ESTRATÉGIAS DE ENFERMAGEM PARA PREVENÇÃO DE INFECÇÃO RELACIONADO AO CATETER VENOSO CENTRAL
REGISTRO DOI: 10.69849/revistaft/pa10202505311258
Gonzaga, Christian Liria de Oliveira1
Coimbra, Juliano Rodrigues1
Silva, Douglas Fernandes1
RESUMO
As infecções relacionadas ao cateter venoso central (CVC) representam uma das principais causas de morbidade e mortalidade em ambientes hospitalares, especialmente em unidades de terapia intensiva. Este estudo teve como objetivo revisar a literatura científica sobre as estratégias de enfermagem voltadas à prevenção dessas infecções, destacando práticas baseadas em evidências que contribuem para a segurança do paciente. A pesquisa foi realizada nas bases de dados PubMed, SciELO e Google Acadêmico, entre janeiro e março de 2025, utilizando descritores relacionados à prevenção de infecções associadas ao CVC e à atuação da enfermagem. Os resultados apontam que a adoção de bundles de prevenção, a higienização rigorosa das mãos, o uso de barreiras estéreis, a escolha adequada do sítio de inserção e a capacitação contínua da equipe são medidas fundamentais para reduzir a incidência de infecções da corrente sanguínea. Conclui- se que a atuação da equipe de enfermagem, especialmente por meio de práticas baseadas em protocolos e da educação permanente, é determinante para a eficácia das estratégias de prevenção e para a qualidade da assistência prestada.
Palavras chaves: Cateter Venoso Central, Infecção da corrente sanguínea, Enfermagem, Prevenção, Controle de infecção hospitalar.
ABSTRACT
Central venous catheter (CVC)-related infections represent one of the main causes of morbidity and mortality in hospital settings, especially in intensive care units. This study aimed to review the scientific literature on nursing strategies aimed at preventing these infections, highlighting evidence-based practices that contribute to patient safety. The research was conducted in the PubMed, SciELO, and Google Scholar databases between January and March 2025, using descriptors related to the prevention of CVC- associated infections and nursing performance. The results indicate that the adoption of prevention bundles, rigorous hand hygiene, the use of sterile barriers, the appropriate choice of insertion site, and ongoing staff training are fundamental measures to reduce the incidence of bloodstream infections. It is concluded that the performance of the nursing team, especially through protocol-based practices and continuing education, is crucial for the effectiveness of prevention strategies and the quality of care provided.
Keywords: Central Venous Catheter. Bloodstream infection. Nursing. Prevention. Hospital infection control.
1 INTRODUCTION
Central venous catheters (CVCs) are widely used in clinical practice for hemodynamic monitoring, medication administration, and parenteral nutritional support in critically ill patients (HILL; SMITH, 2021). CVCs, along with other intravascular catheters, are among the most widely used invasive devices globally, and are essential in the management of patients hospitalized in Intensive Care Units (ICUs) (MARQUES; FERREIRA; CARNEIRO, 2011).
The use of central venous catheters (CVCs) is strongly associated with an elevated risk of bloodstream infections, which contribute to prolonged hospital stays, increased healthcare costs, and heightened morbidity and mortality rates. As early as 2011, Marques, Ferreira, and Carneiro had already emphasized that the extended use of CVCs constitutes a significant risk factor for infectious complications (MARQUES; FERREIRA; CARNEIRO, 2011). Within this context, infections related to CVCs remain a major concern in intensive care practice, demanding sustained vigilance and adherence to safety protocols by healthcare teams (BÖLL et al., 2021). Consequently, the implementation of evidence-based prevention strategies is imperative to enhance patient safety and mitigate the adverse outcomes associated with these infections ((PITIRIGA et al., 2020).
Bloodstream infections (BSIs) represent a serious public health problem, accounting for a considerable increase in morbidity and mortality rates in hospital settings. In addition, these infections are associated with prolonged hospital stays and increased hospital costs. The use of central venous catheters (CVCs) is one of the main risk factors for the occurrence of these infections, with an estimated 250,000 cases of central line-associated bloodstream infections (CLABSIs) occurring annually in the United States (PITIRIGA et al., 2020).
