Frenectomia lingual em paciente pediátrico com transtorno opositivo-desafiador: relato de caso
FRENECTOMÍA LINGUAL EN UN PACIENTE PEDIÁTRICO CON TRASTORNO NEGATIVISTA DESAFIANTE: REPORTE DE UN CASO
REGISTRO DOI:10.69849/revistaft/th102410101205
Sâmara Paola Ennes Moreno[1]
Diana Fernandes de Melo[2]
Luciana Aleixo dos Santos de Melo[3]
ABSTRACT
Ankyloglossia, or “tongue-tie,” is a congenital condition that restricts tongue movement due to an abnormally short and thick lingual frenulum. This can cause difficulties with breastfeeding, chewing, swallowing, and speaking, negatively affecting social and nutritional development. The prevalence of ankyloglossia is between 4.4% and 5%, with a higher incidence in boys. Surgical treatment, such as frenectomy, may be necessary but can be challenging, especially in children with Oppositional Defiant Disorder (ODD), which is characterized by negativistic and defiant behavior. The objective of this work was to report a clinical case of lingual frenectomy in a 3-year-old pediatric patient with ODD. The patient, weighing 16 kg, presented significant difficulties with speech and feeding, and was referred by a speech therapist who suspected a shortened frenulum. Patient management involved a combined approach, including physical restraint, local anesthesia (4% articaine with epinephrine), nitrous oxide sedation, and additional sedation with intranasal midazolam (0.5 mg/kg). The procedure was successfully performed, considering the complexity of ODD and the need for adapted techniques to ensure cooperation and reduce anxiety. It is concluded that, in patients with ODD, lingual frenectomy can be effectively performed with a well-planned and individualized approach. The combination of sedation and anesthesia techniques, as described in this case, is crucial for overcoming behavioral challenges and ensuring a positive outcome in dental treatment.
Keywords: Oral Surgery; lingual frenectomy; oppositional defiant disorder; conscious sedation.
RESUMO
A anquiloglossia, ou “língua presa”, é uma condição congênita que restringe o movimento da língua devido a um frênulo lingual anormalmente curto e espesso. Isso pode causar dificuldades na amamentação, mastigação, deglutição e fala, afetando negativamente o desenvolvimento social e nutricional. A prevalência da anquiloglossia é de 4,4% a 5%, com predominância em meninos. O tratamento cirúrgico, como a frenectomia, pode ser necessário, mas é desafiador, especialmente em crianças com Transtorno Opositivo-Desafiador (TOD), caracterizado por comportamento negativista e desafiador. O objetivo deste trabalho foi relatar um caso clínico de frenectomia lingual em um paciente pediátrico de 3 anos com TOD. O paciente, com peso de 16 kg, apresentou dificuldades significativas na fala e alimentação, e foi encaminhado por um especialista em fonoaudiologia com suspeita de frênulo encurtado. O manejo do paciente envolveu uma abordagem combinada, com contenção física, anestesia local (articaína 4% com epinefrina), sedação com óxido nitroso e sedação adicional com midazolam intranasal (0,5 mg/kg). O procedimento foi realizado com sucesso, considerando a complexidade do TOD e a necessidade de técnicas adaptadas para garantir a cooperação e reduzir a ansiedade. Conclui-se que, para pacientes com TOD, a frenectomia lingual pode ser realizada eficazmente com uma abordagem planejada e personalizada. A combinação de técnicas de sedação e anestesia, conforme descrito neste caso, é fundamental para superar os desafios comportamentais e assegurar um resultado positivo no tratamento odontológico.
Palavras-chave: Cirurgia oral; frenectomia lingual; transtorno opositivo-desafiador; sedação consciente.
