REGISTRO DOI: 10.5281/zenodo.8327498
Thiago Santos Mendes1
Guto de Oliveira e Silva2
Ana Paula Terossi de Godoi3
Abstract
This study evaluated the “in vitro” shear bond strength (SBS) and adhesive remnant index (ARI) of
ceramic brackets bonded to two types of materials for temporary crowns under different surface
treatments.
Overall, 180 specimens were prepared (n = 10), with 90 specimens of chemically activated acrylic
resin (CAAR) and DuraLay acrylic resin; bis-acrylic resin (BR) each. They were classified into three
groups (no roughening, roughening with a drill, and sandblasting with aluminum oxide) based on
mechanical treatment and subdivided into three groups based on chemical treatment/gluing (TB,
Transbond XT; FB, Filtek Bulk Fill Flow; and CAAR, DuraLay acrylic resin). After bonding, the
brackets underwent 5000 thermal cycles, followed by the SBS test using a universal machine and ARI
evaluation. Data were analyzed using generalized linear models (α = 5%).
A difference was observed between the two provisional materials, among the types of mechanical chemical surface treatments. Most groups had an ARI of 3. Thus, BR had higher SBS values than CAAR. On provisional CAAR surfaces, mechanical preparation is not required when the resin is used for bracket bonding; however, it is required when bonded to TB or FB resin. On temporary BR surfaces, FB resin was the ideal bonding agent.
Keywords: acrylic resins, dental materials, orthodontic brackets, shear strength
INTRODUCTION
The increasing number of adults seeking orthodontic treatment has led the orthodontic materials
industry to search for more discreet fixed appliances with good clinical performance to meet the
demands of patients and orthodontists [1]. Accordingly, ceramic brackets were introduced, which
present as advantages, aesthetics, biocompatibility, resistance to chemical and thermal alterations and
adequate bond strength against masticatory movements [2].
This patient profile, in some cases due to trauma, caries, fractures, or endodontic treatment failures,
may present with the absence of some dental elements or even provisional restorations [3], creating a
problem for bonding brackets on these teeth [4].
Therefore, the correct union between the brackets and the surfaces of the temporary crowns is a
prerequisite for the success of orthodontic treatment [4], as it is not recommended to replace these
crowns with permanent ones during treatment due to possible occlusal changes resulting from tooth
movement. When the provisional restoration is located posteriorly to the arch, it is not advisable to
glue the teeth containing the crown, whereas, when located anteriorly, it is advisable to directly glue
the accessories due to the unaesthetic appearance of the bands [5] to promote protection and
stabilization to the arch position of the tooth before making the definitive crown [6]. In addition, they
contribute to restoring aesthetics and function during the rehabilitation treatment [7].
Among the materials available for making temporary crowns, chemically activated acrylic resin
(CAAR) is the most widely used owing to its low cost, easy handling, and possibility of repair,
adjustment, and reline [5].
Currently, bis-acrylic resins (BRs) are widely used as an alternative for provisional restorations owing
to their simple manufacturing and handling methods, favorable aesthetics, ease of polishing, and
mechanical properties superior to CAAR [8].
Several surface preparation techniques have been proposed to overcome the problems encountered
when bonding orthodontic brackets on these surfaces. In the literature, the most commonly reported
mechanical methods are surface asperization with a bur or aluminum oxide jet. Among chemical
methods, conditioning with phosphoric acid or hydrofluoric acid is highlighted [4].
The lack of a standardized protocol has generated empirical techniques for bonding orthodontic
accessories on temporary crowns, which can lead to numerous detachments and, consequently,
problems during treatment [9]. Frequently performing procedures for relocating brackets make it
impossible to advance mechanotherapy, increasing costs and clinical care time and contributing to
longer treatment time [10], which is undesirable for orthodontists and patients [11].
Studies have compared different acrylic resins used for temporary crowns [3], different methods of
surface preparation before bracket bonding, and different adhesives [5]. However, no consensus has
been made on the best surface treatment [7].
Owing to the scarcity of studies using Filtek Bulk Fill Flow resins to bond ceramic brackets, this
material was selected in the present study.
The null hypotheses are as follows: there is no difference between the two provisional restorative
materials, between the three types of mechanical surface treatments, and between the three chemical
surface treatments–bonding agents.
