REGISTRO DOI: 10.5281/zenodo.11003071
André Luís Viana Feitosa; João Vitor Craveiro Oliveira; Thiago Henrique Gonçalves Moreira; Isabel Cristina Quaresma Rego; Erick Neiva Ribeiro de Carvalho Reis; Giselle Maria Ferreira Lima Verde.
ABSTRACT
Introduction: Children and Young people (CYP) are diagnosed with cancer submitted to chemotherapy (CT) and radiotherapy (RT) potentially acquire complications such as mucositis, an inflammation capable of commit the enteral mucous. This study has the objective to evaluate the photobiomodulation therapy (PBMT) efficiency, the viability despite the management of the pediatric public, the promotion of quality of life (QoL) and the existence of adverse effects in oncopediatric patients with oral mucositis (OM), a specific involvement of mucositis in the mouth cavity. Methodology: This study is a literature review, using the research platforms of PubMed and Virtual Health Library (VHL). The filters applied were: Time interval between 2019 to 2023, the production should be complete and free access. Then, it was applied criteria of inclusion by reading the titles, abstracts and evaluation of the objectives. Results: 18 articles were contemplated for this review. Discussion: According to the results, it can be discussed about PBMT in CYP people involvement by OM who were submitted to CT or RT basing on: the methodology applied in the patients, the cooperation of the patients and their legal responsible, the analgesic effect, the healing induction, the impact for QoL and adverse effects. Conclusion: Based in the intel acquired, concludes the PBMT is a viable tool in oncopediatric patients accomited by OM because the beneficial effects can be acquired in short therm. However, the adverse effects of this therapeutic are inconclusive given that there are insufficient observational studies in long therm.
Keywords: Oral Mucositis, Cancer, Children, Low-Level Laser Therapy
RESUMO
Introdução: Pacientes infantojuvenis diagnosticados com câncer e submetidos à quimioterapia (QT) e à radioterapia (RT). Potencialmente adquirem complicações como a mucosite, uma inflamação capaz de acometer a mucosa enteral. Este estudo tem por objetivo avaliar a Terapia de Fotobiomodulação (TFBM) quanto a sua eficiência, a viabilidade devido aos manejos em pacientes infantojuvenis, a promoção de qualidade de vida (QdV) e a existência de efeitos adversos em pacientes pediátricos acometidos pela mucosite oral (MO), uma específica mucosite que acomete a cavidade bucal. Metodologia: Esse estudo é uma pesquisa de revisão literária utilizando as plataformas de busca Pubmed e Biblioteca Virtual de Saúde (BVS). Durante a pesquisa, filtrou-se os artigos pelas seguintes condições: intervalo de tempo de 2019 a 2023, o texto deveria estar completo, acessível gratuitamente. Por fim, houve critérios de inclusão pela leitura dos títulos, resumo e avaliação de premissas. Resultados : 18 artigos foram contemplados para esta revisão de literatura. Discussão: Conforme o resultado da pesquisa, pode-se discorrer acerca da TFBM em pacientes pediátricos acometidos de MO submetidos à RT e/ou QT de acordo com: a metodologia empregada nos pacientes, a cooperação dos pacientes e responsáveis à terapia, o efeito analgésico, a indução cicatricial, os benefícios à QdV, e os efeitos adversos. Conclusão: Com base nos resultados obtidos, conclui-se que a TFBM é uma ferramenta viável em pacientes oncopediátricos acometidos por MO. Os efeitos benéficos dessa terapia são observados a curto prazo. Porém, os efeitos adversos dessa terapêutica são inconclusivos haja visto que há insuficientes estudos observacionais à longo prazo.
Palavras-chave: Mucosite Oral, Crianças, Terapia à Laser de Baixa Potência
Cancer, its treatments and its complications are not a reality exclusive for adult patients. Because young patients that have age rate from 0 to 18 also are submitted to chemotherapy and radiotherapy with finality to remiss that pathology (Nunes, et al. 2020; Neves, et al. 2021).