Resumen
La anquiloglosia, o “frenillo lingual”, es una afección congénita que restringe el movimiento de la lengua debido a un frenillo lingual anormalmente corto y grueso. Esto puede causar dificultades para amamantar, masticar, tragar y hablar, lo que afecta negativamente el desarrollo social y nutricional. La prevalencia de anquiloglosia es de 4,4% a 5%, con predominio en varones. El tratamiento quirúrgico, como la frenectomía, puede ser necesario pero desafiante, especialmente en niños con trastorno negativista desafiante (TOD), caracterizado por un comportamiento negativista y desafiante. El objetivo de este estudio fue reportar un caso clínico de frenectomía lingual en un paciente pediátrico de 3 años con TOD. El paciente, con un peso de 16 kg, presentaba importantes dificultades en el habla y la alimentación, y fue remitido por un logopedista con sospecha de frenillo acortado. El manejo del paciente implicó un abordaje combinado, con restricción física, anestesia local (4% de articaína con epinefrina), sedación con óxido nitroso y sedación adicional con midazolam intranasal (0,5 mg/kg). El procedimiento se llevó a cabo con éxito, teniendo en cuenta la complejidad del TOD y la necesidad de técnicas adaptadas para garantizar la cooperación y reducir la ansiedad. Se concluye que, para los pacientes con TOD, la frenectomía lingual se puede realizar de manera efectiva con un abordaje planificado y personalizado. La combinación de técnicas de sedación y anestesia, tal y como se describe en este caso, es esencial para superar los retos conductuales y garantizar un resultado positivo en el tratamiento dental.
Palabras clave: Cirugía oral; frenectomía lingual; trastorno negativista desafiante; Sedación consciente.
1. Introduction
Ankyloglossia, commonly known as “tongue-tie,” is a congenital condition characterized by an abnormally short and thick lingual frenulum that restricts tongue movement. The lingual frenulum is a membranous fold of mucosal tissue that connects the ventral surface of the tongue to the floor of the mouth and the basal bone of the mandible, playing a crucial role in stabilizing and limiting tongue movement. In some individuals, the frenulum fibers are attached to the tip of the tongue, restricting essential physiological movements such as protrusion, lateralization, and elevation of the tongue, potentially causing significant difficulties in functions like breastfeeding, chewing, swallowing, and speech (Mazzoni et al., 2021; Zaghi et al., 2021; Tomara et al., 2023; Dhadse et al., 2024).
The prevalence of ankyloglossia in infants ranges from 4.4% to 5%, with a male-to-female ratio of 3:1. Individuals with tongue-tie may experience difficulties with breastfeeding, delayed or impaired speech development, behavioral issues, and an increased risk of developing Class III malocclusion. These problems are exacerbated by the short and fibrotic lingual frenulum, which prevents the tongue from protruding beyond the lower incisors and affects the articulation of consonants like ‘t,’ ‘d,’ ‘n,’ and ‘l’ (Hatami et al., 2022; Komori et al., 2017).
Most frenulum abnormalities occur in the lingual frenulum or the maxillary labial frenulum. In the lingual frenulum, attachment to the tongue impairs tongue movement, leading to problems such as sucking, articulation, and speech disorders. In the maxillary labial frenulum, high attachment to the alveolar portion causes dental diastema and abnormalities in the eruption site of the central incisors. While treatment may be necessary if these symptoms are observed, it is often challenging due to difficulties in obtaining the patient’s understanding and cooperation, especially in infants or school-aged children (Dydyk et al., 2023; Tancredi et al., 2022).
Surgical correction of ankyloglossia can be performed through frenotomy, frenectomy, or frenuloplasty using a scalpel, electrocautery, or soft tissue lasers. Frenectomy, specifically, involves the complete removal of the frenulum and its attachment, allowing the restoration of tongue mobility and the resolution of associated functional problems. However, due to the anatomical location and tissue topography of the lingual area, the procedure can present intraoperative and postoperative complications, such as bleeding, infection, pain, and inadequate healing (Dell’Olio et al., 2022; Narsat et al., 2022).
In pediatric patients, particularly those with Oppositional Defiant Disorder (ODD), performing a lingual frenectomy can be even more complex. ODD is characterized by a persistent pattern of negativistic, hostile, and defiant behavior, which can make obtaining patient cooperation during treatment difficult. Resistance to dental treatment may be exacerbated by the challenging nature of the disorder, requiring a multidisciplinary approach involving pediatric dentists, psychologists, and other mental health professionals to develop effective behavioral strategies (Shumayla et al., 2023).
