OBSTÁCULOS PREDOMINANTEMENTE ENCONTRADOS PELA EQUIPE MULTIPROFISSIONAL NO MANEJO DA SEDAÇÃO PALIATIVA NA UNIDADE DE TERAPIA INTENSIVA
REGISTRO DOI: 10.5281/zenodo.8432668
Rodrigo Marques Barreto Da Costa¹
Bruna Thaysa de Lima Tavares²
Lorena Mayara do Amaral³
Sara de Moraes Simirio4
Ana Carolina Aguirres Braga5
Matheus Fellipe Alves Justo6
Francisca Lucilene Rocha dos Santos7
Maria Carolina Jovem Montalvão8
Dhamacynho César de Lima Peres9
Raissa Mayara da Silva Dantas10
Lucas dos Anjos Sena¹¹
Anderson Brandão dos Santos¹²
Állef Diego Bonfim de Andrade¹³
ABSTRACT
Introduction: Palliative Care (PC) plays a crucial role in improving the quality of life for individuals facing advanced chronic illnesses, especially when they are in the Intensive Care Unit (ICU). Multiprofessional involvement is of utmost importance in this context, as it addresses the complex physical, mental, and emotional needs of patients and their families during this fragile process. In many cases, individuals under PC may require the use of palliative sedation to manage end-of-life pain and other symptoms, which demands specialized and integrated care from the ICU healthcare team. Objectives: To identify and discuss the main practices and approaches of the multiprofessional team in the management of palliative sedation in patients under palliative care in the Intensive Care Unit, as well as effective methods to improve them. Methodology: An Integrative Literature Review was conducted using the PubMed, Embase, Web of Science, and BVS databases. The research question was, “Do (Population) professionals in services providing care in ICUs (Intervention) that promote palliative care services in ICUs (Outcomes) use what approaches for palliative sedation management in these patients?” The descriptors used were “((Palliative Care OR Palliative sedation) AND (sedation) AND (Intensive Care Unit) AND (Patient Care Team OR Multiprofessional Team OR Multiprofessional Health Team)).” Articles in all languages were included, with a focus on those published between 2013 and 2023. Exclusion criteria included articles that did not have the search terms in their titles or abstracts and articles not addressing the central issue of our study. Results: Pain management in patients undergoing palliative care in the intensive care unit involves multiprofessional approaches aimed at providing effective pain relief, proper utilization of palliative sedation, and end-of-life comfort. In this context, the integration of medical teams, nursing, psychologists, and physiotherapists plays a fundamental role in the pharmacological analgesia of these patients. Conclusion: Interdisciplinary assessment of pain, combined with appropriate medication administration and the proper incorporation of palliative sedation, has proven to be effective in optimizing patient comfort and promoting a good death.
Keywords: Palliative Care. Sedation. Intensive Care Unit. Healthcare professional.
RESUMO
Introdução: Os Cuidados Paliativos (CP) desempenham um papel crucial na melhoria da qualidade de vida de indivíduos que enfrentam doenças crônicas avançadas, especialmente quando estão na unidade de terapia intensiva (UTI). A atuação multiprofissional é de suma importância neste contexto, pois atende às complexas necessidades físicas, mentais e emocionais dos pacientes e também suas famílias nesse processo de fragilidade. Em diversos casos indivíduos sob CP podem necessitar da utilização da sedação paliativa para o manejo da dor e outros sintomas de fim de vida, o que demanda um cuidado especializado e integrado da equipe assistencial a UTI. Objetivos: identificar e discutir os principais práticas e abordagens da equipe multiprofissional no manejo da sedação paliativa em pacientes sob cuidados paliativos na Unidade de Terapia Intensiva, assim como os métodos eficazes para melhorá-los. Metodologia: Foi feita Revisão Integrativa da Literatura realizada nas bases de dados PubMed, Embase, Web Of Science e BVS. A pergunta de investigação foi: “(Population) Em profissionais de serviços que prestam serviços em UTIs (Intervention) que promovem os serviços de cuidados paliativos na UTIs (Outcomes) utilizam quais abordagens para o manejo sedação paliativa nesses pacientes?” Os descritores utilizados foram: “((Palliative Care OR Palliative sedation) AND (sedation) AND (Intensive Care Unit) AND (Patient Care Team OR Multiprofessional Team OR Multiprofessional Health Team))”. Foram inclusos artigos em todos os idiomas sem recorte temporal, mas dando privilégio aos artigos publicados entre 2013 e 2023. Critérios de exclusão: artigos que não tivessem os termos de pesquisas no título ou nos resumos e artigos sem foco na problemática central do nosso estudo. Resultados: O manejo da dor em pacientes submetidos a cuidados paliativos na unidade de terapia intensiva envolve abordagens multiprofissionais que visam proporcionar alívio eficaz da dor, utilização adequada da sedação paliativa e um conforto de fim de vida. Nesse contexto, a integração de equipes médicas, de enfermagem, psicólogos e fisioterapeutas desempenha um papel fundamental na analgesia farmacológica dos desses doentes. Conclusão: A avaliação interdisciplinar da dor, combinada com a administração adequada de medicamentos e a incorporação apropriada da sedação paliativa demonstram ser eficazes na otimização do conforto do paciente na promoção de uma boa morte.