The implementation of care bundles—structured sets of evidence-based clinical practices—has proven highly effective in reducing central venous catheter (CVC)- related infections (PITIRIGA et al., 2020). These bundles typically comprise key elements such as strict hand hygiene, the use of full barrier precautions during catheter insertion, antisepsis of the insertion site with 2% chlorhexidine, and daily assessment of the necessity for continued catheterization. According to Negm et al. (NEGM et al., 2021), the consistent application of these practices, along with continuous professional
education and multidisciplinary team involvement, significantly contributes to lowering infection rates and improving patient safety outcomes.
Additional factors with synergistic potential also play a critical role in preventing central line-associated bloodstream infections (CLABSIs). The use of chlorhexidine- impregnated dressings at the catheter insertion site has been shown to significantly reduce infection rates (BENLIGÜL; BEKTAŞ, 2023). Similarly, rigorous hand hygiene practices—performed both before and after catheter manipulation—remain a cornerstone in minimizing the risk of contamination (JARDING; FLYNN MAKIC, 2021). Moreover, the continuous education and training of nursing professionals, particularly in aseptic techniques and best practices for CVC handling, are fundamental for safeguarding patient outcomes and mitigating infectious complications.
Active surveillance and continuous evaluation of clinical practices related to central venous catheter (CVC) insertion and maintenance constitute essential components of infection prevention strategies. The implementation of structured audits, when combined with targeted feedback to healthcare providers, has demonstrated efficacy in enhancing adherence to evidence-based protocols and improving the overall quality of care. Furthermore, the ongoing monitoring of CLABSI (central line-associated bloodstream infection) rates provides critical metrics for assessing the impact of implemented interventions. This approach enables informed decision-making based on empirical data and supports the design of more effective and responsive preventive measures (BUETTI et al., 2022).
The use of central venous catheters is common in hospitalized patients who require prolonged intravenous therapies, such as medication administration, parenteral nutrition, or hemodynamic monitoring. However, their use is associated with a high risk of bloodstream infections, which can prolong hospitalization, increase treatment costs, and lead to adverse outcomes, including death. Therefore, it is essential to study nursing strategies aimed at preventing these infections, since nurses play a central role in the management, insertion, maintenance, and monitoring of CVCs. The aim of this study is to contribute to patient safety and improve care practices in the hospital environment.
2 METHODOLOGY
This study consisted of a literature review, in which studies were carefully selected after a comprehensive search in several electronic databases, including PubMed (National Library of Medicine), SciELO (Scientific Electronic Library Online) and Google Scholar. The research was conducted between January and March 2025, with the central theme: “Nursing strategies for the prevention of infections related to the central venous catheter (CVC)”. To select the articles, keywords such as: “Infections in central catheters” and “Nursing in the prevention of infections in the central venous catheter” were used, with the aim of providing a broad and in-depth view of the topic in question. In this work, only articles published in Portuguese and English that presented thematic adherence were included in the analysis. Studies that were not relevant to the research objectives were excluded.
3. PREVENTION OF INFECTIONS RELATED TO THE CENTRAL VENOUS CATHETER
The handling of central venous catheters (CVCs) including their insertion, maintenance and removal is an activity that requires technical and scientific knowledge and ongoing training on the part of nursing professionals. Although the Federal Nursing Council (Conselho Federal de Enfermagem – COFEN) does not have a specific regulation that defines this responsibility as exclusive to nurses, several opinions and resolutions establish guidelines on the subject. COFEN Resolution No. 258/2001 authorizes nurses to insert central peripheral catheters, provided they have undergone professional qualification and/or training. In addition, COFEN Normative Opinion No. 001/2015 highlights the participation of nurses in hemodynamic procedures, specifically in the removal of vascular introducers (COFEN, 2001, 2015). In this context, the insertion of central venous catheters (CVCs) in neonates demands specialized technical expertise and adherence to evidence-based protocols due to the complexity and inherent risks of the procedure. Ribeiro et al. (RIBEIRO et al., 2018) conducted a scoping review protocol aimed at mapping the best care practices for CVC insertion in newborns, emphasizing the necessity of systematizing knowledge to guide safe and effective clinical management within neonatal intensive care settings.