Thus, this study aimed to evaluate in vitro the shear bond strength (SBS) of ceramic brackets bonded
on two types of temporary crown materials under different surface treatments and assess the
debonding pattern using the adhesive remnant index (ARI).
MATERIALS AND METHODS
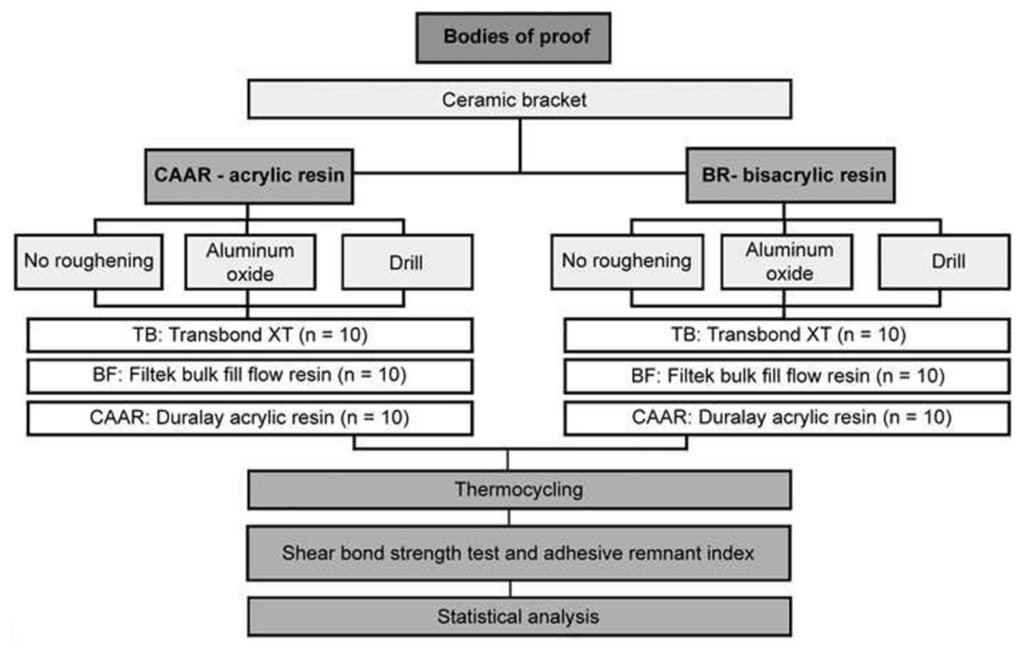
After an in vitro pilot experiment, 180 (n = 10) specimens were made in a trapezoidal shape,
measuring 3 mm in height, with upper and lower bases of 10 × 8 mm and 8 × 6 mm, respectively, and
90 samples of each material temporary restorative (substrate), namely DuraLay acrylic resin (Reliance,
Itasca, USA) and Structur 3 BR (Voco, GmbH, Germany), were prepared (Figure 1).
Inclusion criteria were samples with a smooth surface, without technical failures, such as fractures and
bubbles, and stored in artificial saliva at 37°C in an oven for 24 hours. After this period, the burrs were removed with fine, medium and coarse sandpaper discs (Vortex, São Paulo, Brazil) and polished with a goat hair brush (American Burrs, Palhoça, Brazil) and Diamond Excel polishing paste (FGM, Joinville, Brazil), with an extra fine grain of 2 to 4 microns [12].
In the sequence, the trapezoids were included in rigid polyvinyl chloride tubes (Amanco, Joinvile, Brazil) of 15 × 25 mm of external diameter, using colorless CAAR (Vipi, Pirassununga, Brazil), manipulated in proportions recommended by the manufacturer (Figure 2) .
Each group was divided according to the type of surface treatment (Figure 3): no roughening (control),
mechanical treatment (roughening with a drill, sandblasting with aluminum oxide) [13]; chemical
treatment with adhesives Transbond XT resin + Transbond XT primer (TB), Filtek Bulk Fill Flow
resin + universal single bond (FB) and DuraLay acrylic resin + monomer (CAAR), and all groups
received some type of treatment before bonding.
Polycrystalline ceramic Roth brackets (Ortometric, Marilia, Brazil) were used for upper right central
incisors, with dimensions of 3.3 × 3.6 mm and slot of 0.022 × 0.028. Photoactivation was performed
using an Optilight Max (Saevo, Ribeirão Preto, Brazil) device with a power of 1200 mW/cm2 for
bonding on provisional resin surfaces, except for the CAAR group because this presents chemical
polymerization. Light intensity was measured by an RD-7 radiometer (Ecel, Ribeirão Preto, Brazil)
every five photo activations.