Palavras-chave: Cuidados Paliativos. Sedação. Unidade de Terapia Intensiva. Profissionais de Saúde.
Introduction
The performance of the multiprofessional team is of utmost importance in the Intensive Care Unit (ICU) when it comes to palliative care (PC). This team, which may include physicians, nurses, physiotherapists, nutritionists, psychologists, social workers, and other healthcare professionals, works together to provide pain relief, manage symptoms, offer emotional support, and enhance the well-being of end-of-life patients.(1,2).
The multiprofessional approach aims not only to manage clinical aspects but also to address the biopsychosocial needs of patients and provide comprehensive care to their families. This holistic care can not only offer a peaceful death to the patient in intensive care but also enhance the well-being of the families during this vulnerable period. (3–5).
Palliative sedation plays an essential role in PC in the ICU, managed by the multiprofessional team. Its purpose is to alleviate suffering, improve and enhance the well-being of patients in terminal stages, providing comfort and tranquility while enabling a comprehensive and compassionate approach to their physical and emotional needs.(2,6).
In this context, the rationale and relevance of this research lie in identifying the obstacles that may arise in the management and administration of palliative sedation and how collaboration among health professionals can be optimized to overcome these challenges. More directly, our intention is to develop successful approaches that not only enhance clinical care related to pain relief through palliative sedation but also elevate the quality of care offered to patients under PC, ensuring a more comprehensive and empathetic assistance.
Therefore, the following study had, as its guiding question: What approaches does the multidisciplinary team that promotes palliative care in ICUs use to manage palliative sedation in these patients? Thus, the objective of the research was to identify and discuss the main practices and approaches of the multidisciplinary team in the management of palliative sedation in patients under palliative care in the Intensive Care Unit, as well as effective methods to improve them.
Methodology
This is an integrative literature review (ILR) in which an initial question was formulated according to the PICO strategy, in this specific case, PI(C)O (7): “(Population) Healthcare professionals providing services in ICUs (Intervention) and promoting palliative care (Outcomes) use what approaches in the management of palliative sedation in these patients?”
The literature search was conducted on the PubMed, Embase, Web Of Science, and BVS databases. The following descriptors were used: “((Palliative Care OR Palliative sedation) AND (sedation) AND (Intensive Care Unit) AND (Patient Care Team OR Multiprofessional Team OR Multiprofessional Health Team)).”
The search for studies was conducted in journals without a specific time frame, but with an emphasis on studies published between 2013 and 2023 in all languages. The included study types were meta-analyses, randomized and non-randomized clinical trials, integrative and systematic reviews, and case reports that were published and indexed in the mentioned databases.
As exclusion criteria included studies involving patients under the age of 18, articles that did not contain the search terms in their titles, abstracts, or full text, and those that were not freely accessible. Additionally, articles that did not directly relate to the study’s focal question were excluded.