Despite the numerous benefits provided using CVCs, healthcare-associated infections (HAIs) associated with this device represent the main cause of infections in intensive care units (ICUs). These infectious events are associated with prolonged hospital stays (ranging from 3 to 20 days), a significant increase in hospital costs, estimated at approximately US$30,000 per patient, and an increase of up to 69% in the mortality rate (RIBEIRO et al., 2018).
As a primary measure to prevent infections related to central venous catheters (CVCs), it is essential that healthcare professionals, patients and their families perform adequate hand hygiene. This practice should be carried out using antiseptics, preferably 70% ethyl alcohol, with friction for at least 15 seconds. In situations where there is visible dirt or the presence of organic matter, hand hygiene with antiseptic soap is recommended (ALMEIDA et al., 2018). According to the authors, although needleless catheter connectors have contributed to reducing accidents with sharps, their introduction in some institutions has been associated with an increase in the incidence of catheter-related bloodstream infections (CRBSI). This increase can be attributed to the lack of adequate disinfection of the valved connectors, recontamination after handling, and irregularity in the septal surface of the valves. Regarding infusion systems, continuous-use equipment should be replaced every 96 hours at most. Those used less frequently should be changed at intervals of 24 to 72 hours, depending on the application. For intermittent infusions, administration of lipid emulsions (as in parenteral nutrition) or blood products, replacement every 24 hours is recommended.
The implementation of bundles a structured set of evidence-based interventions has proven effective in standardizing the aseptic techniques used during CVC insertion and maintenance, aiming at preventing infections. Among the recommended practices, the use of maximum sterile barriers (sterile gloves, apron, mask, cap and sterile fields) by the entire team involved in the procedure stands out, as well as rigorous antisepsis of the skin with 0.5% chlorhexidine alcohol solution at the time of insertion. During device maintenance, measures such as hand hygiene before any handling and disinfection of hubs and connections with 70% alcohol must be strictly observed (LUCAS et al., 2018).
Table 1 presents the recommendations established by the Centers for Disease Control and Prevention (CDC) regarding the care of dressings at the insertion site of the central venous catheter (CVC). These guidelines aim to prevent infections associated with the use of the device, and are classified by categories of evidence, according to the degree of scientific recommendation. The guidelines include the choice of dressing type (sterile gauze or transparent and semipermeable dressing), the ideal frequency for changing the dressings, and the specific conditions that require early changes, such as moisture, dirt, or loosening (O’GRADY et al., 2002). In addition, the CDC discourages the routine use of antibiotic ointments at insertion sites — except in specific cases — due to the risk of microbial resistance and fungal infections. There are also specific guidelines for bathing, considering the need for impermeable protection, as well as distinctions between short-term and long-term catheters regarding the frequency of dressing changes. Some recommendations remain uncategorized or are classified as “unsolved problems,” especially in the context of well-healed exit sites in long-term cuffed catheters. These recommendations are essential to guide safe and evidence-based clinical practice in the management of patients with central venous catheters (CVCs) and are essential for reducing infectious complications.