After bonding, the specimens were thermocycled (5000 cycles) in an MCT-2 machine at temperatures
of 5°C and 55°C with an immersion time of 30 seconds and a 4-second interval between baths [14], submitted to the 24-hour SBS test after.
The SBS test was performed in a universal machine AME-5kN (Oswaldo Filizola, São Paulo, Brazil), in which the chisel-shaped rod of the machine was positioned at the adhesive interface bracket/substrate surface (Figure 4). The load exerted by the machine was 0.5 mm/min for all specimens until the bracket was removed from the resin surface. The loads were recorded in N (Newton) and later transformed into megapascal (Mpa) using the following formula: SBS = F/A × g, where SBS is the shear bond strength, F is the force required to remove the bracket from the resin surface, and A is the bracket area, (g) presented gravity acceleration of 9.8 m/s2, and A is the bond area of the brackets to the tooth in mm2.
After the SBS test, the ARI was analyzed under a magnifying glass with a 100-mm magnifying lens
(Figure 5), where the bracket base and cylinder surface were analyzed and failure patterns were
classified according to Artun and Bergland’s scores [15]: 0, no adhesive remaining on the resin
surface; 1, half of the adhesive remained on the resin surface; and 3, all adhesive remained on the resin surface, with the impression of the bracket
base.
Descriptive and exploratory analyses of the SBS data were performed. As the data present asymmetric
distribution, they were analyzed by generalized linear models considering the study factors of
provisional restorative material, type of mechanical surface treatment, chemical surface treatmentbonding agents, and double and triple interactions between them. All analyses were performed in the R program (R Core Team, Vienna, Austria, 2019) with a significance level of 5%.
RESULTS
A three-way interaction was found between factors (p < 0.05) (Table 1). For the TB and FB chemical surface treatments, BR showed higher SBS than CAAR when no mechanical surface treatment was employed and when asperization with a bur was performed (p < 0.05). When aluminum oxide blasting was performed, the BR group showed greater SBS than the CAAR group for treatment with Filtek Bulk Fill Flow resin (p < 0.05). Among groups that received DuraLay acrylic resin as a chemical surface treatment, higher SBS and lower SBS were observed in the DuraLay acrylic resin when no asperization was performed and when drill asperization was employed, respectively.
As for the type of mechanical treatment, in the acrylic resin with TB chemical treatments and FB resin, the group without asperization showed lower SBS than the others (p < 0.05). In the CAAR group with DuraLay acrylic resin, the group without asperization showed higher SBS (p < 0.05). In the BR group with TB, the group that received asperization with drill showed greater resistance than others (p < 0.05). In this same resin, Filtek Bulk Fill Flow, the highest SBS occurred in the group with asperization with a bur, followed by the group with blasting with aluminum oxide, and lower SBS was observed in the group without asperization (p < 0.05). Moreover, in the BR group with DuraLay acrylic resin, lower SBS was observed with aluminum oxide blasting than in the other groups (p<0.05).
For the comparisons between chemical surface treatments using bonding agents, in DuraLay acrylic resin without roughing, the highest SBS occurred with the treatment with DuraLay acrylic resin, followed by the treatment with Filtek Bulk Fill Flow + single bond universal resin and then the treatment with Transbond XT + Transbond Primer (p < 0.05). In this same resin, when aluminum oxide blasting was performed, the SBS was higher for the treatment with DuraLay acrylic resin than with Transbond XT + Transbond Primer (p < 0.05). When using asperization with a bur on DuraLay acrylic resin, no significant difference was found between the three surface treatments using bonding agents (p > 0.05). For the BR without asperization, the SBS was significantly higher when treated with DuraLay acrylic resin than with Transbond XT + Transbond Primer (p < 0.05). For groups that received aluminum oxide blasting and drill roughening, the SBS was significantly higher in the Filtek Bulk Fill Flow + single bond universal resin than in the other groups (p < 0.05).
The ARI data were analyzed, and in all types of surface treatments, a predominant score of 3 was found, except for the Transbond resin without surface roughening; in CAAR, a score of 0 prevailed (Figure 6).
