The influence of peripheral iridotomy on the intraocular pressure course in patients with pigmentary glaucoma. J Glaucoma 14, (2005).
6 Tabatabaei, S. et al. Plateau iris: A review. Journal of Current Ophthalmology vol. 35 Preprint at https://doi.org/10.4103/joco.joco_319_22 (2023).
7 Tham, Y. C. et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology 121, (2014).
8 He, M. et al. Laser peripheral iridotomy for the prevention of angle closure: a single-centre, randomised controlled trial. The Lancet 393, (2019).
9 Fleck, B. W. How large must an iridotomy be? British Journal of Ophthalmology 74, (1990).
10 Esporcatte, B. L. B. et al. Swept-source optical coherence tomography detects anteriorchamber changes in patients with angle-closure after laser peripheral iridotomy. Arq Bras Oftalmol 87, (2024).
11 Kumar, V. M. J. Y. Z. H. C. R. K. Evaluation of Anterior Segment Parameters by using Pentacam and Gonioscopy after Prophylactic Laser Peripheral Iridotomy among primary angle close suspect. Journal of Clinical Practice 17, 12–17 (2023).
12 Gao, X. et al. Predictive Equation for Angle Opening Distance at 750 μm After Laser Peripheral Iridotomy in Primary Angle Closure Suspects. Front Med (Lausanne) 8, (2021).
13 Carassa, R. G., Bettin, P., Fiori, M. & Brancato, R. Nd:YAG laser iridotomy in pigment dispersion syndrome: An ultrasound biomicroscopic study. British Journal of Ophthalmology 82, (1998).
1Bachelor of Medicine – Ophthalmologist Head Doctor Clínica do Olho – Ophthalmology Honassys@me.com
