REGISTRO DOI: 10.69849/revistaft/ni10202410121519
Natália Balbo Arantes Nogueira1; Larissa Tarraf Bertazzo1; Isadora Vergamini Lamana1; Ana Carolina Gomes de Oliveira1; Daniele Costa de Sousa3; Bruno de Paula Lima3; Júlio César Claudino dos Santos2
Abstract
Autism spectrum disorder (ASD) is described by resistant deficits in social interaction and language, such as limited and repetitive habits and interests, so that it is characterized as a complex behavioral disorder that begins in early childhood and extends throughout life. The aim of our study was to explore the current literature on non-pharmacological treatments and their consequent effectiveness in ASD. Based on this, a narrative review of the literature was carried out in order to understand the impact of each non-drug treatment in reducing the core symptoms associated with the disorder. We therefore highlight the importance of non-pharmacological interventions as adjuvant strategies in the treatment of individuals with this neurodevelopmental condition.
Key words: autism spectrum disorder; non-pharmacological treatment; neurodevelopmental disorder.
Introduction
Autism spectrum disorder (ASD) is described by resistant deficits in social interaction and language, such as limited and repetitive habits and interests (Cheng, N et al., 2017), so that it is characterized as a complex behavioral disorder that begins during early childhood and extends throughout life (Chakrabarti, B et al., 2015).
In individuals with ASD there is an extensive spectrum of symptoms and levels of impairment, comprising central behavioral symptoms and the gastrointestinal, immune, hepatic and endocrine systems (Cheng, N et al 2017). Common comorbidities can be exaggerated responses to sounds and textures, attraction to lights and spinning objects. In addition to neurological deficits such as seizures, sleep disorders, and among the uncommon ones are anxiety disorders, obsessive-compulsive disorders and depression (Chakrabarti, B et al., 2015).
Based on the current DSM 5 criteria (APA, 2013), autism contains three levels of severity, which are characterized from “requiring support” to “requiring very substantial support”. The definition of severity is defined only by the two central domains: social communication and restricted or repetitive patterns of behavior. They are specified as, level 1, “without supports in place, deficits in social communication cause noticeable impairment”; level 2 “severe deficits in verbal and non-verbal social communication skills, social impairment apparent even with supports in place”; and level 3, “severe deficits in verbal and non-verbal social communication skills cause serious impairment in functioning”. Respectively, the levels of support are “requiring support”, “requiring substantial support” and “requiring very substantial support” (Waizbard-Bartov, E et al., 2023; APA,2013).
Two decades have passed with major funding for ASD intervention research, and not much pharmacological progress has been made for central deficits. However, there has been a modest advance in the treatment of associated symptoms, but they are still insufficient to grant independence to the adult (McCracken, J. T et al., 2021). Medications such as risperidone and aripiprazole, as well as atypical antipsychotics, have been used to treat irritability and aggression in ASD. In addition to these, there have been studies on oxytocin in social interaction and repetitive restricted behaviors. Bumetanide also showed a reduction in repetitive behaviors and an improvement in the emotional perception of the face was observed in ASD. Despite this, no drug treatment has shown significant clinical advantages (Tian, J et al., 2022).
As for non-pharmacological treatment, psychotherapeutic approaches are those of first choice, such as the metaverse-based social skills training program, which improved social interaction skills and reduced emotional problems in children with ASD (Lee, J.H et al., 2023). In addition, mindfulness has been applied to patients with ASD, and there is evidence suggesting it has the potential to reduce depression and anxiety in these individuals (White, S et al., 2018). There are other alternatives, metabolic therapy, i.e. a ketogenic diet, high in fat and low in carbohydrates that induces neuroprotective effects and reduces comorbidities associated with ASD (Cheng, N et al., 2017).