Techniques such as positive reinforcement, distraction, and progressive desensitization can be implemented to reduce anxiety and promote a more positive experience for the patient. The presence of a psychologist or behavioral therapist during dental appointments may be beneficial to provide additional support and guide the dental team in implementing these strategies. Moreover, clear and effective communication with the parents or guardians is vital to ensure they understand the importance of the procedure and the strategies for managing the patient’s challenging behavior (Aminabadi et al., 2016; Begnini et al., 2019).
Proper postoperative follow-up is crucial for monitoring healing and recovery, as well as identifying and managing any behavioral issues that may arise. Educating parents or guardians on how to support the patient during the recovery period is also essential for ensuring the long-term success of the treatment. Multidisciplinary treatment involving dentists and speech therapists is critical for resolving procedures like lingual frenectomy, especially in patients with complex behavioral conditions such as ODD (Jamali et al., 2021).
The aim of this paper is to report a clinical case of lingual frenectomy in a pediatric patient diagnosed with Oppositional Defiant Disorder (ODD), highlighting the challenges and strategies adopted for the successful completion of the procedure.
2. Case report
The patient, B.A.O., a 3-year-old male weighing 16 kg, attended the pediatric dentistry specialization clinic at Faculdade do Amazonas – IAES, accompanied by his mother. He had been referred by a speech therapy specialist who suspected a shortened lingual frenulum.
The mother reported that the child had significant difficulties with speech and eating, showing frustration when trying to pronounce words and avoiding certain foods, particularly those requiring extensive tongue movement. These difficulties were negatively impacting both the patient’s social and nutritional development. Additionally, the mother mentioned that the patient had already been diagnosed with ODD, which, according to her, made it challenging to manage the child in situations requiring cooperation, such as medical and dental appointments.
During the anamnesis, detailed information was gathered regarding the patient’s medical and dental history. The mother stated that the ODD diagnosis had been made by a pediatric psychiatrist and that the patient displayed defiant behaviors, such as refusing to follow instructions and becoming irritable, especially in situations involving restriction or control of his actions. No history of allergies to medications or anesthetics was identified, and the patient was not on regular controlled medications.
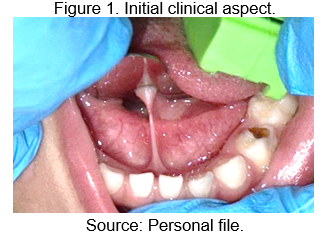
The initial clinical examination revealed that the patient had a lingual frenulum insertion that significantly restricted tongue mobility, indicating a case of ankyloglossia. Functional evaluation of the tongue showed limited elevation and projection of the tongue tip, which explained the mother’s concerns regarding the patient’s speech and feeding difficulties (Figure 1).
Given the complexity of managing the behavior of a child with ODD, a detailed meeting was held with the guardian to discuss treatment options and the necessity of performing the lingual frenectomy. It was explained that to ensure the patient’s safety and comfort, a combined approach would be required, involving physical restraint, local anesthesia, and sedation with nitrous oxide and medication. The mother was informed about the risks and benefits of the procedure and was asked to sign the Informed Consent Form (ICF), as well as authorization for the use of images for scientific and academic purposes.
On the day of the surgical procedure, the patient was prepared in a controlled environment to minimize stimuli that could trigger challenging behaviors. A team of three dental surgeons, including two specialists in pediatric dentistry, was present throughout the intervention.
During the preparation for the procedure, the patient’s vital signs were monitored, including blood pressure, which was within normal limits for his age, measuring 100/89 mmHg. The heart rate was also recorded at 80 beats per minute (bpm), indicating that the patient was in stable condition for the frenectomy.
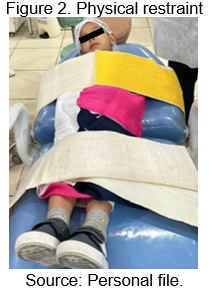
For behavioral control, a technique of moderate physical restraint was used, employing a pediatric dental chair (Macri Maca Odontopediátrica) to ensure the necessary immobilization of the patient during the administration of anesthesia and the surgical procedure (Figure 2).