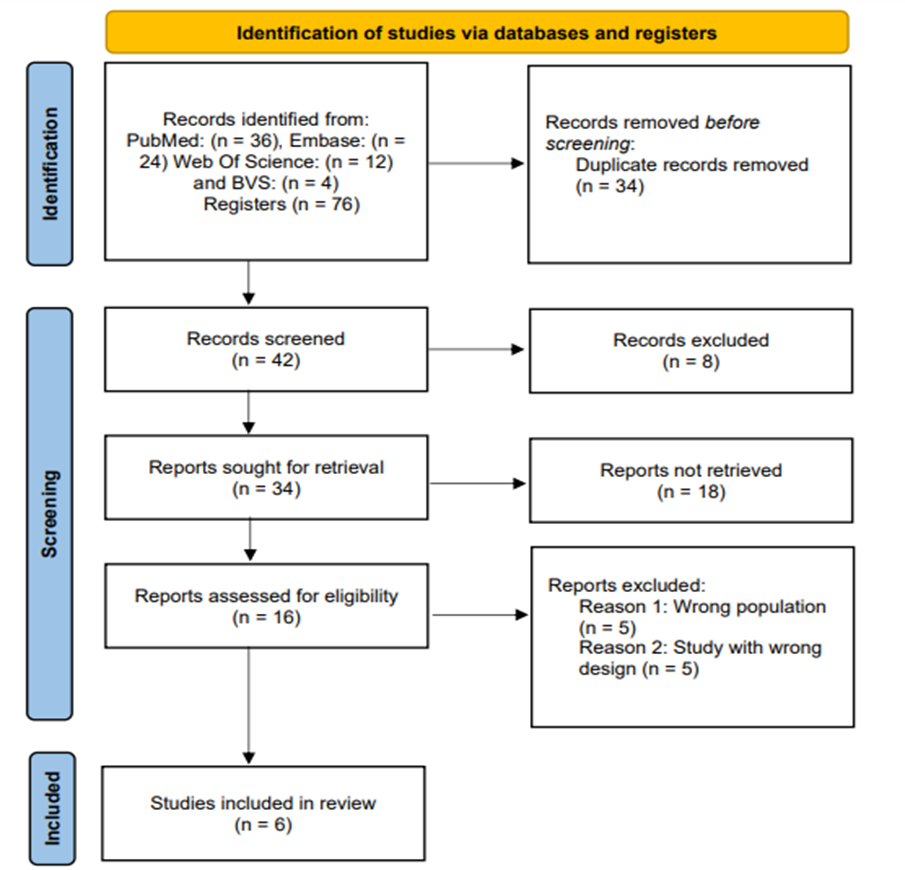
Initially, 76 articles were found, and after applying the criteria mentioned above and conducting a floating reading, 14 articles were selected. Of these, 6 articles were subjected to a thorough examination, critical appraisal, and knowledge synthesis. These 6 articles served as the basis for this Integrative Review of Literature, as outlined in Figure 1 following the PRISMA Flow Diagram. (8).
Figure 1: Prisma Flow Diagram
Two reviewers utilized the recommendations developed by the Joanna Briggs Institute (JBI) (7) To extract data from the articles included in the Integrative Review of Literature (IRL), two reviewers used the recommendations developed by the Joanna Briggs Institute (JBI). They collected information including the authors, the year of publication, the type of study, the objectives of the articles, the critical evaluation performed, and the main results relevant to the question addressed in our IRL.
In order to ensure a rigorous assessment of each article, critical analysis tools were applied to ensure a thorough review of each selected study in terms of its reliability and relevance.
Results
The selection of articles for this research consists of six publications that meet the eligibility criteria established earlier. These criteria were defined to ensure that these articles adequately addressed the research question, as listed in Table 1.
Table 1. Distribution of studies based on authors, study type, and objectives.
Author/Year Study Model Article Title Objective Prado, et. al. (2018) Retrospective Cohort Continuous palliative sedation for patients with advanced cancer at a tertiary care cancer center Assess the frequency, clinical indications, and outcomes of Psychosis Syndrome in patients with advanced cancer admitted to our comprehensive tertiary cancer center. Dorze et. al. (2019) Informative Article Deep continuous sedation maintained until death, in French Intensive Care Units Explore the implementation and implications of the Clayes Leonetti Law, a French law related to end-of-life situations that establishes the right to “deep and continuous sedation that leads to an alteration of consciousness and is maintained until death.” Bruce & Boston (2011) Narrative Review Relieving existential suffering through palliative sedation: discussion of an uneasy practice Present a discussion on the complex nature of palliative sedation in the treatment of existential suffering to highlight and contribute to the growing debates surrounding this multifaceted and ethically charged practice. Effendy et. al. (2022) Scope Review Barriers and facilitators in the provision of palliative care in adult intensive care units: a scoping review Explore and synthesize research that has identified barriers and facilitators in the delivery of palliative care in the ICU. Schur et. al. (2016) Retrospective Observational Sedation at the end of life – a nation-wide study in palliative care units in Austria Investigate the practice of end-of-life sedation in palliative care units in Austria. The study aimed to identify patient characteristics who received sedation, indications for sedation, duration, and the most commonly used medications, as well as to compare the characteristics of sedated patients with non-sedated patients. Klein et. al. (2018) Cross-Sectional Palliative Sedierung Develop standardized documentation for the preparation, administration, documentation, and evaluation of palliative sedation in Germany. The text describes the need to establish a unified foundation for the practice of palliative sedation due to the variety of methods and practices in the country.
