REGISTRO DOI: 10.69849/revistaft/ch10202509220628
Isabela Gouveia Thomasini1
Marcia Elisabetth Rodrigues2
Eduardo Caldeira2,3
Saulo Duarte Passos2
ABSTRACT
There are several craniofacial alterations described in children with microcephaly associated with Congenital Zika Syndrome (CZS). However, the effects of CZS on craniofacial development and acquired therapies in infected children are still unknown. The aim of the study was to evaluate the main defects in craniofacial development and their relationship with CZS, as well as therapies inspired by joint and neuromuscular stimuli in patients attended by the Pediatric Service of the University Hospital. Patients were evaluated, and followed by Physiotherapy, Osteopathy and Maxillofacial Surgery. The joint care for the treatments was carried out by Osteopathy and Maxillofacial Surgery. The stimuli used in the therapies were based on the osteoarticular and neuromuscular system. Between the years 2022 and 2023, a total of 156 patients were treated and of these, 18 provided effective continuity of care. Of the patients seen, it was mainly observed alterations in craniofacial growth 5 (28%), nuchal shortening and cervical instability 3 (17%), difficulty swallowing and chewing 4 (22%), maxillary and palatal atrophy 2 (11%), patient without alterations 4 (22%). After the osteopathic and physiotherapy treatments, a qualitative improvement was observed, mainly in relation to cervical stability and nuchal control, in addition to the positive general condition of the patients. The follow-up of these patients, focusing on osteopathic practices, was fundamental for the improvement in the craniofacial and neck development, which could subsequently reduce the need of craniofacial surgeries. Despite this, we emphasize that there is still no consensus on new therapies and the relationship between CZS and craniofacial deformities.
Keywords: Zika Syndrome; Craniofacial deformities; Osteopathy; and Maxillofacial surgery
INTRODUCTION
Zika Virus – ZIKV
Are what the orofacial changes in children with microcephaly associated with the Zika Virus? This is a question that has been asked by different researchers around the world due to the scarcity of literature in the area by da Silva Sobrinho et al.
Gomes et al. describe children with microcephaly. Among the findings, there are delays and changes in the eruption sequence of deciduous teeth, as well as enamel development defects, which, despite being concomitant, are not associated with Zika virus infection. Another study also highlights oral alterations in children with microcephaly associated with Congenital Zika Syndrome. They are more likely to present some of these alterations, such as difficulty sealing the lips, Silva et al; da Silva Sobrinho and Ventura.
Ribeiro et al. studying children with microcephaly due to congenital Zika infection, showed functional, oral and maxillofacial alterations and less facial development compared to Non-CZS children of the same age group. In another international study, the true association between the Zika virus and the occurrence of microcephaly was verified, studies were carried out focusing on the effects of the infection on fetal development da Silva Rosa et al.
Also, some studies have reported smaller head circumference at birth when compared to normal children of approximately the same age. The shortened upper third of the face and the presence of hypertonic masticatory muscles, hypotonic swallowing muscles, dysphagia, teeth clenching, labial weakness, tongue thrusting, hypersalivation and epilepsy. The deciduous dentition was complete with normal dental morphology; however, the dental eruption was altered, numerous dental caries and malocclusion Aragón et al.
Ventura et al. evaluating a total of 469 children with a mean age of 5.0 ± 7.1 months (range, 0.0-36.0 months), noted microcephaly in 214 (45.6%) children; and 62 cases (29.0%) in severe conditions. In Pernambuco, cases were significantly more prevalent compared to the states of Bahia and Rio de Janeiro.
Other results already show moderate scientific evidence regarding the association of ZIKV with orofacial alterations in children with CZS by da Silva Sobrinho. Several other authors also report the very low certainty of evidence between CZS and craniofacial deformities Silva et al.
Thus, the Congenital Zika Virus Syndrome is a condition already known and much studied, but little addressed in relation to speech, language and hearing disorders in children da Silva Rosa et al.
In this way, it is clear the need for further studies on the relationship between CZS and deformities in craniofacial development, as well as finding therapeutic options to help in the correct evolution of the head and neck region, which may even reduce future indications for maxillofacial surgical interventions.
AIM
Thus, the objective of the present study was to evaluate the main defects in craniofacial development and their relationship with CZS, as well as therapies inspired by joint and neuromuscular stimuli in patients attended by the Pediatric Service of the University Hospital of Jundiaí/ Project Zika Virus.