In this sense, according to the information provided in this introduction and given the importance of non-pharmacological treatment, since pharmacological interventions have not achieved significant success, a more detailed study on the subject is indispensable. Therefore, this article seeks to deepen the connection between ASD and non-pharmacological treatment and how they have a bidirectional relationship with each other, for an improvement in the quality of life of individuals with ASD.
Method
A narrative literature review was executed in the medline database (pubmed) and in the Cochrane, from 2014 to 2024, about the role of non-pharmacological treatment strategies for autism spectrum disorder (ASD). In the medline database (pubmed), 170 articles were found through the mesh descriptor “(((Autism Spectrum Disorder[Text Word]) AND (Autism Spectrum Disorder[Title/Abstract])) AND (Therapeutics[Title/Abstract])) AND (Therapeutics[Text Word])” of which 162 were included, after the exclusion of articles following the first set of criteria – exclusion of titles that did not address the role of non-pharmacological treatment strategies for autism spectrum disorder, articles not included in the research period of 2014-2024, as well as articles that were not originally in english. After this phase, a second set of criteria was applied – exclusion of the abstracts that did not address the role of non-pharmacological treatment strategies for autism spectrum disorder (ASD), which led to the exclusion of 13 articles. After the selection, 4 new articles were manually selected and added, according to their relevance to the study. Finally, aiming to enrich the discussion, 17 articles originally in English were manually selected and added according to their relevance in the synthesis of qualitative evidence.
Discussion
After analyzing the literature and updating the current state of the art on non-pharmacological strategies for autism spectrum disorder, we reviewed the results of intervention strategies such as cognitive behavioral therapy, metaverse social skills training, the ketogenic diet, subtractive therapy, bacteriocins, bacteriophages, additive therapy, melatonin, cannabis-based medicines, equine therapy and fecal microbial transplantation and their evidence and repercussions on the main symptoms of ASD.
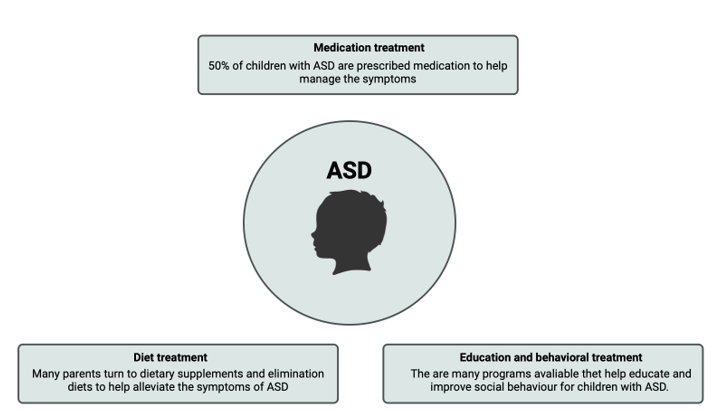
Figure 01. Modalities of interventions in autism spectrum disorder.
Anxiety disorders are the most common mental health condition in children and adolescents with ASD. Cognitive-behavioral therapy, which comprises exposure, modeling and parental involvement, has been found to be a well-established evidence-based treatment for anxiety disorders. In addition, they are four times more likely to develop depression in their lifetimes, according to a meta-analytical review. Among adolescents, cognitive-behavioral therapy and interpersonal therapy have been well-established in evidence-based treatments for depression with medium effect results (White, S. W et al., 2018).
An open, single-center, randomized controlled pilot trial was carried out based on a metaverse social skills training program to advance social interaction in children aged 7 to 12. The program implemented PEERS within the metaverse platform and involved 4 sessions of didactic lessons on social skills and mindfulness from a therapist. In view of this, promising results were obtained in relation to social responsiveness, mental health, social adaptation and emotional and behavioral problems (Lee, J. H et al., 2023).
Neurotechnology, i.e. technology that interacts with the human central nervous system, can be used to influence human thought or perception. This bringing together of thought and technology is at the heart of brain-computer interface (BCI) devices. This allows for social interaction, and because it is virtual, it can be less stressful and more controllable. Despite this, the benefits of these neurotechnology approaches still need to be tested in randomized clinical trials compared to other interventions (Damiano, C. R et al., 2014).