In detriment of these treatments, oncopediatric patients (OP) frequently have complications like mucositis, which is an inflammatory condition that manifests in enteral mucous in consequence of systemic effects by chemotherapy or local irradiation by radiotherapy (Neves, et al. 2021), one case of these mucositis is the oral mucositis (OM), which occurs in the oral cavity(Ludovichetti, et al. 2023).
An OM is a condition that depletes significantly the well-fare of oncopediatric patients. This complication promotes an oral and throat painful symptomatology, therefore, dysphonia and dysphagia. Consequently, debilitates the immunity which propitiates opportunistic infections (Anschau, et al. 2019)
Because of this situation, researchers elaborate protocols that prevents or treat OM, between these works, there is the low-level laser therapy (LLLT). Therapy which benefits is anti-inflammation, analgesia, and tissue repair promotion (Heimlich, 2023).
By this exposition, this research evaluates LLLT efficiency, its viability with the management reality of pediatric patients, its effects on quality of life (QoL) and the existence of any side-effects in its utilization in juvenile patients affected by OM.
And, in face of this objective, this scientific production has the finality to sane these following hypotheses: low-level laser (LLL) is viable with the exigences of the management of pediatric patients; it promotes betterment in QoL by the reduction of symptoms and signals; and, there are reports of side-effects on that public, such as complications with oncological treatment.
By the results of this production, the LLLT in OP, its benefits and restrictions shall have even more scientific fundaments.
II Material and methods
This scientific production is a literature review. And the methodology utilized for this work was a data gathering in the PubMed and the Virtual Health Library (VHL) research tools.
First, the planning of this study was designed following the principles of the Table 1 which are: Research population of children and young adults with maximum 18 years old with OM due to CT or RT, its complication treated with LLLT, compared with others therapies for OM and the LLLT results.
Table 1: PICO strategy utilized for the article gathering about PBM in pediatric patient suffering oral mucositis, modified by reference of Redman, Harris e Phillips (2022)
P (Population) Children and Young Adults with 18 years old max I (Intervention) Any method of LLLT utilized to prevent or treat oral mucositis C (Comparison) Patients treated with Other techniques for OM O (Outcome) Consider results (but not exclusively) like OM, pain, adverse-effects, etc.
Also consider results such as:
Interruption of cancer treatment
Pain in a scale from 0 (no pain) to 10 (intense pain) QoL
Diet (if it had any change with the patient nutrition)
Hospitalization time
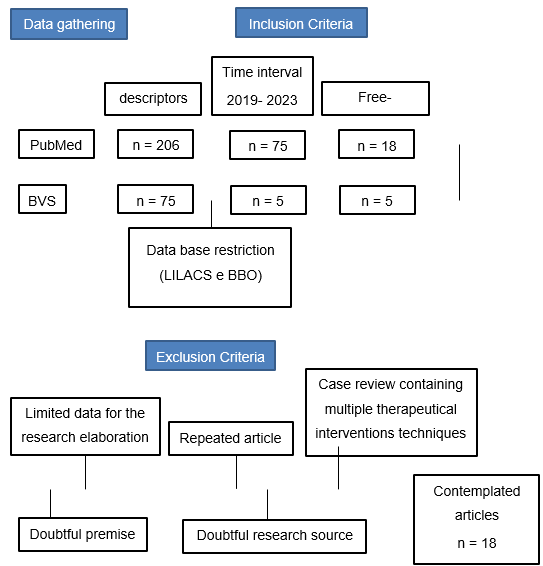
Utilizing the descriptors presented in the first column of Table 2, it was gathered 206 articles on PubMed and 75 on VHL, totalizing 281 productions.
In next step, the research was delimited for the base data of VHL only to LILACS and BBO. By this way, reduced the articles disponible on VHL to 7. In detriment of this, plus the PubMed finds, it was totalized 213 productions acquired.