Discussion
The selected articles address a variety of issues related to the management of palliative sedation in patients under palliative care, focusing on different aspects and contexts.
The first article aims to assess the frequency, clinical indications, and outcomes of Psychosis Syndrome in patients with advanced cancer, providing a detailed insight into the clinical complexities involved in this context (6). The second article discusses the implementation of the Clayes Leonetti Law in France, highlighting the evolution of palliative sedation practice within the legal framework, which is an important aspect to consider when providing palliative care(9). The third article addresses the complex nature of palliative sedation in the treatment of existential suffering, emphasizing the ethical and clinical complexity of this practice, which is a critical point in any discussion about palliative care(10).
As the two last studies provide valuable insights in terms of research and practice. The fourth article focuses on end-of-life sedation practice in palliative care units in Austria, providing information on the characteristics of sedated patients, the indications for sedation, and the medications used. This is essential to understand how palliative sedation is applied in different contexts and can help inform best practices (11). Finally, the sixth article addresses the need to develop standardized documentation for palliative sedation practice in Germany, recognizing the importance of uniformity and quality in palliative care (12). This is crucial to ensure that patients receive the highest level of care, regardless of their location in the country. (12,13).
Overall, these articles contribute to a broader understanding of palliative sedation and its complexities in various palliative care settings, promoting discussion and continuous improvement of this practice in ICUs (6,9–13).
This study has inherent limitations due to its nature of integrative review, as the literature search process has challenges stemming from the method itself, limiting the methodological scope. However, we have described significantly the main practices for managing palliative sedation in patients under palliative care in intensive therapy. We have also suggested best practices and emphasized the importance of their utilization.
Conclusion
Through this integrative literature review, we were able to achieve the main objective of the study, which was to identify and discuss the main practices and approaches of the multidisciplinary team in the management of palliative sedation through the selected articles that allowed us to understand how it is applied in different contexts, addressing clinical, ethical, and legal issues.
However, there is a noticeable scarcity of studies on this specific issue, suggesting the need for additional research to deepen our understanding of this important topic for healthcare professionals. The complexity of palliative sedation, along with variations in practices between countries and institutions, underscores the importance of future investigations that explore the obstacles and best practices in this field.
In this way, this study provides a solid foundation for understanding palliative sedation in the ICU, but it also highlights the importance of continuing research and promoting discussion on the best way to provide comprehensive and empathetic palliative care to patients in their final moments of life. The quality of this care is essential to ensure that patients and their families face this period with dignity and comfort.
REFERENCES
1. Seaman JB, Arnold RM, Buddadhumaruk P, Shields AM, Gustafson RM, Felman K, et al. Protocol and fidelity monitoring plan for four supports a multicenter trial of an intervention to support surrogate decision makers in intensive care units. Ann Am Thorac Soc. 2018;15(9):1083–91.
2. Martins BDCPCC, Oliveira RA, Cataneo AJM. Palliative care for terminally ill patients in the intensive care unit: Systematic review and metaanalysis. Palliat Support Care. 2017;15(3):376–83.
3. Michalsen A, Long AC, DeKeyser Ganz F, White DB, Jensen HI, Metaxa V, et al. Interprofessional shared decision-making in the ICU: A systematic review and recommendations from an expert panel. Crit Care Med. 2019;47(9):1258–66.
4. Azoulay E, Forel J marie, Vinatier I, Truillet R, Valade S, Jaber S, et al. Questions to improve family – staff communication in the ICU : a randomized controlled trial To cite this version : HAL Id : hal-01910514. 2019;
5. Kim JM, Godfrey S, O’neill D, Sinha SS, Kochar A, Kapur NK, et al. Integrating palliative care into the modern cardiac intensive care unit: A review. Eur Heart J Acute Cardiovasc Care. 2022;11(5):442–9.
6. Prado BL, Gomes DBD, Usón Júnior PLS, Taranto P, França MS, Eiger D, et al. Continuous palliative sedation for patients with advanced cancer at a tertiary care cancer center. BMC Palliat Care. 2018;17(1):1–7.