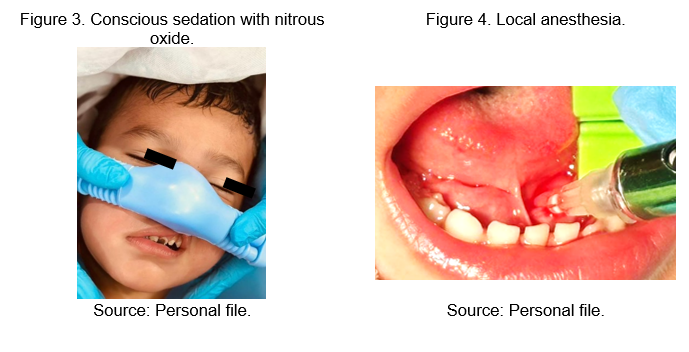
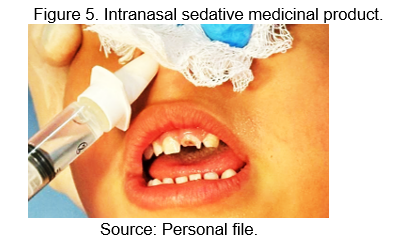
Initially, conscious sedation was performed using inhaled nitrous oxide, administered through a facial mask adapted to the patient, which helped reduce anxiety and improve behavioral control (Figure 3). Subsequently, local anesthesia was administered via a bilateral infiltrative technique of the lingual nerve using 2% Lidocaine Hydrochloride (Figure 4). Finally, midazolam was administered intranasally with a syringe for rapid absorption at a dose of 0.5 mg/kg, totaling 12.5 mg, ensuring deeper sedation and comfort during the procedure (Figure 5).
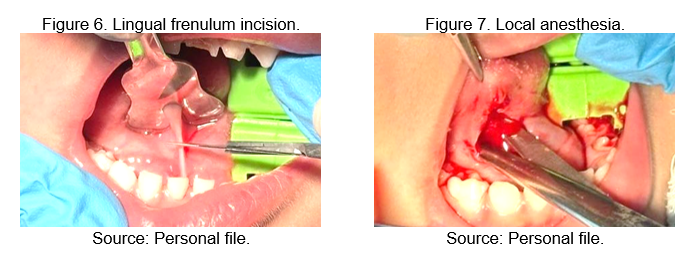
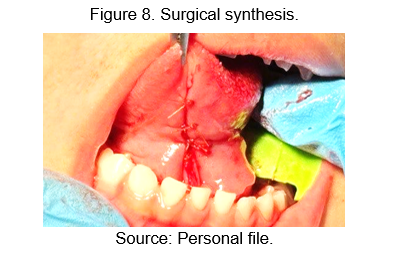
With the patient in an adequate state of conscious sedation and under physical restraint, the lingual frenectomy was initiated. After elevating the tongue, the frenulum was secured using a tissue forceps, while a linear incision was made with sterile Metzenbaum scissors, parallel to the ventral surface of the organ (Figure 6). Subsequently, tissue dilation was performed with the scissors to release the connective fibers and promote the approximation of the surgical wound edges. The entire procedure was executed under strict aseptic conditions, ensuring the integrity of the adjacent anatomical structures and adequate range of motion of the tongue after the surgery (Figure 7).
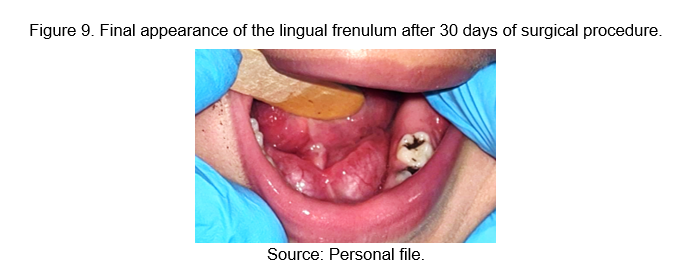
Hemostasis was controlled using gauze with direct pressure, and absorbable sutures of 4-0 Vicryl (Ethicon®) were applied in simple sutures to the sublingual mucosa, aiming to approximate the edges of the surgical wound and promote efficient healing (Figure 8).
After the procedure was completed, the patient was kept under observation until full recovery from sedation. The immediate postoperative period was monitored by the team, with special attention to potential complications such as bleeding.
The patient’s mother received detailed instructions on home care, including the need for proper oral hygiene, the use of cold compresses on the surgical area to minimize swelling, and the administration of ibuprofen 100 mg every 8 hours for three days, followed by 16 drops every 12 hours for two days. She was also advised to avoid activities that could traumatize the surgical area, such as using toys that involved sucking or intense chewing.