To finish, inclusion criteria were applied in order of the second column of Table 2. In this way, it was included complete articles, then those which was freely-available, at last, those which contained title, abstract and a text in accordance with the strategy demonstrated on Table 1.
Table 2: Descriptors and inclusion criteria for article gathering
Descriptors Inclusion Criteria Oral mucositis Complete text LLLT Time interval of 2019-2023 Children Freely-available Title Abstract Compatible text premises English or Portuguese
After this process, it was obtained 23 articles, then, applied the exclusion criteria illustrated on table 3, respectively demonstrated by its chronological order, which restricted the data to 18 productions that were used to fundament this review.
Table 3: Exclusion criteria to delimitate the contemplated articles
Exclusion Criteria Exclusion of Medline data base on the research in the BVS platform Case review containing multiple therapies Doubtful research source Scarse data for analysis in a research Doubtful premise Repeated article
Flowchart 1: Methodology utilized for each stage with the respectively.
III Results
The results of this research were 18 articles found utilizing PubMed and VHL database. 11 of those productions which is strictly directed with the objectives of this research, on a single table (Table 4), were didactically ordained by each publication year and with their data properly organized by each column respectively demonstrating: Author, Title, Outcomes, Conclusions. While the others 7 text were properly devolved (as well as the contemplated in the Table 4) in the discussion.
Table 4: Article contemplated to evaluate the utilization of PBM on young patients accomited by OM
Authors/Year Title Patients ages Results of PBM treatment on OM Conclusion Tomaževič, T. et al. 2019 Optimization of Photobiomodulation Protocol for Chemotherapy-Induced Mucositis in Pediatric Patients Dp de 11 anos PBM offers quicker tissue healing.Preventive PBM benefits less severity of mucositis. OM severity significantly reduced by PBM; Noirrit-Esclassan, E. et al. 2019 Photobiomodulation with a combination of two wavelengths in the treatment of oral mucositis in children: The PEDIALASE feasibility study. 3 – 18 years No side-effects notified.Pain relief 2h after therapy session.Improved healing on tissue. Combination of two exposures methods is viable;. LLLT is atraumatic, non-invasive and well received by young patients. Bardellini, E. 2020 Photobiomodulation therapy for the management of recurrent aphthous stomatitis in children: clinical effectiveness and parental satisfaction 5- 12 years Does not apply Parents and children were very collaborative despite the routine that the therapy demanded. Obs.: This study evaluated the PBM on aphthous lesions. Still, this is relevant because of LLLT applicability despite pediatric management. Nunes, L. F. M. et al. 2020 Prophylactic photobiomodulation therapy using 660 nm diode laser for oral mucositis in paediatric patients under chemotherapy: 5-year experience from a Brazilian referral service. 8 months to 17 years Lower probability of opportunistic infectionsPrevents OMPromotes pain relief LLLT is efficient and safe for both children and teenager submitted to CT. Guimaraes, D. M. et al. 2021 Low-level laser or LED photobiomodulation on oral mucositis in pediatric patients under high doses of methotrextate: prospective randomized, controlled trial. 9,4 years average Prevents OM on patients submitted to MTX treatment.Significative pain reduction after 4 days of therapy. LLLT reduced period and intensity of pain.LEDT is a safe and low-cost alternative to LLLT Neves, et al. 2021 : Low-level laser therapy for oral mucositis in children with cancer: a meta-analysis & systematic review considering safety and efficacy < 18 years Prevents OM and its aggravation.Reduction of hospitalization by OM. PBM is safe on pediatric patients as well as on adults;The large number of protocols of LLLT difficult an accurate procedure.Patients that weren’t submitted to PBM had severer intensity of OM Patel, P. et al. 2021 Clinical practice guideline for the prevention of oral and oropharygeal mucositis in pediatric