DISCUSSION
Here, thermocycling was performed to simulate oral conditions, subjecting to 5000 cycles. Samples subjected to 1000 thermocycling cycles correspond to ~1 month of clinical function [16]; therefore, the time was estimated to correspond to a 5-month treatment. The first null hypothesis that is, there is no difference between the two temporary materials in relation to SBS, was rejected, as BR presented higher SBS than CAAR resin. These findings can be attributed to the presence of bifunctional acrylates, which provide less weakening of the material in the presence of moisture, as substrate and cement are types of composite resins [17].
Bis-acrylic materials are a combination of dimethacrylate (bis-GMA) which is found in composite resins. They form polymers via free radicals, resulting in better adhesion to the light cured bonding resin [3].
The second null hypothesis that is, there is no difference between the three types of mechanical treatment, was rejected. When using Transbond resin and Filtek Bulk Fill Flow for bonding CAAR crowns, some mechanical treatments (aluminum oxide blasting or bur roughening) must be performed. These findings are in line with the finding that SBS increases when one of the two surface treatments is used [5], further showing that aluminum oxide blasting provides deeper grooves than bur spraying providing greater SBS when brackets are used. In contrast, they reported greater SBS after surface grinding with a diamond bur than with aluminum oxide grinding [14], demonstrating by scanning electron microscopy that aluminum oxide blasting creates areas of micromechanical retention, while the diamond bur creates macro and micromechanical areas, producing better retention. Although the literature is controversial in this regard, the present study revealed that both forms of mechanical retention provide satisfactory SBS.
As for the second point, when no mechanical surface treatment should be performed when bonding with the acrylic resin, this was also reported previously [18]. Simply wetting the material with monomer can work as an additional measure to improve the effectiveness of the chemical interaction between resins [19].
The third null hypothesis, that is, there is no difference between the three chemical surface treatments,
was rejected because, according to the results presented for BR, the best chemical bonding agent is
Filtek Bulk Fill Flow resin, regardless of the mechanical treatment, while for CAAR, the best chemical
bonding agent is acrylic resin when not spraying. Results for CAAR were confirmed [20,21]. Acrylic
resin is recommended for bonding to acrylic surfaces because its bond strength is greater than the bond
strength of other bonding agents. Furthermore, the tertiary amines present in the CAAR composition
can inhibit the polymerization of photopolymerizable resins (Transbond/Filtek Bulk Fill Flow),
impairing the bond between the materials [11].
In this study, all SBS results are within the minimum necessary to withstand orthodontic forces,
between 5.9 and 7.8 MPa [22,23], being strong enough to prevent bracket breakage during orthodontic
treatment [4].
The analysis of the substrate surface after the SBS test was evaluated using the ARI [15]. In all groups,
the most common score was 3 points, showing that most fractures after debonding occurred at the
bracket/composite interface. The CAAR substrate group was exempted because when it did not
receive mechanical treatment on its surface before bonding with Transbond resin, more scores of
number 0 points were found, demonstrating that most fractures after debonding occurred at the
composite/substrate interface.
The ARI data are in agreement with the SBS results. The fact that most groups scored an ARI of 3
infers the presence of good adherence; however, this can lead to fractures of the temporary material, as
was verified in seven specimens, however, as it is a temporary material that can be replaced, this is not
a problem.
The limitation of the SBS test is the difficulty in standardization during bonding, especially regarding
the removal of excess bonding adhesives that do not contrast with the resin material surface [24] and
aesthetic bracket, making their removal difficult. This aspect also has a negative clinical effect because
resin residues may have accumulated at the crown–adhesive interface, favoring early staining of the
temporary crown by the dental biofilm accumulation and gingival inflammation [25]. To solve this
problem, further studies are needed.
The present study guides the dental surgeon in the choice of material, for making the provisional
crown and for choosing the best material to be used for bonding in the presence of several clinical
possibilities.
CONCLUSION
This study’s findings revealed that BR presented higher SBS values than CAAR. On provisional
surfaces with CAAR, no mechanical preparation is necessary when using the resin itself for bonding
the bracket, whereas when bonded with Transbond or Bulk Fill Flow resin, surface preparation
(asperization with a bur or aluminum oxide jetting) should be performed. On BR provisional surfaces,
Filtek Bulk Fill Flow resin was the best bonding agent regardless of the mechanical surface treatment.
CONFLICT OF INTEREST:
No conflict of interest to disclose.