A follow-up appointment was scheduled for 30 days after surgery. During this visit, good healing progress was observed, with no signs of infection or dehiscence in the sutures. The mother reported that the patient showed improvement in food acceptance and that speech difficulties had begun to reduce, although continued speech therapy was necessary to enhance the results achieved (Figure 9).
It was recommended that the patient return to the pediatric dentist for regular follow-up, as well as continue speech therapy to optimize speech development and correct any possible residual articulation disorders.
3. Discussion
In recent years, there has been a significant increase in the scientific literature on lingual frenectomy and ankyloglossia, reflecting greater awareness of the importance of early diagnosis and treatment of this condition (Wei et al., 2020). Terceiro et al. (2022) discuss how early detection and appropriate intervention can improve oral development and the quality of life of patients, while Buchanan, Purnell, and Carr (2020) highlight the need for careful evaluation to determine whether intervention is truly necessary. In the reported clinical case, the decision to perform the frenectomy was based on the severity of the symptoms presented by the patient, which included significant difficulties in speech and feeding, and not merely on the presence of ankyloglossia.
Authors such as Ogundele and Morton (2022) and Reddy and Deutsch (2020) emphasize that managing patients with ODD requires an interdisciplinary approach to overcome behavioral challenges. Ogundele and Morton (2022) highlight the importance of collaboration among professionals to improve clinical outcomes, while Reddy and Deutsch (2020) stress the need for a careful approach in selecting anesthetic and sedative techniques. In the described clinical case, the team was crucial for the successful completion of the frenectomy, confirming the relevance of these approaches in clinical practice.
Elkamash and Abuohashish (2021) and Kledzik et al. (2012) agree that conscious sedation is essential for patients with ODD. Elkamash and Abuohashish (2021) discuss how behavioral disorders can complicate clinical management, and Kledzik et al. (2012) highlight the need for adapted sedation techniques to improve cooperation. The administration of nitrous oxide and intranasal midazolam in the present case followed these recommendations, helping to ensure that the patient was in an adequately sedated and comfortable state during the procedure.
López-Velasco et al. (2021) and Azevedo, Marinho, and Barreto (2020) emphasize the importance of precise surgical techniques tailored to the patient’s needs. López-Velasco et al. (2021) underline the necessity of precision in performing surgical procedures in children, while Azevedo, Marinho, and Barreto (2020) discuss adapting surgical techniques to meet the individual characteristics of patients. The choice of surgical technique in the reported case, using Metzenbaum scissors and tissue dilation, was aligned with these guidelines, contributing to an effective and satisfactory outcome.
Mayel et al. (2020) and Romero-Ruiz (2006) discuss the use of medications for postoperative pain and inflammation control. Mayel et al. (2020) report that intranasal administration of midazolam is effective for rapid sedation, while Romero-Ruiz (2006) emphasizes that controlling postoperative pain and inflammation is crucial for recovery. In the clinical case, the prescription of amoxicillin and ibuprofen proved effective in managing pain and preventing infections, aligning with existing literature.
Reddy and Deutsch (2020) and Aminabadi et al. (2016) discuss the need for special postoperative care for patients with Oppositional Defiant Disorder (ODD). Reddy and Deutsch (2020) emphasize the importance of personalized postoperative management, while Aminabadi et al. (2016) address adapting guidelines to meet individual needs. The patient’s postoperative follow-up, including instructions to avoid trauma, adhered to these recommendations, demonstrating the effectiveness of personalized strategies in managing patients with behavioral disorders.
Salam et al. (2023) and Komsic et al. (2020) agree that planning and adapting techniques are crucial for the success of dental procedures in children with behavioral disorders. Salam et al. (2023) discuss the challenges of managing patients with ODD, while Komsic et al. (2020) suggest that personalizing the procedure is essential. The reported case followed meticulous planning and technique adaptation, corroborating these observations and ensuring an effective approach.