cancer and hematopoietic stem cell transplant patients: 2021 update 0-7 years Reduced severed cases of OM.Reduced exigence of opioids analgesic therapy.No adverse-effects notified. LLLT is indicated for both prevention and treatment of OM caused by CT and/or RT in oncopediatric patients.Authors suggest the utilization of λ ≈ 620- 750 nm. AlqahtanI, S. S. Khan, S. D. 2022 Management of oral mucositis in children ≤ 18 years Lesions sites exposed by laser had significantly less pain than control sites;Pain reduction after 1 to 2 days of therapy;No side-effects notified. OM severity reduced. Ludovichetti, F. S. et al. 2022 Evaluating high power laser therapy (HPLT) as treatment for chemotherapy-induced oral mucositis in pediatric patients with oncohematological diseases. 5 – 16 years PBM unlikely has carcinogenic effects. PBM reduces hospitalization period;LLLT analgesic effects reduce the demands of opioids. Fiwek, P. et al. 2022 Photobiomodulation Treatment in Chemotherapy-Induced Oral Mucositis in Young Hematological Patients – A Pilot Study. 3 – 18 years Analgesic effects improved after each therapy session. Extraoral technique more viable for children;. Despite the success of multiple procedures. Authors affirm that researches should be applied for better understanding of multiple parameters of PBM utilization and what effects they imply. Hafner, D. et al. 2023 Photobiomodulation for Chemotherapy-Induced Oral Mucositis in Pediatric Patients 0- 18 years Pain relief reported by all trials evaluatedOM severity reduced Pediatric patients more susceptible for OM than adults;PBM safe, applicable and efficient for this public;Research indication for parameters adaptations for young patients.
IV Discussion
IV.I Oncopediatric patients difficult
Cancer and its treatments aren’t a reality exclusive for adult patients. This is because even infant juvenile patients from 0 to 18 years old age also receives chemotherapy (CT) and radiotherapy (RT) objectively to withstand this disease. Therefore, complications such as oral mucositis is frequent in that public (Alqahtani e Khanz. 2022; Neves. 2021; Nunes. 2020).
Mucositis is an inflammation that occurs in the whole enteral mucous. In case of CT, that side effect appears because of the therapy with systemic utilization hematopoietic stem cell transplantation (HPSCT) or methotrexate (MTX)(Neves. 2021). In case of RT, because of the immunosuppression caused by the local irradiation(Hafner, et al. 2023). Consequently, these kinds of stresses submitted especially to the oral cavity, provokes oral mucositis (OM).
The manifestation of OM is observed after 2 to 18 days after the start of oncological treatment(Alqahtani e Khanz. 2022). In sight of this problem, it is relevant to mention the severity of this involvement because OM deeply harms its patients with pain (Alqahtani e Khanz. 2022; Capellanes, et al. 2021; Heimlich. 2023; Legouté, et al. 2019; Kauark-Fontes, et al. 2022. Redman, Harris, Phillips. 2022).
In consequence of the intolerable level of pain, the patients devolve dysphonia (Kauark-fontes, et al. 2022), which is the difficulty to communicate, and dysphagia (Kauark-fontes, et al. 2022), which is the difficulty to swallow. In consequence of the pain to swallow, oncological pediatric patients are submitted to enteral and parenteral nutrition by probes. Also, the pain intensity submits those patients to use potent opioids, consequently, to be exposed to their debilitating adverse-effects.
Also, because of these multiple nuances of complications, opportunistic infections in the ulceration can occurs by the immunosuppression (Patel, et al. 2021). Other than the algic symptoms, the OM and bacteremia induce a suspension the CT and/or RT, so, it prolongs the hospitalization period, the resource costs and worse the patient prognostic(Patel, et al. 2021).
Otherwise, is important to mention that OM is more debilitating in young patients than in adults. This is because this public has a higher mitotic activity, therefore, they are more sensible for CT and RT adverse-effects (Hafner, et al. 2023). In conclusion, this case scenario provokes a deep psychological stress in both parents and patients (Redman, Harris and Phillips. 2022).