ACKNOWLEDGMENTS:
To God, to my family in the person of my parents Paulo and Fátima and
my wife Bruna, to the Coordinator of the Graduate Course in Orthodontics, to all friends and
colleagues.
FUNDING:
This research did not receive any specific grant from funding agencies in the public,
commercial, or not-for-profit sectors.
AUTHOR CONTRIBUTIONS:
Thiago: Conceptualization, Methodology, Data collection, Software, Investigation, Writing-Original
draft preparation. Guto: Data collection, Software, Investigation, Writing-Original draft preparation.
Ana Paula: Software, Investigation, Writing-Original draft preparation.
DATA AVAILABILITY STATEMENT:
The datasets used and/or analyzed during the current study are available from the corresponding
author on reasonable request.
REFERENCES
- C.R. Sobreira, L.B. Loriato, D.D. Oliveira, Braquetes estéticos: características e
comportamento clinic, Rev. Clín. Ortodon. Dental Press. 6 (2007) 94–102. - H.Z. Zarif Najafi, M. Moradi, S. Torkan, Effect of different surface treatment methods on the
shear bond strength of orthodontic brackets to temporary crowns, Int. Orthod. 17 (2019) 89–95.
https://doi.org/10.1016/j.ortho.2019.01.017. - I. Maryanchik, E.J. Brendlinger, D.W. Fallis, K.S. Vandewalle, Shear bond strength of
orthodontic brackets bonded to various esthetic Pontic materials, Am. J. Orthod. Dentofacial Orthop.
137 (2010) 684–689. https://doi.org/10.1016/j.ajodo.2008.06.031. - R. Blakey, J. Mah, Effects of surface conditioning on the shear bond strength of orthodontic
brackets bonded to temporary polycarbonate crowns, Am. J. Orthod. Dentofacial Orthop. 138 (2010)
72–78. https://doi.org/10.1016/j.ajodo.2008.08.030. - A. Tayebi, F. Fallahzadeh, M. Morsaghian, Shear bond strength of orthodontic metal brackets
to aged composite using three primers, J. Clin. Exp. Dent. 9 (2017) e749–e755.
https://doi.org/10.4317/jced.53731. - S.A. Yannikakis, A.J. Zissis, G.L. Polyzois, C. Caroni, Color stability of provisional resin restorative materials, J. Prosthet. Dent. 80 (1998) 533–539. https://doi.org/10.1016/s0022- 3913(98)70028-9.
- S. Rambhia, R. Heshmati, V. Dhuru, A. Iacopino, Shear bond strength of orthodontic brackets
- bonded to provisional crown materials utilizing two different adhesives, Angle Orthod. 79 (2009)
- 784–789. https://doi.org/10.2319/060908-298.1.
- I. Henriques, B. Seabra, S. Arantes‐ Oliveira, J. Portugal, Influência da técnica de acabamento
e do tempo de exposição na estabilidade cromática do bis‐ acrílico,
Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 55 (2014) 220–226.
https://doi.org/10.1016/j.rpemd.2014.10.002. - D.L.C. Masioli, M.Ad.O. Almeida, M.A. Masioli, J.R.Md. Almeida, Avaliação do efeito de
tratamentos superficiais sobre a força de adesão de braquetes em provisórios de resina acrílica. Dent.
Press J .Orthod. 16 (2011) 37–47. https://doi.org/10.1590/S2176-94512011000100008. - A. Pasquale, M. Weinstein, A.J. Borislow, L.E. Braitman, In-vivo prospective comparison of
bond failure rates of 2 self-etching primer/adhesive systems, Am. J. Orthod. Dentofacial Orthop. 132
(2007) 671–674. https://doi.org/10.1016/j.ajodo.2006.12.008. - F.M. Dias, C.R. Pinzan-Vercelino, R.R. Tavares, et al, Evaluation of an alternative technique
to optimize direct bonding of orthodontic brackets to temporary crowns, Dent. Press J. Orthod. 20
(2015) 57–62. https://doi.org/10.1590/2176-9451.20.4.057-062.oar. - Í.V.M. Tupinambá, P.C.C. Giampá, I.A.R. Rocha, E.M.C.X. Lima, Effect of different
polishing methods on surface roughness of provisional prosthetic materials, J. Indian Prosthodont.