To date, limited clinical trials have been carried out on the treatment of ASD patients with metabolic therapy applying a ketogenic diet. However, according to a pilot study, there was satisfactory progress based on the Childhood Autism Rating Scale (CARS). In addition, the diet was effective in reducing ASD comorbidities, such as seizures, and showed improvement in cognition and behavior, especially anxiety disorders (Cheng, N et al., 2017).
Studies coordinated by McMaster University have suggested that dysbiosis of the intestinal microbiota favors the development of neurobehavioral disorders. Studies have found strong links between the gut microbiome and ASD. The use of antibiotics from birth to around 3 years of age can impair the development of the human microbiome, thus crucially affecting the maturation of the immune system, which can lead to infections, inflammation, allergies and gastrointestinal diseases. In addition, the excessive use of antibiotics leads to dysbiosis of the intestinal microbiome and can activate the autism gene. However, there is subtractive therapy, bacteriocins and bacteriophages which are used to combat pathogens in various ways: releasing toxins, interrupting respiratory mechanisms, disintegrating the membrane and cell death, without harming other microbes in the ecosystem. This is a more favorable alternative to the use of antibiotics. Furthermore, based on studies, additive therapy, which constitutes a cocktail of beneficial microbes extracted from the healthy human body and introduced in fecal microbial transplantation, or through the consumption of probiotics, has shown significant results in gastrointestinal symptoms in children, such as Clostridium difficile infections, contributing to a significant improvement in ASD (Taniya, M. A et al., 2022).
In parallel with probiotics, fecal microbial transplantation covers around a thousand bacterial species from the GI, and according to a recent open study on the safety, tolerability and efficacy of FMT, it was concluded that it has great potential for the treatment of gastrointestinal problems in people with ASD, by rebalancing the intestinal microbiota (Yang, Y et al., 2018).
Numerous studies have reported on the use of controlled-release melatonin in ASD patients with sleep disorders. This resembles the circadian rhythm of melatonin secretion. The results indicate that it improves sleep quality, increases total sleep duration and reduces nocturnal awakenings. In addition, studies have looked into the efficacy of a pediatric melatonin extended-release formulation (PedPRM), which showed a significant reduction in sleep latency and improvement in total sleep time, with no adverse effects on growth and development (Maurer, J. J et al., 2023). In addition, there are studies on an integrative approach combining the use of melatonin with ESDM (Early Start Denver Model), which is an early behavioral and developmental intervention designed for the delivery of children aged 12 to 60 months. ESDM aims to interact with the child by synchronizing the therapist’s motor, emotional and relational rhythms with those of the child. Thus, ESDM is designed for the development of social engagement and interactional synchrony in autistic children, where the therapist spontaneously imitates the child’s actions and follows their rhythm, with the purpose of facilitating motivated response and contact. This integrated physiological and psychological approach brings relevant therapeutic concepts to ASD based on the regulation of physiological rhythms through the use of melatonin combined with the coordination of motor, emotional and relational rhythms through ESDM (Tordjman, S et al., 2015).
Melatonin, an endogenous hormone secreted by the pineal gland, has the function of sleep-wake regulation and is necessary for neurodevelopment and embryonic growth. Reduced plasma levels of melatonin are correlated not only in ASD patients, but also in the mothers of these children during their pregnancy. Interestingly, the inadequate synthesis of melatonin in autistic patients is in the brain and gastrointestinal tract, thus indicating that GI melatonin contributes to ASD pathology. In view of this, the establishment of the intestinal microbiota falls in the same critical timeframe for neurodevelopment. However, studies have shown that melatonin supplementation early in life and during pregnancy and lactation alleviates behaviors and rescues social deficits in ASD via restoration of the dysbiotic gut microbiota (Liu, X et al., 2022).