IV.II Photobiomodulation tech
IV.II.I Theory principles
Photobiomodulation (PBM), or, Low Level Laser Therapy (LLLT) as known in the past, has effects in an intracellular level (Legouté, et al. 2019). This can be explained because different laser levels induce different cellular components, for example: the intracellular water can be energized with wave lengths of 400-450 nm, in consequence of this effect, it acts in the calcium ions transportation. Meanwhile, lipidic structures are energized by wave lengths between 900-1000 nm (Amaroli, et al. 2022).
IV.II.II Mechanism of Action
The PBM effects are achieved by the irradiation of cellular structures by the laser emitted from the device. Which it results in the betterment of cellular respiration, of Ca2+ pump mechanisms, of redox homeostasis, of apoptosis process, and, consequently, notoriously impacts in the tissue proliferation at clinical levels (Amaroli, et al.2022).
IV.II.III General effects
The PBM therapeutical effects basically are: analgesia, anti-inflammation and promotes tissue healing. Therefore, optimal not only for treatment but lesions prevention as well (Patel, et al. 2021).
IV.III Photobiomodulation on oncopediatric patients accomited by oral mucositis
According to the found text analysis, this research can be didactically and in order, discus about PBM on oncopediatric patients accomited by OM submitted to CT and/or RT in the following subjects: the methodology applied on the patients, the parameters utilized in the devices, the cooperation of the patients and their respective legal guardians, the effect on the tissue healing, the impact on the QoL, and adverse-effects.
IV.III.I Viability
First, is important to mention that PBM is viable for preventing OM. This affirmation fundaments itself on the indications of Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO) (Fiwek, et al. 2022).
Those indications can be well illustrated by the data found in Hafner, et al (2023) research that indicates a minor occurrence of OM for patients submitted to prophylactic PBM, and, when occurred, the candidates have been benefited by a less severe level that complication (Hafner, et al. 2023).
Also, is necessary to highlight the frequently mention of the seventh day utilized to evaluate the therapy progress in a such way that can verify the tissue lesion remission and analgesia in patients (Tomačevič, et al. 2020).
IV.III.II Parameters configuration for OM
Parameters utilized are frequently mentioned as eclectics, thus, vary the results. This is explained by the categories of parameters divided in: wave length (between 600 to 1070 nm), power (between 150 to 1500 mW) energy dispersion, also called energy intensity (between 4.5 to 26,8 J/cm²), session frequency (frequently daily or each 2 days), the laser application method (by irradiating the whole cavity or only the affected region; direct laser contact or not, and intra or extraoral irradiation) (Alqahtani e Khan. 2022; Hafner, et al. 2023)
These parameters, even though it can be applied in children and young public as well as in adults, difficult the elaboration of specific protocols for the management reality and the biological individuality of the pediatric patients (; Redman, Harrise Phillips. 2022; Ludovichetti, et al. 2023).
Meanwhile, the variety of parameters permits for professionals to adapt for each case. This premise is explained by, even though PBM is well received by a significantly number of patients (Noirrit-Eclassan, et al. 2019; Bardellini, et al. 2020; Tomačevič, et al. 2020), there are reports that evidence that patients under 7 years old are prone to no cooperate due to refuse of using opaque google, a personal protective equipment necessary for the treatment(Noirrit-Eclassan, et al. 2019).
IV.III.III Treatment collaboration
Otherwise, about the treatment collaboration, both patients and parents had an excellent attendance to the sessions, even if they were daily (Noirrint-Eclassan, et al. 2019; Bardellini, et al. 2020; Tomačevič, et al. 2020). This phenomenon is explained by the impact the pathologies have in the QoL of the patients as well as the efficiency that PBM can be applied to the young accompanied with the benefits the treatment can promotes(Bardellini, et al. 2020).