Table 1: CDC recommendations for catheter site dressing regimens (Centers for Disease Control and Prevention 2017)
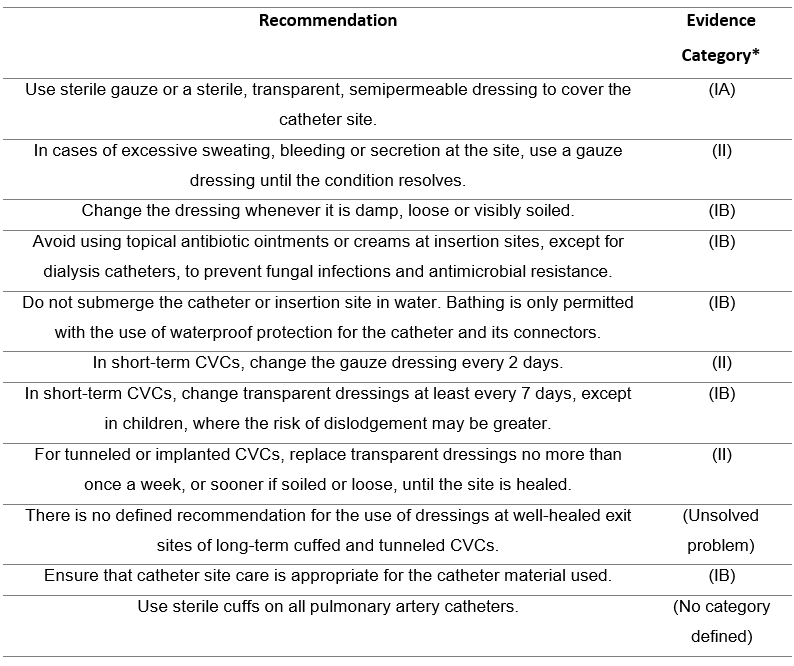
Table 2 presents the recommendations of the World Health Organization (WHO) regarding the care of dressings on central venous catheters (CVCs), with the aim of preventing healthcare-associated infections. These guidelines emphasize evidence- based practices and must be strictly followed by all professionals involved in handling the device. Hand hygiene is highlighted as an essential measure before and after any handling of the dressing or catheter and should be performed with 70% alcohol or soap and water, depending on the situation (WORLD HEALTH ORGANIZATION, 2024). The WHO recommends the use of sterile and transparent dressings, which allow continuous visualization of the insertion site, reducing the need for frequent removals. In situations involving bleeding, secretion or intense sweating, replacement with sterile gauze dressing with more frequent changes is indicated. Skin antisepsis should be performed with a 2% chlorhexidine solution in 70% alcohol and is essential in all dressing changes and catheter manipulations.
Other guidelines include changing the dressing whenever it is damp, dirty, loose or damaged, and regardless of visible changes, it should be changed at least once a week, especially when using transparent dressings. The entire procedure should be performed using complete aseptic technique, using sterile gloves, sterile drapes and appropriate materials. The WHO also emphasizes the importance of ongoing training of health professionals, standardization of care through institutional protocols and active surveillance of the insertion site, with systematic recording of clinical signs suggestive of infection. Therefore, these recommendations are essential to ensure patient safety, reduce complications and promote the quality of care provided in health units.
Table 2: WHO Recommendations for Dressing Care of Central Venous Catheters.

4. CRITERIA FOR CHOOSING THE INSERTION SITE AND THE IMPORTANCE OF PROFESSIONAL TRAINING IN PREVENTING CVC-RELATED INFECTIONS
Although the literature presents some controversy regarding the optimal insertion site for central venous catheters (CVCs) between the internal jugular and subclavian veins, the subclavian vein is generally favored. This preference is attributed to the higher infection risk associated with internal jugular vein catheterization, which is related to its proximity to oropharyngeal secretions and challenges in securing and maintaining the dressing. Conversely, the femoral vein is the least recommended site due to its increased susceptibility to microbial colonization and, consequently, a heightened risk of infection (FERREIRA; ANDRADE; FERREIRA, 2011).
Insertion of the catheter into the femoral vein is generally avoided, since the high microbial density of the inguinal region represents an important risk factor for infections, especially in patients with urinary or fecal incontinence, given the difficulty in adequately cleaning the site. In addition, its use is associated with a higher risk of complications, such as deep vein thrombosis, due to prolonged immobilization of the lower limbs (DA SILVA; OLIVEIRA, 2016).
The use of CVCs is directly related to the risk of complications, particularly infections at the insertion site and bloodstream infections. Studies show that many of these complications can be prevented through ongoing training of nursing staff, with an emphasis on the rigorous application of technical protocols based on scientific evidence (PERIN et al., 2016). The most effective preventive methods include proper hand hygiene with antiseptics such as chlorhexidine disinfectant, the use of sterile techniques during insertion, and aseptic handling of the catheter in the post-insertion period.