In a systematic review of the scientific literature on equine-assisted therapy intervention, they found a positive effect on the postural control of patients with autism, improving balance, since it is an activity that requires the coordination of multiple sensory channels. In addition, they experienced improvements in social interaction, positive emotions, stress and communication. At the end of the day, it is worth emphasizing that caring for postural control in autistic children is fundamental, since this gap directly influences the person’s autonomy and the execution of routine activities (Vives-Vilarroig, J et al., 2024).
It is clear that the endocannabinoid system is altered in many neurodegenerative diseases. And because of this, the eCB system controls emotional responses, behavioral reactivity and social interaction, which contributes to the autistic phenotype. In fact, the understanding of eCB signaling in autism is still being studied, but research in this area is set to evolve rapidly, and new drugs will be developed, including those that target metabolic enzymes of eCBs, and at the same time, key enzymes of oxidative pathways such as cyclooxygenases, which could be promising as therapeutics for human disorders with inflammatory elements, and thus be positive for ASD. In addition, antiepileptic drugs focused on the eCB system could effectively improve the symptoms associated with epilepsy that commonly occur in ASD (Chakrabarti, B et al., 2015).
A study was carried out comparing the response to treatment between pharmacological drugs or dietary supplements with placebo. This meta-analysis revealed that the response to treatment with placebo in clinical trials in ASD was moderate and detected five key factors that increase the placebo effect: outcome measures completed by clinicians, the level of response to active intervention, an active pharmacological intervention, adjuvant treatments and the geographical location of the study (Masi, A et al., 2015).
Recent progress in the genomics of non-syndromic autism spectrum disorder (nsASD) underscores the importance of de novo heterozygous mutations of large effect. These discoveries offer distinct opportunities for elucidating ASD-related biology and for developing precise therapies, although they present significant challenges. The phenotypes of interest, including social communication and complex behaviors, are highly derived in humans, making faithful recapitulation in animal models difficult. Furthermore, the tissue of greatest interest, the living human brain, is rarely accessible for direct investigation. This complicates the distinction between mutation-related biology and human pathophysiology. Therefore, approaches that use multiple nsASD risk genes in parallel may be crucial to understanding human pathology, based on the hypothesis that these genes converge at a point in the pathway from genes to behavior, leading to a shared and reproducible set of phenotypic characteristics defined as nsASD (Sestan, N et al., 2018).
With this information, it was possible to observe the importance of non-pharmacological treatment in patients with ASD, with the aim of reducing central and associated symptoms. Furthermore, in view of the aforementioned results, it was possible to note that it is essential to combine some of these non-pharmacological strategies, such as cognitive behavioral therapy with the use of melatonin, ketogenic diet or a therapy in order to rebalance the intestinal microbiome for example, in order to potentiate the reduction of symptoms and provide a better quality of life for people with this disorder and help them cope with the symptoms of this neurodevelopmental condition. With this in mind, it is of the utmost importance to increase the field of research into this area, i.e. in addition to looking for more non-pharmacological measures to help reduce symptoms, also to carry out larger studies over a longer period of time, so that the results really show whether or not there is an improvement.
Table 1. Methodological description of the studies included in this review.