Agarwal, Singh, and Dubey (2023) and Srinivasan et al. (2021) provide evidence on the effectiveness of anesthetic and sedative approaches in pediatric dental procedures. Agarwal, Singh, and Dubey (2023) demonstrated that intranasal midazolam in doses of 0.3-0.5 mg/kg is safe and effective for conscious sedation, with a rapid onset (5-15 minutes) and minimal complications, while Srinivasan et al. (2021) highlight that when compared to nitrous oxide sedation, intranasal midazolam was found to be equally effective in managing behavior and controlling pain, with better patient acceptance. The use of intranasal midazolam and nitrous oxide in the clinical case aligned with these guidelines, confirming the effectiveness of the described approaches.
Karam and Barakat (2011) and Lima et al. (2019) emphasize the importance of adapted strategies for postoperative care and pain control. Karam and Barakat (2011) focus on the need for tailored postoperative management for children with ODD. Reddy and Deutsch (2020) assert that understanding the specific challenges associated with ODD is crucial for anesthesiologists and other healthcare professionals to facilitate a smooth perioperative experience. In the context of this clinical case, the adaptation of anesthetic techniques and postoperative management strategies were aligned with these recommendations, allowing for the successful execution of the lingual frenectomy and minimizing the behavioral challenges associated with ODD.
4. Conclusion
Concludes that lingual frenectomy can be successfully performed in pediatric patients with ODD through a carefully planned approach tailored to the specific needs of the patient. The combination of conscious sedation techniques, using nitrous oxide and intranasal midazolam, was crucial in ensuring cooperation and reducing anxiety during the procedure, as evidenced by the literature. The experience reported in this case emphasizes the importance of personalizing treatment to overcome behavioral challenges, enabling the effective execution of complex dental procedures.
REFERENCES
AGARWAL, M.; SINGH, N.; DUBEY, B. Comparative evaluation of intranasal, buccal and oral midazolam for procedural sedation in pediatric dental patients. v. 8, p. 597–601, 2023.
AMINABADI, N. A. et al. Oral health status, dental anxiety, and behavior-management problems in children with oppositional defiant disorder. European Journal of Oral Sciences, v. 124, n. 1, p. 45–51, 2016.
AZEVEDO, A. V.; MARINHO, J. L.; BARRETO, R. C. Anquiloglossia e frenectomia: uma revisão de literatura. Brazilian Journal of Development, v. 6, n. 12, p. 98628–98635, 2020.
BEGNINI, G. J. et al. Oral health of children and adolescents with attention deficit hyperactivity disorder. International Journal of Clinical Pediatric Dentistry, v. 12, n. 6, p. 543, 2019.
BUCHANAN, T.; PURNELL, P.; CARR, M. Oral frenula in newborns: when should you refer for evaluation and intervention?. West Virginia Medical Journal, v. 116, 2020.
DELL’OLIO, F. et al. Lingual laser frenotomy in newborns with ankyloglossia: a prospective cohort study. Italian Journal of Pediatrics, v. 48, n. 1, p. 163, 2022.
DHADSE, P. V et al. Laser-assisted lingual frenectomy: a case report. Cureus, v. 16, n. 4, 2024.
DYDYK, A. et al. Influence of shortened tongue frenulum on tongue mobility, speech and occlusion. Journal of Clinical Medicine, v. 12, n. 23, 2023.
ELKAMASH, H. M.; ABUOHASHISH, H. M. The behavior of patients with obsessive-compulsive disorder in dental clinics. International journal of dentistry, Egypt, v. 2021, p. 5561690, 2021.
HATAMI, A. et al. Effectiveness of tongue‐tie assessment tools in diagnosing and fulfilling lingual frenectomy criteria: a systematic review. Australian Dental Journal, v. 67, n. 3, p. 212, 2022.
JAMALI, Z. et al. Oral health status and oral health-related quality of life in children with attention-deficit hyperactivity disorder and oppositional defiant disorder. Special Care in Dentistry, v. 41, n. 2, p. 178–186, 2021.
KARAM, V. Y.; BARAKAT, H. Perioperative management of the child with behavioral disorders. Middle East Journal of Anaesthesiology, Lebanon, v. 21, n. 2, p. 191–197, 2011.
KLEDZIK, A. M. et al. Challenges in treating oppositional defiant disorder in a pediatric medical setting: a case study. Journal of Pediatric Nursing, United States, v. 27, n. 5, p. 557–562, 2012.