Soc. 18 (2018) 96–101. https://doi.org/10.4103/jips.jips_258_17. - M.M. Suzuki, W. Custódio, V.F. Furletti, et al, Influência de diferentes tratamentos de
superfície na resistência ao cisalhamento de bráquetes colados em substrato resinoso, Braz. Oral Res.
32 (2018) 294. - C.S. Almeida, M. Amaral, F.D. de Cássia Papaiz Gonçalves, T.J. de Arruda Paes-Junior. Effect of an experimental silica-nylon reinforcement on the fracture load and flexural strength of bisacrylic interim partial fixed dental prostheses, J. Prosthet. Dent. 115 (2016) 301–305. https://doi.org/10.1016/j.prosdent.2015.08.009.
- S.H. Chay, S.L. Wong, N. Mohamed, A. Chia, A.U. Yap, Effects of surface treatment and
aging on the bond strength of orthodontic brackets to provisional materials, Am. J. Orthod.
Dentofacial Orthop. 132 (2007) 577.e7–577.11. https://doi.org/10.1016/j.ajodo.2004.01.024. - R.S. Fajardo, A. Muench, Tensile bond strength between denture base acrylic resin and acrylic
resin teeth, Rev. Odontol. Univ. São Paulo 11 (1997) 1–5. - S. Damade, S. Parlani, G. Beohar, Prosthetic management of obstructive sleep apnea. Guident.12 (2019) 18–20.
- Y.O. Zachrisson, B.U. Zachrisson, T. Büyükyilmaz, Surface preparation for orthodontic bonding to porcelain. Am. J. Orthod. Dentofacial Orthop. 109 (1996) 420–430. https://doi.org/10.1016/s0889-5406(96)70124-5.
- J.X. de Almeida, M.B. Deprá, M. Marquezan, L.B. Retamoso, O. Tanaka, Effects of surface
treatment of provisional crowns on the shear bond strength of brackets, Dent. Press J. Orthod. 18 (2013) 29–34. https://doi.org/10.1590/s2176-94512013000400006. - I.R. Reynolds, A review of direct orthodontic bonding, Br. J. Orthod. 2 (1975) 171–178.
https://doi.org/10.1080/0301228X.1975.11743666. - Y.S. Al Jabbari, S.M. Al Taweel, M. Al Rifaiy, et al, Effects of surface treatment and artificial
aging on the shear bond strength of orthodontic brackets bonded to four different provisional
restorations, Angle Orthod. 84 (2014) 649–655. https://doi.org/10.2319/090313-649.1. - H. Wang, G. Feng, B. Hu, et al, Comparison of flash-free and conventional bonding systems:
A systematic review and meta-analysis, Angle Orthod. 92 (2022) 691–699.
https://doi.org/10.2319/122221-932.1 - M. Delavarian, F. Rahimi, R. Mohammadi, M.M. Imani, Shear bond strength of ceramic and
- metal brackets bonded to enamel using color-change adhesive, Dent. Res. J. (Isfahan). 16 (2019) 233– https://doi.org/10.4103/1735-3327.261128.
FIGURE CAPTIONS
TABLE
Table 1. Median (minimum and maximum value) of shear bond strength (SBS) of ceramic brackets as a function of provisional restorative material, type of mechanical surface treatment, and chemical surface treatment using bonding agents.
Temporary restorative material Type of mechanical surface treatment Chemical surface treatment using bonding agents Transbond XT + Transbond Primer Resina Filtek Bulk Fill Flow + Single Bond Universal Duralay acrylic resin Duralay acrylic resin No roughening 15.09 (10.3–18.72) Cb 20.38 (11.6–20.9) Bb 32.24 (21.0–35.1) Aa Blasting with aluminum oxide 20.09 (18.32–21.2) Ba 21.26 (14.5–32.5) ABa 23.61 (19.0–28.4) Ab Drill spraying 21.76 (13.52–3.08) Aa 24.50 (20.6–28.0)Aa 22.15 (15.2–25.38) Ab Bis-acrylic resin No roughening *22.63 (1.20–20.4) Bb *23.72 (18.3–29.5) ABc *26.26 (21.6–38.6) Aa Blasting with aluminum oxide 22.64 (14.9–31.4) Bb *28.02 (22.15–34.8) Ab 21.66 (17.4–27. 24) Bb Drill spraying *25.38 (20.5–31.9) Ba *32.83 (25.8–39.8) Aa *24.69 (21.4–33.12) Ba
Figure 1 Composition chart of the materials used.