Central venous catheter-associated bloodstream infections (CLABSIs) are a significant concern in hospital settings, contributing to increased morbidity, mortality, and hospitalization costs. Several recent studies highlight the effectiveness of educational programs in reducing these infections, highlighting the importance of ongoing training of healthcare teams (HIGHTOWER et al., 2022). A study conducted in Saudi Arabia demonstrated that after implementing a comprehensive national initiative, CLABSI rates in adult intensive care units were reduced by 48.8%. The initiative included hybrid training for healthcare professionals, development of evidence-based guidelines, and ongoing monitoring of infection rates (WORLD HEALTH ORGANIZATION (WHO), 2023).
Educational programs aimed at multidisciplinary teams have shown significant results in reducing CVC-related infections. A study conducted showed that, after the implementation of educational measures, the infection rate, initially recorded at 22.72 cases per thousand days of catheter use, was reduced to 5.87 cases per thousand days over a two-year period. The authors emphasize that simple, low-cost and easy- to-implement interventions can be highly effective, as long as they are associated with the engagement of the multidisciplinary team, the support of hospital management and the proactive action of the Hospital Infection Control Committee, which should promote surveillance actions and foster an institutional culture of patient safety (MEDEIROS, 2010)
The use of central venous catheters (CVCs) is an essential resource in several intravascular therapies, especially in intensive care units and in the management of critically ill patients. However, its use is associated with significant risks, mainly related to bloodstream infections (BSIs), which can result in increased morbidity and mortality, length of hospital stays and hospital costs. Scientific evidence shows that most of these infections can be avoided through the rigorous adoption of practices based on updated technical protocols, with an emphasis on ongoing training of the multidisciplinary team involved in the handling and maintenance of CVCs (FOKA et al., 2023; SHIMOYAMA et al., 2017). Among the most effective preventive measures are hand hygiene with appropriate antiseptics, such as chlorhexidine, the use of aseptic technique during insertion and adequate care with dressings, as recommended by institutions such as the World Health Organization (WORLD HEALTH ORGANIZATION (WHO), 2023).
Additionally, educational programs aimed at healthcare teams have demonstrated a significant reduction in infection rates associated with the use of CVCs, demonstrating that simple, low-cost and easy-to-implement measures can be highly effective when associated with institutional engagement and a culture of patient safety (FOKA et al., 2023). This reinforces the need for ongoing institutional commitment, including investment in continuing education, standardization of evidence-based protocols, and active monitoring of clinical practices. Such actions are essential for preventing CVC-related infections and, consequently, for promoting safer and higher- quality patient care.
5. CONCLUSION
Prevention of infections related to central venous catheters (CVCs) remains one of the main challenges faced in intensive care units and other hospital settings, requiring a coordinated effort by the entire multidisciplinary team, with emphasis on the central role of nursing. This study demonstrated that the rigorous adoption of strategies based on updated clinical protocols, combined with ongoing training of professionals and the systematic application of aseptic measures, constitutes an essential set of practices aimed at reducing infectious complications associated with the use of CVCs. It is worth noting that investment in continuing education, periodic audits of catheter insertion and maintenance processes, as well as active monitoring of care practices, are fundamental components to ensure the quality of care provided and patient safety. In this context, nursing stands out as a protagonist in conducting preventive interventions, reaffirming its strategic role in promoting safe, ethical, and evidence- based care.
6. ACKNOWLEDGEMENTS
The authors wish to University Center of the Integrated Faculties of Ourinhos – Unifio, Ourinhos, SP, Brazil.
7. REFERENCES
ALMEIDA, Thamyres Morgado De; GALLASCH, Cristiane Helena; GOMES, Helena Ferraz; FONSECA, Bianca De Oliveira; PIRES, Ariane Da Silva; PERES, Ellen M. Prevenção de infecções relacionadas ao cateter venoso central não implantado de curta permanência. Revista Enfermagem UERJ, [S. l.], v. 26, p. e31771, 2018. DOI: 10.12957/reuerj.2018.31771.
BENLIGÜL, Ebru Melek; BEKTAŞ, Murat. Effectiveness of Chlorhexidine- Impregnated Central Venous Catheter Dressing for Preventing Catheter-Related Bloodstream Infections in Pediatric Patients: A Systematic Review and Meta-Analysis Study. Journal of Pediatric Infectious Diseases, [S. l.], v. 18, n. 03, p. 116–126, 2023. DOI: 10.1055/s-0043-1764479.