IV.III.IV Effectiveness
Even though the meta-analysis promoted by Anschau, et al. (2019) that affirms that there are not enough evidences that supports the PBM intervention on children and teenagers, is important to announce the benefits by others researches. This is based on the frequently reports of the severity of the OM lesions followed by the anti-inflammation, analgesia, then the betterment of QoL of the subjects (Noirrit-Eclassan, et al. 2019; Nunes, et al. 2020; Tomačevič, et al. 2020; Guimaraes, et al. 2021; Neves, et al. 2021; Patel, et al. 2021; AlqahtanI e Khan. 2022; Fiwek, et al. 2022; Kauark-fontes, et al. 2022; Redman, Harris e Phillips. 2022; Hafner, et al. 2023; Ludovichetti, et al. 2023).
These benefits make possible the reduction of aggressive medicine treatment in fact that OM usually requires opioids for pain remission and non-steroidal anti-inflammatory drugs (NSAID) to intervein in the clinical condition (Guimaraes. 2021).
To conclude, the PBM interferes positively in the patient nutrition. This is caused by the remission of symptomatology severity on the subjects submitted for the treatment therefore dismiss the parenteral nutrition (Nunes, et al. 2020; Redman, Harris e Phillips. 2022).
IV.III.V Adverse-effects
Even with the number of researches made, there is insufficient reports about adverse-effects of PBM. According to Amaroli, et al. (2022) researches, the physiological principle of low-level laser irradiation also can affect the cancer cellular proliferation. Although, there is a possibility that these effects are minimal on humans(Kauark-fontes, et al. 2022. Redman, Harris and Phillips. 2022), in consequence of this, there is conflicting data about adverse-effects with the conclusion that they insignificantly alter the survival rate of those treated for cancer (Anschau, et al. 2019; Fiwek, et al. 2022; Noirrit-Eclassan, et al. 2019). Still, there is authors that suggest that randomized clinical essays should be performed with a long-term criteria observation (Redman, Harris and Phillips. 2022).
V Conclusion
In light of the acquired information by this review, it can be concluded that OM can highly harm the QoL of pediatric patients by:
1) severe pain;
2) then dysphagia;
3) therefore, dietary prejudice;
4) resulting in opportunistic infections;
5) and a longer hospitalization time;
6) and resources costs.
In hope to soft this reality, the LLLT:
7) is a technique that is viable despite the management demands on oncopediatric patients;
8) reduces pain;
9) promotes anti-inflammatory tissue responses;
10) a significantly healing promotion effects;
11) reduces opioids demands by its patients;
12) Has notorious effects after 2-3 days.
But, the PBM on OM has downsights such as:
13) Possibility of induce cancer cells proliferation then prolongate the oncological treatment;
14) Few researches evaluating in long-time the possibility of adverse-effects;
15) Multiple parameters with very few researches evaluating what each configuration implies;
16) Few protocols that are adapted for the management of pediatric patients, such as session periods, and frequency of treatment.
Therefore, it is relevant that these matters should be researched carefully.
VII Literature
ALQAHTANI, SS, KHANZ. Management of oral mucositis in children. European Review for Medical and Pharmacological Sciences, v. 26, p. 1648- 1657, 2022.
AMAROLI, A. et al. A Narrative Review on Oral and Periodontal Bacteria Microbiota Photobiomodulation, through Visible and Near-Infrared Light: From the Origins to Modern Therapies. International Journal of Molecular Sciences, v. 23, n. 3, p. 1372 – 1398, 2022.
ANSCHAU, F. et al. Efficacy of low-level laser for treatment of cancer oral mucositis: a systematic review and meta-analysis. Lasers in Medical Science, 2019. DOI: https://doi.org/10.1007/s10103-019-02722-7.
BARDELLINI, E. et al. Photobiomodulation therapy for the management of recurrent aphthous stomatitis in children: clinical effectiveness and parental satisfaction. Medicina oral, patologia oral y cirurgía bucal, v. 25, n. 4, p. 545- 553, 2020.