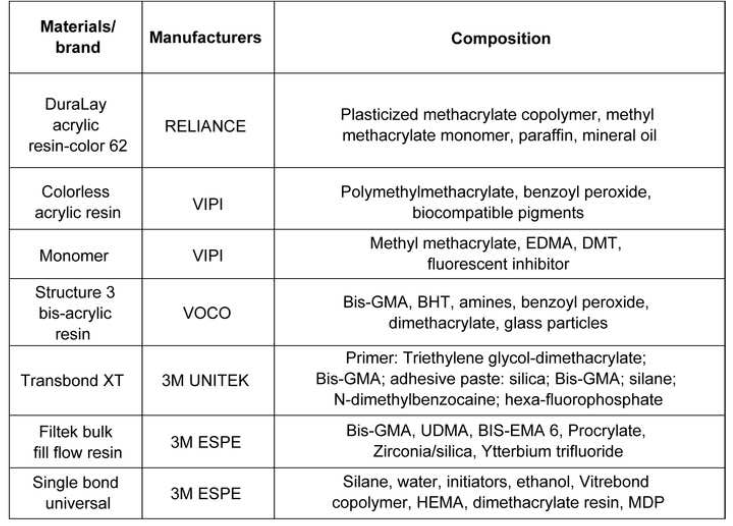
Figure 2 Experiment flowchart.
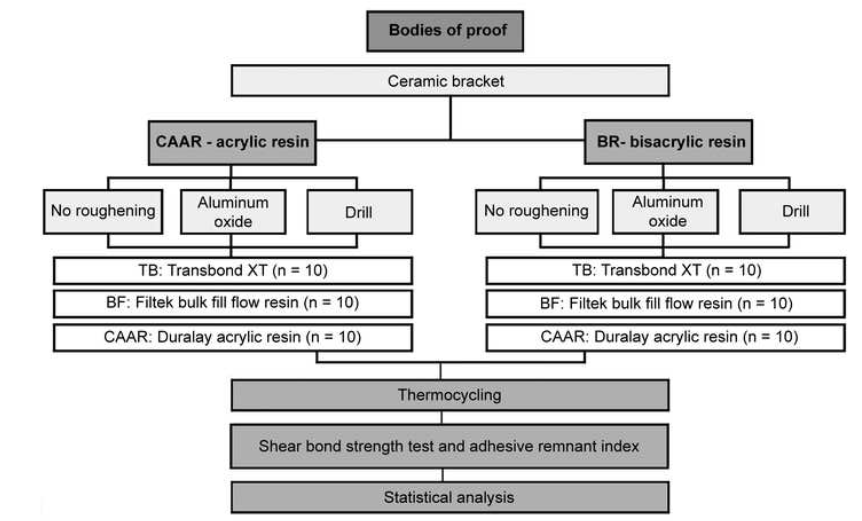
Figure 3 Specimen-surface preparation board.
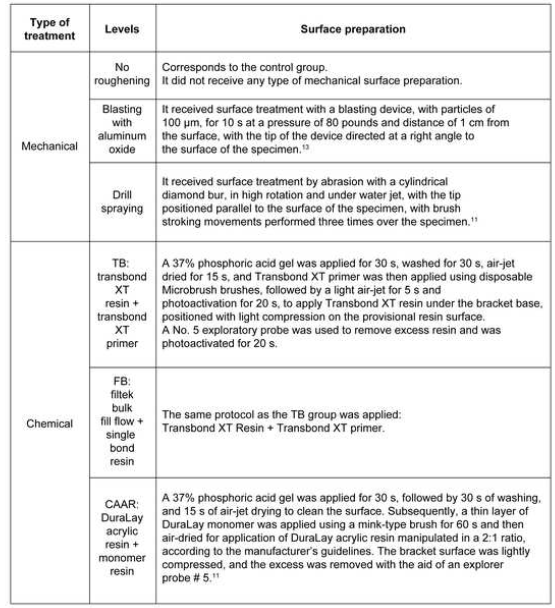
Figure 4 Specimen positioned in the universal testing machine (AME-5kN) for the SBS test.

Figure 5 Scores found in the study according to Artun and Bergland (1984). A, 0 points; B, 1 point; C,2 points; and D, 3 points.