METHODS
The patients were evaluated by the Pediatrics, Physiotherapy, Osteopathy and Maxillofacial Surgery Services. The care is always provided initially by Pediatrics, and jointly by the affinity of treatments by Osteopathy and Maxillofacial Surgery, and, if necessary, referred to Physiotherapy. This project was approved by the Research Ethics Committee of Jundiaí Medical School Process number: 1446577. Fapesp Grants number: 16/08578-0 and 2018/08578-0
Therapeutic Protocols
Regarding the physiotherapeutic and osteopathic activities, the techniques used in manual therapy were manipulations, mobilizations and specific exercises with the objective of stimulating proprioception, producing elasticity of the adhered structures, in relation to the joints, stimulating the synovial fluid and promoting the reduction of pain, as well as stimulating the sutures (fibrous joints). With regard to the Temporomandibular Joint (TMJ), a joint mobilization technique similar to that proposed by Maitland was used, which is based on passive oscillatory, rhythmic movements, classified into four levels of mobilization and a fifth level called direct joint manipulation. All these stimuli were manual directly or indirectly in the TMJ area.
Neuromuscular mobilization is based on the principle that impairments in the functioning and mechanics of the nervous system (elasticity, movement, conduction, axoplasmic flow) and muscle can generate dysfunctions of the nervous system or in the musculoskeletal structures innervated by it, and that the recovery of biomechanics and proper physiology, allows you to restore the extensibility and normal function of these systems, as well as improve the conduction of the nerve impulse. The technique consists of imposing greater tension and/or movement on the neuromuscular system, through certain postures and stimuli so that, then, slow and rhythmic directed and regional movements are applied by Vasconcelos, Machado & Bigolin, Machado.
Remembering that Physiotherapy and mainly Osteopathy has as a basic concept; “Man is an indivisible being” and self-regulation as a principle, where the body has the capacity for self-healing, that is, the “Principle of Immunity”. Another principle is that the structure commands the function, therefore, dysfunctions can be diagnosed and treated. Osteopathy analyzes the body as a unit, where everything is interconnected and has the function of acquiring homeostasis. In this way, the body has the ability to regain balance (Rauber, 2007; Rezende & Gabriel, 2008).
Statistical analysis
For analysis of the results, as well as for the mathematical calculations involved in the studies, the GraphPad Prism 5.0 program was used. From this program, ANOVA (one way) was performed, for a minimum value of p≤0.05 (Mandarim de Lacerda, 1995).
RESULTS AND DISCUSSION
The service assisted patients with CZS in the areas of Pediatrics, Physiotherapy, Occupational Therapy, Nursing, Osteopathy and Maxillofacial Surgery.
Between 2022 and 2023, a total of 156 patients were treated, and of these, 18 provided effective continuity (minimum returns) in care (Figure 1).
Figure 1: Sample of patients assisted at the Pediatric Sevice (Zika Virus Project) in relation to those who followed up with the minimum number of returns and therapies.
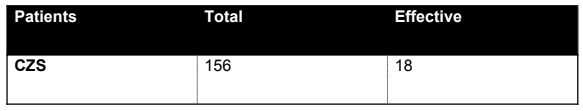
It is important to highlight that the evasion occurred due to the financial conditions of the patients, who in the vast majority have precarious conditions and this can influence in locomotion, per diem, and food costs.
The basis for determining facial growth was based on the study of the Z angle (Figure 2).

Figure 2: Measured angle (Z) from the tragus to the nasal apex region and nasomental line. Being the average in children of 58 to 62 degrees.
In addition to this measure, the head circumference was also taken for boys equal to or less than 31.9 cm and girls equal to or less than 31.5 cm (17) (Figure 3).

Figure 3: Head circumference measurement (cm).
Of the patients seen, it was observed mainly changes in craniofacial growth (head circumference and z angle) 5 (28%), nuchal shortening and cervical instability 3 (17%), difficulty swallowing and chewing 4 (22%), maxillary and palatal atrophy 2 (11%), patient without changes 4 (22%) (Figure 4).
Figure 4: Most frequently detected craniofacial deformities among patients seen at the Pediatric Service of the University Hospital at Jundiaí.