BÖLL, Boris et al. Central venous catheter–related infections in hematology and oncology: 2020 updated guidelines on diagnosis, management, and prevention by the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Annals of Hematology, [S. l.], v. 100, n. 1, p. 239–259, 2021. DOI: 10.1007/s00277-020-04286-x.
BUETTI, Niccolò et al. Strategies to prevent central line-associated bloodstream infections in acute-care hospitals: 2022 Update. Infection Control & Hospital Epidemiology, [S. l.], v. 43, n. 5, p. 553–569, 2022. DOI: 10.1017/ice.2022.87.
COFEN. RESOLUÇÃO COFEN-258/01- Inserção de Cateter Periférico Central, pelos Enfermeiros. 2001. Disponível em: https://www.coren-ro.org.br/resolucao- cofen-25801-insercao-de-cateter-periferico-central-pelos-enfermeiros/.
COFEN. PARECER NORMATIVO No 001/2015/COFEN. 2015. Disponível em: https://www.cofen.gov.br/parecer-normativo-no-0012015/.
DA SILVA, Alanna Gomes; OLIVEIRA, Adriana Cristina De. Prevenção da infecção da corrente sanguínea relacionada ao cateter venoso central: Uma revisão integrativa. Vigilância Sanitária em Debate, [S. l.], v. 4, n. 2, 2016. DOI: 10.3395/2317-269x.00705.
FERREIRA, Maria Verônica Ferrareze; ANDRADE, Denise De; FERREIRA, Adriano Menis. Controle de infecção relacionada a cateter venoso central impregnado com antissépticos: revisão integrativa. Revista da Escola de Enfermagem da USP, [S. l.], v. 45, n. 4, p. 1002–1006, 2011. DOI: 10.1590/S0080-62342011000400030.
FOKA, Maria; KYPRIANOU, Theodoros; STYLIANIDES, Nikolas; PAIKOUSIS, Lefkios; PALAZIS, Lakis; KYRANOU, Maria; PAPATHANASSOGLOU, Elizabeth; LAMBRINOU, Ekaterini. An Interactive E-learning Platform-Based Training to Improve Intensive Care Professionals’ Knowledge Regarding Central Venous Catheter-Related Infections. Cureus, [S. l.], v. 15, n. 10, p. e46399, 2023. DOI: 10.7759/cureus.46399.
HIGHTOWER, Hannah B. et al. Reduction of Central-line–Associated Bloodstream Infections in a Tertiary Neonatal Intensive Care Unit through Simulation Education. Pediatric Quality & Safety, [S. l.], v. 7, n. 6, p. e610, 2022. DOI: 10.1097/pq9.0000000000000610.
HILL, Barry; SMITH, Catherine. Central venous pressure monitoring in critical care settings. British Journal of Nursing, [S. l.], v. 30, n. 4, p. 230–236, 2021. DOI: 10.12968/bjon.2021.30.4.230.
JARDING, Emily K.; FLYNN MAKIC, Mary Beth. Central Line Care and Management: Adopting Evidence-Based Nursing Interventions. Journal of PeriAnesthesia Nursing, [S. l.], v. 36, n. 4, p. 328–333, 2021. DOI: 10.1016/j.jopan.2020.10.010.
LUCAS, Thabata Coaglio; CAMPOS DE SÁ, Poliana Lopes; DOS SANTOS, Laura Petronilha; LEITE, Cleyde Amaral; CALDEIRA, Ana Luisa De Paulo; OLIVEIRA, Adriana Cristina De. Desafio da higienização das mãos para a implementação dos bundles de cateter venoso central. Revista de Epidemiologia e Controle de Infecção, [S. l.], v. 8, n. 3, p. 216–223, 2018. DOI: 10.17058/reci.v8i3.11283.
MARQUES, Patrícia Bentes; FERREIRA, Alcione Pena; CARNEIRO, Flavia Matilla Colares. Perfil bacteriano de cultura de ponta de cateter venoso central. Revista Pan-Amazônica de Saúde, [S. l.], v. 2, n. 1, p. 53–58, 2011. DOI: 10.5123/S2176- 62232011000100006.