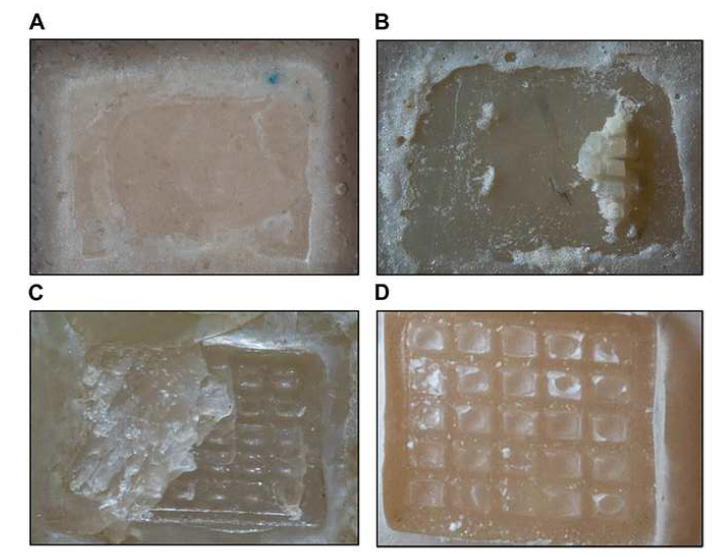
Figure 6 Adhesive remnant index.
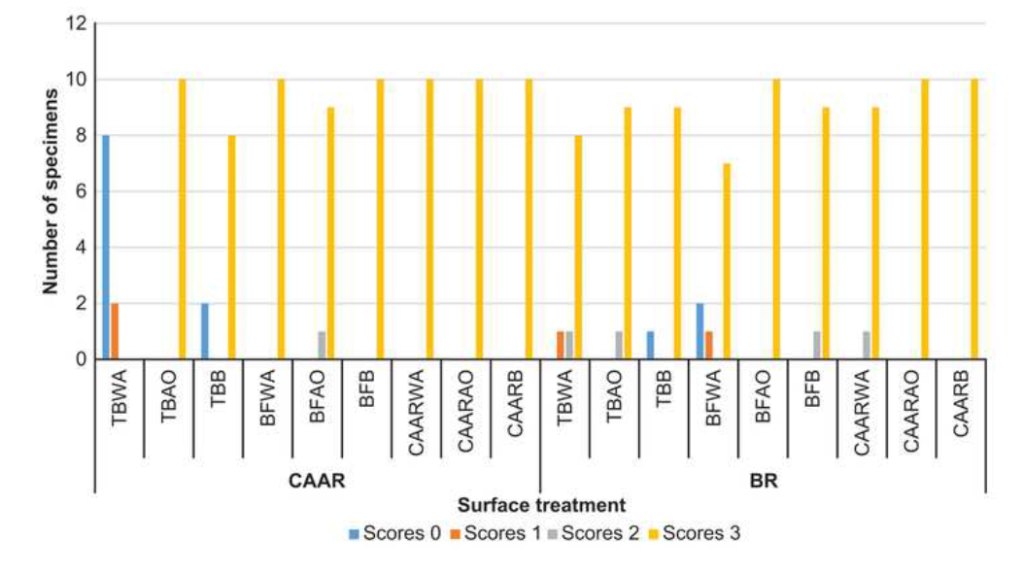
FONTE:
TBWA, Transbond without asperization; TBAO, Transbond with aluminum oxide; TBB, Transbond with bur; BFWA, Bulkfill Flow without asperization; BFAO, Bulkfill Flow with aluminum oxide;
BFB, Bulkfill Flow with bur; CAARWA. DuraLay acrylic resin without asperization; CAARAO,
DuraLay acrylic resin with aluminum oxide; CAARB, DuraLay acrylic resin with bur.
1Thiago Santos Mendes
Department of Orthodontics, FHO-Uniararas, Araras, Brazil. Maximiliano Baruto, 500. Jardim
Universitario. Araras- SP, Brasil.
E-mail: mendesodontologia@outlook.com
2 Department of Orthodontics, FHO-Uniararas, Araras, Brazil. Maximiliano Baruto, 500. Jardim
Universitario. Araras- SP, Brasil
guto_odonto@yahoo.com.br
3Department of Orthodontics, FHO-Uniararas, Araras, Brazil. Maximiliano Baruto, 500. Jardim
Universitario. Araras- SP, Brasil
anapaulatgodoi@yahoo.com.br