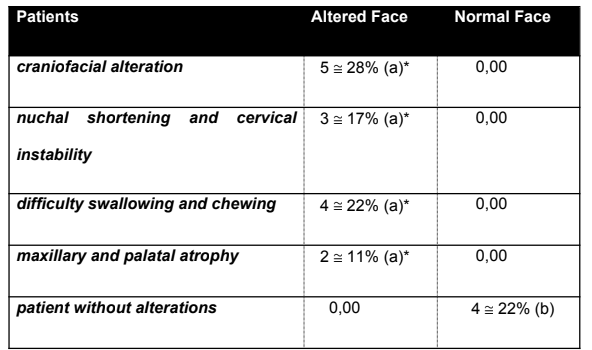
a,b differ at 5% significance (ANOVA)
Patients with craniofacial alterations were submitted to physiotherapy and osteopathy, followed by maxillofacial surgery, focusing on myomodulation and muscle strengthening therapies, mainly to strengthen the masticatory muscles and facial expression with manual excitatory stimuli. In addition to strengthening and developing the neck muscles as seen in Figure 5 with image A; demonstrating patient with shortening of the neck muscles and in image B; patient already with cervical control and stability.

Figure 5: (A) Patient with cervical instability and shortening of the neck muscles. (B) Patient after 8 months of osteopathic and physiotherapeutic therapy with development of nuchal stability and reversal of shortening of the nuchal muscles.
Osteopathy has neuromuscular stimuli and bone-joint stimuli as its principles. In this regard, some authors have been describing the use of different treatments and alternative therapies to inactivate the virus and its complications, with very promising results by Batista et al.
The results observed in our study corroborate the scientific evidence that shows the association of ZIKV with orofacial alterations in children with microcephaly. da Silva et al. observed mainly alterations in the chronology of dental eruption, alteration in the teeth and in the attached oral structures da Silva Sobrinho et al.
Within these frameworks of craniofacial deformities, mandibulofacial dysostosis with microcephaly (MFDM) is a multiple malformation syndrome that comprises microcephaly, craniofacial anomalies, hearing loss, dysmorphic features and, in some cases, esophageal atresia. Being the GTPase, U5-116 kDa/EFTUD2, the responsible factors , observed by Huang et al.
Yang et al. indicate that mandibulofacial dysostosis is related to potentially pathogenic mutations, particularly in rare diseases, which makes genetic mapping and careful prenatal diagnosis necessary (Yang et al. 2022). Medina et al. observing 38 eligible children, with a mean age of 12.4 months, describes significant changes in the sequence of tooth emergence. In addition, tooth agenesis, gingival bleeding, narrow palate, and bruxism were observed (Medina et al. 2022). These results shown in the literature converge with the results observed in our Service, where the relationship between CZS and craniofacial deformities were significant.
CONCLUSIONS
Our results showed a significant relationship between CZS and craniofacial deformities, especially in relation to craniofacial growth, cervical stability and difficulties in chewing and swallowing.
We could also observe positive preliminary results using therapies based on Physiotherapy and Osteopathy, with follow-up from the Maxillofacial Surgery area.
These therapies focused on bone-joint stimuli and neuromuscular stimuli, with the aim of stimulating craniofacial growth. Results were mainly qualitative with regard to cervical stability and control, as well as general child development.
These results are important because, in the long term, you can avoid maxillofacial surgical procedures. Despite these results, there are still doubts and there is no consensus regarding all craniofacial alterations and therapies, which denotes the need for further studies in this area.
REFERENCES
Aragón N, Díaz C, Contreras A. Dental, Occlusal, and Craniofacial Features of Children With Microcephaly Due to Congenital Zika Infection: 3 Cases Report From Valle del Cauca, Cali-Colombia-2020. Cleft Palate Craniofac J. v.58, n.10, p.1318-1325, 2021.
Batista MN, Braga ACS, Campos GRF, Souza MM, Matos RPA, Lopes TZ, Candido NM, Lima MLD, Machado FC, Andrade STQ, Bittar C, Nogueira ML, Carneiro BM, Mariutti RB, Arni RK, Calmon MF, Rahal P. Natural Products Isolated from Oriental Medicinal Herbs Inactivate Zika Virus. Viruses. v. 11, n. 1, p. 49, 2019.
da Silva Rosa CB, Hernandez Alves Ribeiro César CP, Paranhos LR, Guedes-Granzotti RB, Lewis DR. Speech-language disorders in children with congenital Zika virus syndrome: A systematic review. Int J Pediatr Otorhinolaryngol. v. 138, p. 110309, 2020
da Silva Sobrinho AR, Ramos LFS, Maciel YL, Maurício HA, Cartaxo RO, Ferreira SJ, Sette-de-Souza PH. Orofacial features in children with microcephaly associated with Zika virus: A scoping review. Oral Dis. v. 28, n. 4, p. 1022-1028, 2022.
Gomes PN, do Amaral BA, Azevedo ID, de Medeiros Maia HC, Arrais NMR, de Lima KC. Association of congenital Zika syndrome with dental alterations in children with microcephaly. PLoS One. v. 1, n. 11, p. e0276931, 2022.
