REGISTRO DOI: 10.5281/zenodo.11263604
Phamela de Freitas Geraldo Antunes¹; Daniel Antunes Pereira²; Vinícius Freitas Bastos³; Maria Clara Arca Peixoto4; Cássia Santos de Lima Menezes5; Diego de Lima Moura6; Antônio Carlos de Freitas da Silva7; Monique José de Souza Chagas8; Yasmin Faria Menezes Castro Santos9; Amanda Menescal Sias Lins10; Isaías Leite de Almeida Esteves¹¹.
ABASTRACT
This case of a 53-year-old male (MAC) diagnosed with mild hemophilia B, who presented with dysarthria, myalgia, and vomiting over four days. Initial computed tomography on 24/02/2024 revealed intraparenchymal hemorrhage with midline shift, prompting conservative treatment under neurosurgical care. Factor IX replacement therapy commenced immediately on 24/02/2024, with rigorous monitoring to ensure adequate cerebral perfusion. Despite observed hemorrhage area increase during follow-up on 26/02/2024, the patient remained neurologically intact. Continuous factor IX replacement per protocol, with adjustments in antihypertensive therapy and glycemic control, sustained stability, evidenced by subsequent CT scans on 02/03/2024 showing no further hemorrhage progression. The case underscores the critical role of multidisciplinary collaboration among neurosurgery, intensive care, and hematology in optimizing outcomes for hemophiliac patients with severe hemorrhagic complications. Monitoring hematoma evolution through frequent imaging and meticulous therapeutic adjustments are crucial aspects of this comprehensive approach. In conclusion, this case report emphasizes the successful management of ICH in hemophilia B, reinforcing the need for personalized protocols and continuous surveillance to navigate bleeding control and thrombotic risk effectively. Future advancements in hemophilia management, including gene therapy and extended half-life factor replacements, hold promise for further enhancing outcomes and quality of life for these patients.
Keywords: Hemophilia B, Intracranial Hemorrhages, factor IX.1
INTRODUCTION
In Brazil, the prevalence of hemophilia A is 1 in 10,000 males, while hemophilia B affects approximately 0.7 in 35,000 males. From 1999 to 2016, a total of 927 male deaths related to hemophilia were recorded, with 45.1% of these deaths having hemophilia as the underlying cause and 54.9% as an associated cause. The leading cause associated with deaths where hemophilia was the underlying cause was hemorrhage, particularly intracranial hemorrhage (ICH), which poses a significant challenge due to its high mortality and morbidity rates. ICH is especially prevalent among hemophiliacs, with an incidence of 2.2% to 7.7%, which is at least 20 times higher than in the general male population. Risk factors include severe disease, on-demand treatment, presence of inhibitors, and cranial trauma(DE CRISTOFARO; FRANCHINI, 2019; DIRINGER et al., 2008; SANTO, 2021).
In children with hemophilia, ICH can occur spontaneously or as a result of unwitnessed trauma, making it difficult to assess its exact prevalence. Literature reviews indicate that most cases of ICH in hemophilic children occur in those with severe hemophilia A, with a median age of 2 years. Symptoms of ICH in children can be nonspecific, with alterations in consciousness and headache being the most frequent. In children under 2 years old, symptoms such as seizures, pallor, bulging fontanelle, vomiting, and irritability are common. In older children, headache, alterations in consciousness, and neurological deficits are predominant. Early identification and proper management are crucial to minimize adverse consequences of ICH in these patients(LJUNG; MATINO; SHAPIRO, 2024; ROHAERT; LABARQUE, 2021).
Treatment of hemophilia B has significantly evolved in recent years with the introduction of extended half-life factor IX (FIX) replacement products. These products, such as rFIXFc, a recombinant fusion protein with extended circulation time, provide effective protection against bleeding with less frequent administrations, improving quality of life for patients. rFIXFc has a biodistribution profile that supports hemostasis at vascular injury sites regardless of activity levels(CHO et al., 2016; CHOU; HSU; LIN, 2023; DIRINGER et al., 2008; LJUNG; MATINO; SHAPIRO, 2024).
Spontaneous intracranial hemorrhage is a rare complication of hemophilia, occurring at a frequency of 2.2% to 7.8% with a mortality rate of 34%. This condition is potentially fatal and requires emergent neurosurgical intervention. Small hemorrhages without significant mass effect can be managed conservatively with factor VIII concentrate and rigorous neurological monitoring. However, larger hemorrhages require surgery under factor VIII coverage. A specific case successfully converted an acute subdural hematoma into a chronic one using decongestants and factor VIII concentrate, thereby avoiding the need for craniotomy and significantly reducing the risk of re-bleeding. Intensive factor VIII management followed guidelines from the World Federation of Hemophilia, with precisely calculated doses to maintain therapeutic levels during the perioperative period, demonstrating favorable functional outcomes with a Glasgow score of 5(FERNANDES et al., 2021; OLDENBURG et al., 2023).
