REGISTRO DOI: 10.69849/revistaft/fa10202001081539
Leonardo Dornelas Alves
ABSTRACT
The external hexagon implant is widely utilized in dentistry as a support for dental prostheses, characterized by its hexagonal platform that connects to the prosthetic abutment. Its key advantages include ease of handling due to its hexagonal design, which facilitates placement and adjustment during surgical and prosthetic phases. Additionally, being one of the earliest developed implant systems, it boasts broad compatibility with various components and brands, allowing for a wider range of prosthetic elements, which helps reduce costs and simplifies maintenance. Its stability under axial loads makes it effective in areas with lower lateral stress, particularly in fixed prostheses or complete arches. However, the external hexagon implant has notable limitations, primarily its lower resistance to lateral forces compared to internal connections, which can lead to micro-movements and increase the risk of component failures and bone loss around the implant. The external connection also poses a greater risk of screw loosening, necessitating frequent adjustments, which can be inconvenient for patients. Additionally, the potential formation of microgaps between the implant and abutment can facilitate bacterial infiltration, causing inflammation and jeopardizing the long-term health of the implant. Aesthetic considerations also come into play, as the external hexagon may not be ideal for visible areas due to potential bone resorption affecting the appearance of surrounding gum tissue. Recent studies have explored various design aspects and their impact on mechanical resistance, emphasizing the need for careful analysis of clinical and biomechanical factors when selecting this type of connection. Thus, while the external hexagon implant is a practical option in specific scenarios, its use should be weighed against alternative connection designs to ensure optimal treatment outcomes.
Keywords: External hexagon implant; Dental prostheses; Mechanical resistance; Bone loss; Aesthetic considerations.
The external hexagon implant, often referred to as the “external hexagon,” is widely used in dentistry as a support for dental prostheses. This type of implant is characterized by the presence of a hexagonal platform at its end, which connects to the prosthetic abutment. Although it has significant advantages, it also has limitations that must be considered when choosing the most suitable implant for each case.
One of the main advantages of the external hexagon implant is its ease of handling. The hexagonal configuration of the platform simplifies the placement and adjustment of the abutment during surgery and the prosthetic phase, making the process more efficient and accessible for the dentist. Additionally, since it was one of the first implant systems developed, it is widely compatible with various components and brands, allowing professionals to use a broader range of prosthetic elements, reducing costs and facilitating the maintenance of the implant. Another positive aspect is its stability under axial loads, making it effective in regions with lower lateral stress or in cases of connected multiple implants, such as in fixed prostheses or complete arches.
On the other hand, the external hexagon implant has relevant disadvantages. Its main limitation is its lower resistance to lateral loads, as the external connection does not provide the same fit as the internal one. This can lead to micro-movements, increasing the risk of component failure and bone loss around the implant (bone resorption). Furthermore, this type of connection presents a higher risk of screw loosening, requiring frequent adjustments and checks, which can be inconvenient for the patient and increase the need for maintenance.
Another issue is the possibility of microgap formation, which are small spaces between the implant and the abutment. These microgaps can facilitate bacterial infiltration and cause inflammation in the adjacent tissues, compromising the long-term health of the implant. Aesthetically, the external hexagon may not be the best choice for visible areas, such as the anterior region, as its configuration can lead to greater bone resorption, altering the appearance of the gums around the implant.
Figure 1: Implant connection types.
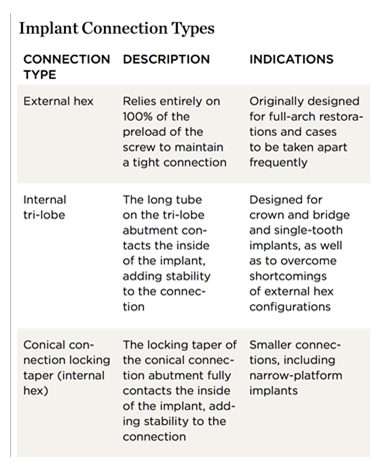
Source: Hurson (2016).
Thus, the external hexagon implant represents a practical and effective solution in certain scenarios, especially in extensive rehabilitations and complete arches. However, the decision to use it should consider the location, aesthetic needs, and functional requirements of each case. In some situations, other connection options may be more advantageous, particularly in areas where resistance to lateral forces and aesthetic preservation are crucial.
Several studies have explored aspects of the design and properties of implant-abutment connectors. Ribeiro et al. (2011) investigated how these characteristics affect the mechanical resistance of implants by comparing external hexagon, internal hexagon, and cone-in-cone interfaces. The study used a cantilever beam test to simulate multivectorial intraoral loading, determining the force levels at which 50% of the samples withstood one million load cycles. The results showed that the external hexagon interface performed better compared to the other types, while the internal interfaces did not show significant advantages in terms of strength.