MEDEIROS, Eduardo Alexandrino S. Efeito de um programa educacional na redução de infecção da corrente sanguínea relacionada ao cateter venoso central. Revista Paulista de Pediatria, [S. l.], v. 28, n. 4, p. 290–291, 2010. DOI: 10.1590/S0103-05822010000400001.
NEGM, Essamedin M.; OTHMAN, Howaydah A.; TAWFEEK, Mohamed M.; ZALAT, Marwa M.; EL-SOKKARY, Rehab H.; ALANWER, Khaled M. Impact of a comprehensive care bundle educational program on device-associated infections in an emergency intensive care unit. Germs, [S. l.], v. 11, n. 3, p. 381–390, 2021. DOI: 10.18683/germs.2021.1275.
O’GRADY, Naomi P. et al. Guidelines for the prevention of intravascular catheter- related infections. Clinical Infectious Diseases, [S. l.], v. 35, n. 11, p. 1281–1307, 2002. DOI: 10.1086/344188.
PERIN, Daniele Cristina; ERDMANN, Alacoque Lorenzini; HIGASHI, Giovana Dorneles Callegaro; SASSO, Grace Teresinha Marcon Dal. Evidence-based measures to prevent central line-associated bloodstream infections: a systematic review. Revista Latino-Americana de Enfermagem, [S. l.], v. 24, 2016. DOI: 10.1590/1518-8345.1233.2787.
PITIRIGA, Vassiliki; KANELLOPOULOS, Petros; BAKALIS, Ioannis; KAMPOS, Elsa; SAGRIS, Ioannis; SAROGLOU, George; TSAKRIS, Athanasios. Central venous catheter-related bloodstream infection and colonization: the impact of insertion site and distribution of multidrug-resistant pathogens. Antimicrobial Resistance & Infection Control, [S. l.], v. 9, n. 1, p. 189, 2020. DOI: 10.1186/s13756-020-00851-1.
RIBEIRO, Wanderson Alves; ANDRADE, Marilda; FASSARELLA, Bruna Porath Azevedo; SOUZA, Viviane De Melo; PEREIRA, Eric Rosa; CIRINO, Hosana Pereira; DE AZEVEDO, Taiana Daniela Pereira; DE SOUZA, João Luiz Ramos. Cateter venoso central na UTI pediátrica : o enfermeiro intensivista na prevenção e controle das infecções hospitalares. Revista Pró-UniverSUS, [S. l.], v. 9, n. 2, p. 47–52, 2018.
SHIMOYAMA, Yuichiro; UMEGAKI, Osamu; AGUI, Tomoyuki; KADONO, Noriko; KOMASAWA, Nobuyasu; MINAMI, Toshiaki. An educational program for decreasing catheter-related bloodstream infections in intensive care units: a pre- and post- intervention observational study. JA Clinical Reports, [S. l.], v. 3, n. 1, p. 23, 2017. DOI: 10.1186/s40981-017-0095-4.
WORLD HEALTH ORGANIZATION (ORG.). Guidelines for the prevention of bloodstream infections and other infections associated with the use of intravascular catheters: part I: peripheral catheters. [s.l: s.n.].
WORLD HEALTH ORGANIZATION (WHO). Infection, prevention and control excellence in the Kingdom of Saudi Arabia: reducing central line-associated bloodstream infections. 2023. Disponível em: https://www.who.int/news- room/feature-stories/detail/infection–prevention-and-control-excellence-in-the- kingdom-of-saudi-arabia–reducing-central-line-associated-bloodstream-infections.
1 Department of Nursing – University Center of the Integrated Faculties of Ourinhos – Unifio, Ourinhos, SP, Brazil. (ORCID: 0009-0008-2595-5838) christianldogonzaga27@gmail.com
1 Department of Nursing – University Center of the Integrated Faculties of Ourinhos – Unifio, Ourinhos, SP, Brazil. (ORCID: 0000-0002-3227-452X) liano.coimbra@unifio.edu.br
1 Department of Nursing – University Center of the Integrated Faculties of Ourinhos – Unifio, Ourinhos, SP, Brazil. (ORCID: 0000-0002-0252-1112) douglas.silva@unifio.edu.br