In contrast, significant advances in gene therapy for hemophilia B were achieved in 2011 by Nathwani et al. This pioneering study used an AAV vector with hepatic tropism to deliver and sustain expression of the F9 gene in patients, raising factor IX levels up to 6%. Optimized self-complementary DNA constructs improved expression efficiency, allowing for a single non-invasive intravenous infusion rather than intrahepatic injections. However, sustained expression was challenged by immune clearance of transduced hepatocytes, mitigated in this study by using steroids to suppress the immune response. These advances offer promising prospects for future treatments of hemophilia B, potentially radically altering the management of this chronic condition(FERNANDES et al., 2021; LJUNG; MATINO; SHAPIRO, 2024; ROCINO; FRANCHINI; COPPOLA, 2017).
This case report aims to discuss a case of ICH in a patient with hemophilia B managed conservatively by neurosurgery and therapeutic management with factor IX replacement, resulting in a good outcome.
CASE REPORT
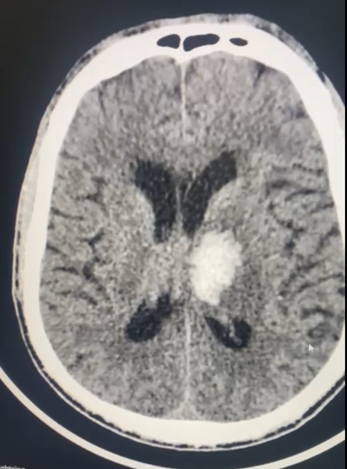
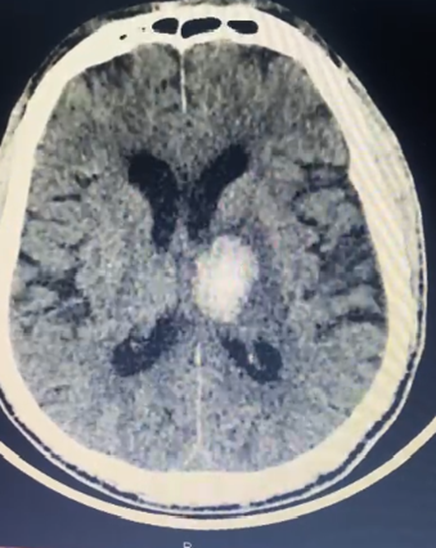
MAC, male, 53 years old, diagnosed with mild hemophilia B, presented with a clinical picture evolving over four days characterized by dysarthria, myalgia, and vomiting. Following initial evaluation and a computed tomography scan on 24/02/2024, he was diagnosed with intraparenchymal hemorrhage with midline shift, conservatively treated by the neurosurgical team (Figure 1). Factor IX replacement therapy was initiated on 24/02, and he was kept under rigorous monitoring, highlighting compensatory hypertension to ensure adequate cerebral perfusion. NIHSS 5, previously in good health, GLASGOW 15, disoriented and without neurological deficit, Aplastic anemia, chronic kidney disease, started nipride and Dexamethasone and rigorous glycemic monitoring. Despite increased hemorrhagic area observed on follow-up CT on 26/02, the patient remained oriented, without significant neurological deficits. In subsequent follow-up, the patient continued to receive factor IX replacement per protocol, with adjustments in antihypertensive therapy and glycemic control. CT scan on 02/03 showed no further increase in hemorrhage, indicating stability (Figure 2). Management was reassessed in conjunction with intensive care and hematology, emphasizing the importance of clinical and radiological vigilance, especially in the face of any neurological deterioration.
Finally, after 10 days of factor IX replacement and stabilization of clinical condition, the patient demonstrated a good overall and neurological outcome.
DISCUSSION
Intracerebral hemorrhage (ICH) is a rare but severe complication of hemophilia, affecting between 2.2% to 7.7% of patients with the condition, a significantly higher incidence than in the general population. In the case of the 53-year-old patient with mild hemophilia B, the presentation of ICH with midline shift required careful management due to its complexity. The initial conservative approach with factor IX replacement was crucial, given the need to stabilize hemorrhage without resorting to immediate invasive procedures, reflecting management guidelines for hemophiliac patients with intracranial hemorrhages(HEGDE; NAIR; UPADHYAYA, 2016; ROHAERT; LABARQUE, 2021).
Case reports and previous studies indicate that while factor IX administration may reduce hematoma expansion and improve outcomes in ICH cases in hemophilia B, there is an associated increased risk of arterial thromboembolic events, especially at higher doses. This risk is particularly relevant in older patients with a higher prevalence of atherosclerosis and reduced mobility, such as the patient in question. Therefore, the decision for conservative management with factor IX may have been influenced by the balance between hemostatic efficacy and the risk of thromboembolic complications.