In turn, the study by Gil et al. (2009) assessed the impact of the height of the external hexagon and surface treatments applied on the fatigue life of titanium dental implants. Electropolished titanium implants, with three heights of external hexagon (0.6, 1.2, and 1.8 mm), were tested with different surface treatments. Tests conducted in artificial saliva at 37 °C showed that the height of 1.8 mm significantly increased the fatigue life, while the aluminum oxide blasting treatment provided the highest durability among the materials analyzed.
The study by Pessoa et al. (2017) aimed to evaluate clinical, radiographic, microbiological, and biomechanical parameters related to bone remodeling in implants with external hexagon (EH) and Morse taper (MT) connections. Involving twelve edentulous patients who received four custom implants in the interforaminal region of the mandible, the research compared implants with the same macroscopic design but different prosthetic connections. Radiographic analysis demonstrated significant differences in bone loss around the implants, with an average bone contact distance of 1.17 ± 0.44 mm for EH and 0.17 ± 0.54 mm for MT. Finite element analysis revealed that EH connections had a significantly higher peak deformation compared to MT connections.
Similarly, the study by Almeida et al. (2014) analyzed stress distribution in the bone tissue around implants with variable angulations (0°, 17°, and 30°) and connection types (external hexagon and conical). The results showed that under oblique load, the external hexagon connection induced significantly higher stress concentrations in the bone tissue compared to the conical connection.
Finally, the study by Menini et al. (2019) evaluated whether the morphology of implant-abutment connections—specifically internal designs versus external hexagons—affects the behavior of peri-implant tissues. After 12 months of follow-up, no significant differences were found between the connections regarding marginal bone loss or periodontal health indicators, suggesting that both types offer reliable clinical outcomes.
Overall, the literature highlights the effectiveness and applicability of the external hexagon implant but also emphasizes the importance of careful analysis of clinical and biomechanical factors when opting for this type of connection.
In summary, the external hexagon implant stands out as a widely used and practical solution in dental prosthetics, offering notable advantages such as ease of handling, broad compatibility with various components, and stability under axial loads. However, it also presents significant limitations, particularly regarding its resistance to lateral forces, the risk of screw loosening, and potential issues with microgap formation, which can affect the long-term success of the implant.
The decision to use an external hexagon implant should be made with careful consideration of the specific clinical scenario, including factors such as the location of the implant, aesthetic demands, and functional requirements. Additionally, recent studies indicate that while the external hexagon offers reliable mechanical performance, it may not always be the best choice in situations where lateral stress resistance and aesthetic preservation are paramount.
Ultimately, ongoing research and advancements in implant design continue to inform best practices in implant dentistry, enabling practitioners to make more informed decisions tailored to the needs of individual patients. By weighing the pros and cons of the external hexagon implant against alternative connection options, dental professionals can optimize treatment outcomes and enhance the overall success of implant-supported rehabilitations.
REFERENCES
Almeida, D., Pellizzer, E., Verri, F., Santiago, J., & Carvalho, P. (2014). Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: three-dimensional finite element method with statistical analysis.. Journal of periodontology, 85 2, 261-9 . https://doi.org/10.1902/jop.2013.120713.
Gil, F., Aparicio, C., Manero, J., & Padrós, A. (2009). Influence of the height of the external hexagon and surface treatment on fatigue life of commercially pure titanium dental implants.. The International journal of oral & maxillofacial implants, 24 4, 583-90.
Hurson, S. (2016). Use of Authentic, Integrated Dental Implant Components Vital to Predictability and Successful Long-Term Clinical Outcomes. Compendium of Continuing Education in Dentistry (Jamesburg, NJ: 1995), 37(7), 450-455.
Melo, L., Souza, M., Barbosa, G., & Carreiro, A. (2017). Peri-Implant Bone Loss of External Hexagon and Morse Taper in Patients Wearing Immediately Loaded Overdentures.. Brazilian dental journal, 28 6, 694-698. https://doi.org/10.1590/0103-6440201701577.
Menini, M., Pesce, P., Bagnasco, F., Carossa, M., Mussano, F., & Pera, F. (2019). Evaluation of internal and external hexagon connections in immediately loaded full-arch rehabilitations: A within-person randomised split-mouth controlled trial.. International journal of oral implantology, 12 2, 169-179 .
Pessoa, R., Sousa, R., Pereira, L., Neves, F., Bezerra, F., Jaecques, S., Sloten, J., Quirynen, M., Teughels, W., & Spin‐Neto, R. (2017). Bone Remodeling Around Implants with External Hexagon and Morse‐Taper Connections: A Randomized, Controlled, Split‐Mouth, Clinical Trial. Clinical Implant Dentistry and Related Research, 19, 97–110. https://doi.org/10.1111/cid.12437.
Ribeiro, C., Maia, M., Scherrer, S., Cardoso, A., & Wiskott, H. (2011). Resistance of three implant-abutment interfaces to fatigue testing. Journal of Applied Oral Science, 19, 413 – 420. https://doi.org/10.1590/S1678-77572011005000018.