AUTHOR STUDY TYPE NON-PHARMACOLOGICAL THERAPY THAT REDUCED SYMPTOMS CONCEPT White, S. W et al., 2018 Systematic Review Cognitive-behavioral therapy Includes exposure, modeling and parental involvement Lee, J. H et al., 2023 Clinical Trial Social skills training program in metaverse 4 teaching sessions on social skills and mindfulness from a therapist Cheng, N et al., 2017 Systematic Review Metabolic therapy Ketogenic diet, i.e. more fat and less carbohydrates Taniya, M. A et al., 2022 Systematic Review Subtractive therapy, bacteriocins and bacteriophages Used to fight pathogens in various ways: release of toxins, disruption of respiratory mechanisms, disintegration of the membrane and cell death, without harming other microbes in the gut Taniya, M. A et al., 2022 Systematic Review Additive therapy It consists of a cocktail of beneficial microbes extracted from the healthy human body and introduced through fecal microbial transplantation, or through the consumption of probiotics. Yang, Y et al., 2018 Systematic Review Fecal microbial transplantation It includes around a thousand bacterial species from the GI tract and therefore has great potential for rebalancing the intestinal microbiota Maurer, J. J et al., 2023 Systematic Review Controlled release melatonin and pediatric melatonin extended release formulation (PedPRM) It resembles the circadian rhythm of melatonin secretion and thus improves sleep quality. Tordjman, S et al., 2015 Systematic Review ESDM (Early Start Denver Model) Early behavioral and developmental intervention, which aims to interact with the child by synchronizing the therapist’s motor, emotional and relational rhythms with the child’s rhythms. Vives-Vilarroig, J et al., 2024 Control case Equine-assisted therapy Activity that requires the coordination of multiple sensory channels, thus improving balance Chakrabarti, B et al., 2015 Systematic Review Drugs that act on the eCB system They target metabolic enzymes of eCBs, and at the same time, key enzymes of oxidative pathways such as cyclooxygenases that may be promising as therapeutics for human disorders with inflammatory elements, and with this, they will be positive for ASD
Conclusion
In view of the information provided in the article, it was possible to observe the importance of non-pharmacological strategies in the treatment of ASD. However, due to the lack of studies on certain treatments, studies with small samples and studies carried out in a short period of time have limited the results of the work. This makes it necessary to carry out more studies on the subject.
Referências:
1. APA. (2013). Manual diagnóstico e estatístico de transtornos mentais: DSM-5 (5ª ed.). Associação Americana de Psiquiatria. [Google Acadêmico]]
2. Chakrabarti, B., Persico, A., Battista, N., & Maccarrone, M. (2015). Endocannabinoid Signaling in Autism. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics, 12(4), 837–847. https://doi.org/10.1007/s13311-015-0371-9]
3. Cheng, N., Rho, J. M., & Masino, S. A. (2017). Metabolic Dysfunction Underlying Autism Spectrum Disorder and Potential Treatment Approaches. Frontiers in molecular neuroscience, 10, 34. https://doi.org/10.3389/fnmol.2017.00034
4. Damiano, C. R., Mazefsky, C. A., White, S. W., & Dichter, G. S. (2014). Future directions for research in autism spectrum disorders. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 43(5), 828–843. https://doi.org/10.1080/15374416.2014.945214
5. Lee, J. H., Lee, T. S., Yoo, S. Y., Lee, S. W., Jang, J. H., Choi, Y. J., & Park, Y. R. (2023). Metaverse-based social skills training programme for children with autism spectrum disorder to improve social interaction ability: an open-label, single-centre, randomised controlled pilot trial. EClinicalMedicine, 61, 102072. https://doi.org/10.1016/j.eclinm.2023.102072