7. Briggs J. Checklist for Systematic Reviews and Research Syntheses. The Joanna Briggs Institute [Internet]. 2017;7. Disponível em: http://joannabriggs.org/research/critical-appraisal-tools.htmlwww.joannabriggs.org%0Awww.joannabriggs.org
8. Singer AE, Ash T, Ochotorena C, Lorenz KA, Chong K, Shreve ST, et al. A Systematic Review of Family Meeting Tools in Palliative and Intensive Care Settings. American Journal of Hospice and Palliative Medicine. 2016;33(8):797–806.
9. Le Dorze M, Kandelman S, Veber B, Brunel E, Baghdadi H, Baumann A, et al. Deep continuous sedation maintained until death, in French Intensive Care Units. Anaesth Crit Care Pain Med. 2020;39(1):115–6.
10. Bruce A, Boston P. Relieving existential suffering through palliative sedation: Discussion of an uneasy practice. J Adv Nurs. 2011;67(12):2732–40.
11. Effendy C, Yodang Y, Amalia S, Rochmawati E. Barriers and facilitators in the provision of palliative care in adult intensive care units: a scoping review. Acute and Critical Care. 2022;37(4):516–26.
12. Klein C, Wittmann C, Wendt KN, Ostgathe C, Stiel S. Palliative sedation: Development and consensus of a German language documentation template. Anaesthesist. 2018;67(7):504–11.
13. Schur S, Weixler D, Gabl C, Kreye G, Likar R, Masel EK, et al. Sedation at the end of life – A nation-wide study in palliative care units in Austria. BMC Palliat Care [Internet]. 2016;15(1):1–8. Disponível em: http://dx.doi.org/10.1186/s12904-016-0121-8
¹Graduando em Fisioterapia pelo Centro Universitário Integrado (CEI), r.barretoo@outlook.com
²Graduada em Enfermagem pelo Centro Universitário Brasileiro (UNIBRA) E-mail: brunatltavares@gmail.com
³Graduanda em Fisioterapia pelo Centro Universitário Integrado (CEI), lorenamayaradoamaral@gmail.com
4Graduanda em Fisioterapia pela Universidade da Amazônia (UNAMA) saramoraes022@gmail.com
5Graduada em Fisioterapia pela Universidade Federal de Mato Grosso do Sul (UFMS) e Pós-graduanda em Terapia Intensiva Neonatal e Pediátrica pela Pontifícia Universidade Católica do Paraná (PUCPR/ARTMED) sr.aguirres@gmail.com
6Graduando em Fisioterapia pela Universidade do Estado de Minas Gerais (UEMG), matheushtv@gmail.com
7Graduada em Fisioterapia pela Universidade de Cuiabá (UNIC) e Pós-graduada em Terapia Intensiva Adulto, Neonatal e Pediátrica pela Faculdade Inspirar (INSPIRAR) lurodrigues26@hotmail.com
8Graduada em Fisioterapia pelo Centro Universitário Alfredo Nasser (UNIFAN) e Pós-graduanda em Fisioterapia Dermatofuncional pelo Instituto Educacional CDCS, mariacjmontalvao@gmail.com
9Fisioterapeuta pela Faculdade Barão do Rio Branco (UNINORTE), Pós-graduado em Ortopedia pela Faculdade Inspirar (INSPIRAR), Fisioterapeuta da Secretaria de Estado de Saúde do Acre (SESACRE), cesarperees@gmail.com
10Graduada em Enfermagem pelo Centro Universitário UNIFACISA e Mestranda em Saúde da Criança e do Adolescente pela Universidade Federal de Pernambuco (UFPE) raissamayaradantas@hotmail.com
¹¹Graduado em Fisioterapia pela da Universidade Federal de Juiz de Fora (UFJF), Pós-graduado em Fisioterapia em Terapia Intensiva Adulto (UNICOR) e Mestrando em Ciências da Reabilitação e Desempenho Físico Funcional (UFJF) fisio.lucassena@gmail.com
¹²Graduado em Fisioterapia pelo Centro Universitário de Maringá (UNICESUMAR), Pós graduado em Docência no Ensino Superior (UNICV) e Mestrando do programa de Pós Graduação Interdisciplinar Sociedade e Desenvolvimento (UNESPAR), anderson.brandao@grupointegrado.br
¹³Graduado em Fisioterapia pela Faculdade São Paulo (FSP), Pós-graduado em Docência do Ensino Superior (UNINTER), Residência Multiprofissional em Fisioterapia em Unidade de Terapia Intensiva (HRC), Mestre em Fisioterapia com ênfase em Cardiorrespiratória (UDESC), Doutorando em Ciências do Movimento Humano (UDESC) allefdiego_bonfim@hotmail.com