KOMORI, S. et al. Clinical study of laser treatment for frenectomy of pediatric patients. International Journal of Clinical Pediatric Dentistry, v. 10, n. 3, p. 272, 2017.
KOMSIC, J. et al. Various techniques of adaptation to dental treatment of children with autism spectrum disorder. Med Pregl, v. LXXIII, p. 375–379, 2020.
LÓPEZ-VELASCO, A. et al. General anesthesia for oral and dental care in paediatric patients with special needs: A systematic review. Journal of clinical and experimental dentistry, Spain, v. 13, n. 3, p. e303–e312, 2021.
MAYEL, M. et al. Intranasal midazolam sedation as an effective sedation route in pediatric patients for radiologic imaging in the emergency ward: A single-blind randomized trial. Turkish Journal of Emergency Medicine, India, v. 20, n. 4, p. 168–174, 2020.
MAZZONI, A. et al. Protocol: Evaluation of the effects of high-level laser and electrocautery in lingual frenectomy surgeries in infants: protocol for a blinded randomised controlled clinical trial. BMJ Open, v. 11, n. 11, p. 50733, 2021.
NARSAT, M. A. et al. Grouping of ankyloglossia according to coryllos anatomical classification and follow-up results for breastfeeding: single-center, cross-sectional study. Children, v. 9, n. 12, 2022.
OGUNDELE, M. O.; MORTON, M. Classification, prevalence and integrated care for neurodevelopmental and child mental health disorders: A brief overview for paediatricians. World Journal of Clinical Pediatrics, United States, v. 11, n. 2, p. 120–135, 2022.
REDDY, S. K.; DEUTSCH, N. Behavioral and Emotional Disorders in Children and Their Anesthetic Implications. Children (Basel, Switzerland), Switzerland, v. 7, n. 12, 2020.
ROMERO-RUIZ MM et al. Protocolo de control del dolor y la inflamación postquirúrgica. Una aproximación racional Postoperative pain and swelling treatment protocol. A rational approach. Rcoe, v. 11, n. 2, p. 205–215, 2006.
SALAM T A, A. et al. Management of attention-deficit hyperactivity disorder children for dental procedures. Cureus, United States, v. 15, n. 4, p. e36989, 2023.
SHUMAYLA, K. et al. A case report on dental management of a child with attention deficit hyperactivity disorder. 2023.
SRINIVASAN, N. K. et al. Comparison of the sedative effect of inhaled nitrous oxide and intranasal midazolam in behavior management and pain perception of pediatric patients: a split-mouth randomized controlled clinical trial. International Journal of Clinical Pediatric Dentistry, India, v. 14, n. Suppl 2, p. S111–S116, 2021.
TANCREDI, S. et al. Clinical comparison of diode laser assisted “v-shape frenectomy” and conventional surgical method as treatment of ankyloglossia. Healthcare, v. 10, n. 1, 2022.
TERCEIRO, Laríssia Honório et al. Impacto da frenectomia lingual na qualidade de vida de bebês e seus pais. Revista da Faculdade Paulo Picanço, v. 2, n. 1 SE-, p. 8, 2022.
TOMARA, E. et al. Ankyloglossia as a barrier to breastfeeding: a literature review. Children, v. 10, n. 12, 2023.
WEI, E. X. et al. Ankyloglossia: Update on Trends in Diagnosis and Management in the United States, 2012-2016. Otolaryngology Head and Neck Surgery, England, v. 163, n. 5, p. 1029–1031, 2020.
ZAGHI, S. et al. Assessment of posterior tongue mobility using lingual‐palatal suction: Progress towards a functional definition of ankyloglossia. Journal of Oral Rehabilitation, v. 48, n. 6, p. 692, 2021.
[1]Specialist in Pediatric Dentistry. Faculdade do Amazonas (IAES). Manaus, Amazonas, Brazil. Email: drasamaramoreno@gmail.com
[2]Specialist in Pediatric Dentistry. Faculdade do Amazonas (IAES). Manaus, Amazonas, Brazil. Email: dra.dianamelo@gmail.com
[3]PhD in Pharmaceutical Innovation. Federal University of Amazonas (UFAM). Manaus, Amazonas, Brazil. E-mail: meloaleixoluciana@hotmail.com