CAPELLANES, THB. et al. Photobiomodulation therapy for oral mucositis management in head and neck cancer patients undergoing radiotherapy: case reports. Rio de Janeiro Dental Journal, v. 6, n. 3, 2021.
FIWEK, P. et al. Photobiomodulation Treatment in Chemotherapy-Induced Oral Mucositis in Young Hematological Patients – A Pilot Study. Revista Medicina, v. 58, n. 1023, 2022. DOI: https://doi.org/10.3390/medicina58081023.
GUIMARAES, DM. Low-level laser or LED photobiomodulation on oral mucositis in pediatric patients under high doses of methotrextate: prospective randomized, controlled trial. Supportive Care in Cancer. 2021. DOI: https://doi.org/10.1007/s00520-021-06206-9.
HAFNER, D. et al. Photobiomodulation for Chemotherapy-Induced Oral Mucositis in Pediatric Patients. Biomolecules, v. 13, p. 418- 433, 2023.
HEIMLICH, FV. Proposta de novo protocolo de Fotobiomodulação profilática para mucosite oral e orofaríngea induzida por quimioterapia: um estudo clínico randomizado. 2023. Dissertação (Mestrado) – Faculdade de Odontologia, Universidade Federal de Minas Gerais, Belo Horizonte, 2023.
KAUARK-FONTES, E. et al. Extra oral photobiomodulation for prevetion for oral and oropharyngeal oral mucositis in head and neck patients: interim analysis of a randomized, double-blind, clinical trial. Supportive Care in Cancer, v. 30, p 2225- 2236, 2022.
LEGOUTÉ, F. et al. Low-level laser therapy in treatment of chemoradiation-induced mucositis in head and neck cancer: results of a a randomised, triple blind, multicenter phase III trial. Radiology Oncology, v. 14, p. 83- 94, 2019.
LUDOVICHETTI, FS. et al. Evaluating high power laser therapy (HPLT) as treatment for chemotherapy-induced oral mucositis in paediatric patients with oncohematological diseases. International Journal Paediatry Dentistry, v. 33, p. 269- 277, 2023. DOI: 10.1111/ipd.13050.
NEVES, L. J. Avaliação do Efeito do Laser Preventivo na Mucosite Oral Quimioinduzida em Pacientes Submetidos a Altas Doses em Metotrexato. Revista Brasileira de Canceriologia, v. 67, n. 1, 2021.
NOIRRIT-ECLASSAN, E. et al. Photobiomodulation with a combination of two wavelengths in the treatment of oral mucositis in children: The PEDIALASE feasibility study. Archives de Pédiatre, v. 26, p. 268- 274 2019. DOI: https://doi.org/10.1016/j.arcped.2019.05.012.
NUNES, LFM. et al. Prophylactic photobiomodulation therapy using 660 nm diode laser for oral mucositis in pediatric patients under chemotherapy: 5-year experience from a Brazilian referral service. Lasers in Medical Science, 2020. DOI: https://doi.org/10.1007/s10103-020-03060-9.
PATEL, P. et al. Clinical practice guideline for the prevention of oral and oropharyngeal mucositis in pediatric cancer and hematopoietic stem cell transplant patients: 2021 update. European Journal of Cancer, v. 154, p. 92- 101, 2021.
REDMAN, M. G. HARRIS, K. PHILLIPS, B. S. Low-level laser therapy for oral mucositis in children with cancer. Archives of Diseases in Childhood, v. 107, p. 128- 133, 2022. DOI: 10.1136/archdischild-2020-321216. TOMAŽEVIČ, D. M. D. et al. Optimization of Photobiomodulation Protocol for Chemotherapy-Induced Mucositis in Pediatric Patients. Photobiomodulation, Photomedicine, and Laser Surgery, v. 20, n. 20, 2020. DOI: 10.1089/photob.2019.4794.