Huang L, Vanstone MR, Hartley T, Osmond M, Barrowman N, allanson J, Baker L, Dabir TA, Dipple KM, Dobyns WB, Estrella J, Faghfoury H, Favaro FP, Goel H, Gregersen PA, Gripp KW, Grix A, Guion-Almeida ML, Harr MH, Hudson C, Hunter AG, Johnson J, Joss SK, Kimball A, Kini U, Kline AD, Lauzon J, Lildballe DL, López-González V, Martinezmoles J, Meldrum C, Mirzaa GM, Morel CF, Morton JE, Pyle LC, Quintero-Rivera F, Richer J, Scheuerle AE, Schönewolf-Greulich B, Shears DJ, Silver J, Smith AC, Temple IK, UCLA Clinical Genomics Center, Van de Kamp JM, Van Dijk FS, Vandersteen AM, White SM, Zackai EH, Zou R, Care4rare Canada Consortium, Bulman DE, Boycott KM, Lines MA. Mandibulofacial Dysostosis with Microcephaly: Mutation and Database Update. Hum Mutat. v. 37, n. 2, p. 148-54, 2016.
Machado GF, Bigolin SE. Estudo comparativo de casos entre a mobilização neural e um programa de alongamento muscular em lombalgicos crônicos. Fisioter. mov. v. 23, n. 4, p. 545-554, 2010.
Maitland GD. Princípios das técnicas. In: Maitland GD, editor. Maitland’s Vertebral Manipulation. 6nd ed. London: Butterworth Heinemann, 2001.
Mandarim de Lacerda, CA. Métodos quantitativos em morfologia. EDUERJ, Rio de Janeiro, 1995.
Medina DT, Santos APPD, Rodrigues FMDF, Oliveira BH. Oral manifestations of congenital Zika virus infection in children with microcephaly: 18-month follow-up case series. Spec Care Dentist. v. 42, n. 4, p. 343-351, 2022.
Rauber D. Tratamento da hérnia de hiato através de técnicas osteopaticas. Monografia (Bacharel em Fisioterapia) Faculdade Assis Gurgacz, 2007.
Rezende RPDB; Gabriel A. Relações entre clínica e osteopatia. Rev Bras Clin Med. 2008.
Ribeiro RA, Mattos A, Meneghim MC, Vedovello SAS, Borges TMD, Santamaria M. Oral and maxillofacial outcomes in children with microcephaly associated with the congenital Zika syndrome. Eur J Orthod. v. 8, n. 3, p. 346-352, 2021.
Silva LVO, Hermont AP, Magnani IQ, Martins CC, Borges-Oliveira AC. Oral alterations in children with microcephaly associated to congenital Zika syndrome: A systematic review and meta-analyses. Spec Care Dentist. v. 43, n. 2, p. 184-198, 2023.
Vasconcelos DA, Lins LCRF, Dantas EHM. Avaliação da mobilização neural sobre o ganho de amplitude de movimento. Fisioter. mov. v. 24, n. 4, p. 665-672, 2011.
Ventura CV, Zin A, Paula Freitas B, Ventura LO, Rocha C, Costa F, Nery N Jr, De Senna TCR, Lopes Moreira ME, Maia M, Belfort R Jr. Ophthalmological manifestations in congenital Zika syndrome in 469 Brazilian children. J AAPOS. v. 25, n. 158, p. e1-158.e8, 2021.
Veras, Larissa Sales Teles; Vale, Rodrigo Gomes de Souza; Mello, Danielli Braga de; Castro, JoséAdail Fonseca de; Dantas, Estelio Henrique Martin. Avaliação da dor em portadores de hanseniase submetidos a mobilização neural. Fisioterapia e Pesquisa, São Paulo, 2011.
Yang M, Liu Y, Lin Z, Sun H, Hu T. A novel de novo missense mutation in EFTUD2 identified by whole-exome sequencing in mandibulofacial dysostosis with microcephaly. J Clin Lab Anal. v. 36, n. 5, p. e24440, 2022.
1Undergraduated Student of Dental Medicine, Campo Limpo Paulista, São Paulo, Brazil
2Pediatric Ambulatory Clinic Zika Virus, University Hospital, Jundiaí Medical School, Jundiaí, São Paulo, Brazil
3Maxillofacial Surgery Service, Clinical Hospital, Campo Limpo Paulista, São Paulo, Brazil;
Contact author:
Dr. Eduardo Caldeira PhD
Maxillofacial Surgery Service, Clinical Hospital, Campo Limpo Paulista, São Paulo, Brazil
eduardo.caldeira@faccamp.br