6. Liu, X., Cui, Y., Zhang, Y., Xiang, G., Yu, M., Wang, X., Qiu, B., Li, X. G., Liu, W., & Zhang, D. (2022). Rescue of social deficits by early-life melatonin supplementation through modulation of gut microbiota in a murine model of autism. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 156, 113949. https://doi.org/10.1016/j.biopha.2022.113949
7. McCracken, J. T., Anagnostou, E., Arango, C., Dawson, G., Farchione, T., Mantua, V., McPartland, J., Murphy, D., Pandina, G., Veenstra-VanderWeele, J., & ISCTM/ECNP ASD Working Group (2021). Drug development for Autism Spectrum Disorder (ASD): Progress, challenges, and future directions. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology, 48, 3–31. https://doi.org/10.1016/j.euroneuro.2021.05.010
8. Masi, A., Lampit, A., Glozier, N., Hickie, I. B., & Guastella, A. J. (2015). Predictors of placebo response in pharmacological and dietary supplement treatment trials in pediatric autism spectrum disorder: a meta-analysis. Translational psychiatry, 5(9), e640. https://doi.org/10.1038/tp.2015.143
9. Maurer, J. J., Choi, A., An, I., Sathi, N., & Chung, S. (2023). Sleep disturbances in autism spectrum disorder: Animal models, neural mechanisms, and therapeutics. Neurobiology of sleep and circadian rhythms, 14, 100095. https://doi.org/10.1016/j.nbscr.2023.100095
10. Sestan, N., & State, M. W. (2018). Lost in Translation: Traversing the Complex Path from Genomics to Therapeutics in Autism Spectrum Disorder. Neuron, 100(2), 406–423. https://doi.org/10.1016/j.neuron.2018.10.015
11. Taniya, M. A., Chung, H. J., Al Mamun, A., Alam, S., Aziz, M. A., Emon, N. U., Islam, M. M., Hong, S. S., Podder, B. R., Ara Mimi, A., Aktar Suchi, S., & Xiao, J. (2022). Role of Gut Microbiome in Autism Spectrum Disorder and Its Therapeutic Regulation. Frontiers in cellular and infection microbiology, 12, 915701. https://doi.org/10.3389/fcimb.2022.915701
12. Tian, J., Gao, X., & Yang, L. (2022). Repetitive Restricted Behaviors in Autism Spectrum Disorder: From Mechanism to Development of Therapeutics. Frontiers in neuroscience, 16, 780407. https://doi.org/10.3389/fnins.2022.780407
13. Tordjman, S., Davlantis, K. S., Georgieff, N., Geoffray, M. M., Speranza, M., Anderson, G. M., Xavier, J., Botbol, M., Oriol, C., Bellissant, E., Vernay-Leconte, J., Fougerou, C., Hespel, A., Tavenard, A., Cohen, D., Kermarrec, S., Coulon, N., Bonnot, O., & Dawson, G. (2015). Autism as a disorder of biological and behavioral rhythms: toward new therapeutic perspectives. Frontiers in pediatrics, 3, 1. https://doi.org/10.3389/fped.2015.00001
14. Vives-Vilarroig, J., Ruiz-Bernardo, P., & García-Gómez, A. (2024). Effects of Horseback Riding on the Postural Control of Autistic Children: A Multiple Baseline Across-subjects Design. Journal of autism and developmental disorders, 10.1007/s10803-023-06174-5. Advance online publication. https://doi.org/10.1007/s10803-023-06174-5
15. Waizbard-Bartov, E., Fein, D., Lord, C., & Amaral, D. G. (2023). Autism severity and its relationship to disability. Autism research : official journal of the International Society for Autism Research, 16(4), 685–696. https://doi.org/10.1002/aur.2898
16. White, S. W., Simmons, G. L., Gotham, K. O., Conner, C. M., Smith, I. C., Beck, K. B., & Mazefsky, C. A. (2018). Psychosocial Treatments Targeting Anxiety and Depression in Adolescents and Adults on the Autism Spectrum: Review of the Latest Research and Recommended Future Directions. Current psychiatry reports, 20(10), 82. https://doi.org/10.1007/s11920-018-0949-0
17. Yang, Y., Tian, J., & Yang, B. (2018). Targeting gut microbiome: A novel and potential therapy for autism. Life sciences, 194, 111–119. https://doi.org/10.1016/j.lfs.2017.12.027
1Centro universitário Barão de Mauá, CBM, Ribeirão Preto, São Paulo, Brasil.
2Universidade Federal do Ceará, UFC, Fortaleza, Ceará, Brasil.
3Universidade Federal do Amapá, UNIFAP, Macapá, Amapá, Brasil