In neonates and children with hemophilia, the incidence of ICH is high in the first few days of life, with high mortality. In adults, risk factors for ICH include hypertension, presence of inhibitors, infections such as HIV and hepatitis C, and inadequate adherence to prophylaxis. In the discussed patient, arterial hypertension was managed with nitroprusside, maintaining blood pressure at controlled levels to minimize the risk of re-bleeding, while factor IX replacement was carefully adjusted to ensure adequate therapeutic levels(BADESCU et al., 2022; LJUNG; MATINO; SHAPIRO, 2024).
The literature suggests that intensive and personalized management of ICH in hemophiliacs is crucial to prevent adverse outcomes. Frequent imaging such as CT scans allowed monitoring of hematoma evolution and adjustment of therapy as needed. Maintenance of factor IX replacement and continuous monitoring of renal function and glucose levels demonstrate the need for a rigorous multidisciplinary approach(HEGDE; NAIR; UPADHYAYA, 2016; LJUNG; MATINO; SHAPIRO, 2024; SANTO, 2021).
CONCLUSION
This patient’s case illustrates the complexity of managing ICH in hemophiliacs, highlighting the importance of an approach that balances hemorrhage control with prevention of thromboembolic complications. Success in stabilizing the hemorrhagic condition without significant hematoma increase until 02/03, coupled with the absence of neurological deficits, reflects the effectiveness of the adopted management. This report reinforces the need for personalized protocols and continuous surveillance to optimize outcomes in patients with hemophilia and severe hemorrhagic complications.
REFERENCES
BADESCU, M. C. et al. Current Therapeutic Approach to Atrial Fibrillation in Patients with Congenital Hemophilia. Journal of personalized medicine, v. 12, n. 4, 1 abr. 2022.
CHO, J. Y. et al. Clinical Characteristics and Prognostic Factors in Hemophiliacs with Intracranial Hemorrhage: A Single-Center, Retrospective Experience. Indian journal of hematology & blood transfusion : an official journal of Indian Society of Hematology and Blood Transfusion, v. 32, n. 4, p. 488–493, 1 dez. 2016.
CHOU, S. C.; HSU, Y. C.; LIN, S. W. Gene therapy for hemophilia, a clinical viewpoint. Journal of the Formosan Medical Association = Taiwan yi zhi, v. 122, n. 11, p. 1101–1110, 1 nov. 2023.
DE CRISTOFARO, R.; FRANCHINI, M. Intracranial haemorrhage in children and adults with haemophilia A and B: a literature review of the last 20 years. Blood transfusion = Trasfusione del sangue, v. 17, n. 5, p. 334–335, 2019.
DIRINGER, M. N. et al. Risk of thromboembolic events in controlled trials of rFVIIa in spontaneous intracerebral hemorrhage. Stroke, v. 39, n. 3, p. 850–856, mar. 2008.
FERNANDES, J. M. A. et al. Factor VIII prophylactic therapy reduces neurological complications in patients with Hemophilia A. Arquivos de neuro-psiquiatria, v. 79, n. 12, p. 1116–1122, 1 dez. 2021.
HEGDE, A.; NAIR, R.; UPADHYAYA, S. Spontaneous intracerebral hemorrhage in hemophiliacs-A treatment dilemma. International journal of surgery case reports, v. 29, p. 17–19, 2016.
LJUNG, R.; MATINO, D.; SHAPIRO, A. D. Recombinant factor IX Fc for the treatment of hemophilia B. European journal of haematology, v. 112, n. 5, p. 678–691, 1 maio 2024.
OLDENBURG, J. et al. Clinical experience of switching patients with severe hemophilia to rVIII-SingleChain or rIX-FP. Current medical research and opinion, v. 39, n. 2, p. 219–225, 2023.
ROCINO, A.; FRANCHINI, M.; COPPOLA, A. Treatment and Prevention of Bleeds in Haemophilia Patients with Inhibitors to Factor VIII/IX. Journal of clinical medicine, v. 6, n. 4, 1 abr. 2017.
ROHAERT, C.; LABARQUE, V. Spontaneous intracranial haemorrhage as initial presentation of haemophilia in infants and children: A case report and systematic literature review. Haemophilia : the official journal of the World Federation of Hemophilia, v. 27, n. 3, p. e398–e401, 1 maio 2021.
SANTO, A. H. Causes of death and mortality trends related to hemophilia in Brazil, 1999 to 2016. Hematology, transfusion and cell therapy, v. 43, n. 2, p. 171–178, 1 abr. 2021.
¹Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: phamellafreitas@hotmail.com
²Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: danielantunespi@gmail.com
³Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: vinicius.freitas16@icloud.com
4Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: maria.arcapeixoto@gmail.com
5Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: cassiasantosdelimamenezes@gmail.com
6Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: ddelimamoura@gmail.com
7Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: antoniofreitascff@gmail.com
8Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: moniqjsc@gmail.com
9Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: yasminfaria@gmail.com
10Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: amandasias@gmail.com
¹¹Discente do Curso Superior de Medicina da Universidade Iguaçu Campus Nova Iguaçu e-mail: isaias.esteves1702@gmail.com
