REGISTRO DOI: 10.69849/revistaft/os102411271425
Paulo Sérgio Santos1
Angela Mara Rambo Martini1
Adriane Viapiana Bossa2
Caroline Azevedo3
ABSTRACT
Pain is considered a very common symptom in several illnesses. Allopathic medicine has several drugs to combat it. However, their side effects can greatly harm health. Thus, this study is an exploratory, descriptive research with a quantitative approach analyzing the medical record of an individual treated with Medicinal Biomagnetism therapy (MB). This technique created by Mexican physician Isaac Goiz Durán in 1988 consists of placing medium-intensity magnets (1,000 to 7,500 Gauss) on specific points of the body. Therefore, the static magnetic field generated may contribute to the energetic and bioelectric balance of the organism facilitating homeostasis and better performance of the immune system. The aim of this study was to verify the effects of a pain relief treatment, the Modern Trauma Pair (MTP). Its application is simple, noninvasive, low-cost, with mild, transient, and non-harmful side effects, such as drowsiness and increased diuresis. This case study was conducted using information from the medical record of a participant who presented with abrasions on the tips of her fingers. The pain was classified as severe, acute, superficial, somatic, and nociceptive considering the Visual Analog Scale (VAS) for pain intensity measurement. Fifteen minutes after starting the application, pain intensity of level 8 was completely reduced and pain intensity of 10 was reduced to 2, indicating that MTP has a positive and fast action being a good treatment option.
Keywords: Medicinal Biomagnetism; Biomagnetic Pair; Modern Trauma Pair; Pain relief; Magnetotherapy; Magnets; Static Magnetic Field.
INTRODUCTION
It is common for pain to arise at some point in the development of several illnesses (VARANDAS, 2013). However, this sensation could be a signal that something is not right and that some action is needed (BARROS; PAULINO, 1999). But besides appearing as a symptom, it may also be the disease itself. Pain is increasingly prevalent in society, especially chronic pain. The increase in longevity and chronic diseases may be some of the reasons (TEIXEIRA; YENG; KAZIYAMA, 2008; VARANDAS, 2013; BARROS; PAULINO, 1999).
After a recent review in 2021, the International Association for the Study of Pain (IASP) defines pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” (RAJA, 2021). It is noteworthy from this definition that pain is a mental process, a sensation, an emotion, a perception. Therefore, it is not mandatory to have a physical injury for pain occurrence, as long as the brain perceives a situation as harmful (ARGOFF; DUBIN; PILITSIS, 2019). In other words, as noted in the IASP review, “pain and nociception are different phenomena. Pain cannot be determined solely by the activities of sensory neurons” (RAJA, 2021).
The manual on pain control developed by the National Cancer Institute approaches pain as a unique and personal experience, with emotional and social components (BRASIL, 2001). According to Teixeira, Yeng and Kaziyama (2008), Argoff, Dubin and Pilitsis (2019), and Parker (2012), sensory neurons are spread throughout the body and are capable of sensing stimuli (chemical, physical, or thermal) being able to perceive the difference between them. When a neurological receptor or nociceptor receives a stimulus as harmful to the tissues, it transmits an action potential propagating through the Peripheral Nervous System (PNS) to the Central Nervous System (CNS), that is, it goes through the spinal cord ascending to the brain.
Considering the physio-pathological origin, pain may be classified as nociceptive according to the process explained above (divided into visceral and somatic), and non-nociceptive (divided into neuropathic and psychogenic). Nociceptive pain originates from a stimulus perceived by a nociceptor corresponding to damage to a tissue or organ. It may be visceral (when the injury is in internal organs), superficial somatic (skin injury), or deep somatic (injury to other structures: muscles, bones, tendons, and ligaments) (TEIXEIRA; YENG; KAZIYAMA, 2008; ARGOFF; DUBIN; PILITSIS, 2019; PARKER, 2012).
The skin consists of an epithelial portion (epidermis) and a connective portion. The dermis is supported on the subcutaneous layer (hypodermis) which has adipocytes that is not part of the skin. The epidermis is formed by keratinized stratified squamous epithelium. The dermis is formed by two layers: the thin loose connective tissue layer (papillary layer) which is just below the epidermis and the deeper dense connective tissue layer (reticular layer) (BARROS; PAULINO, 1999; PARKER, 2012).
The pain is classified as nociceptive in case of a skin abrasion as it arises from tissue damage that would generate a stimulus perceived by a nociceptor. If the injury does not refer to internal organs, the pain would be considered somatic nociceptive. When an injury affects only the skin, the somatic nociceptive pain would be considered superficial (TEIXEIRA; YENG; KAZIYAMA, 2008; ARGOFF; DUBIN; PILITSIS, 2019; PARKER, 2012).
When bleeding occurs in a skin abrasion, it is evidence that the injury has exceeded the epidermis and reached the dermis where there are blood vessels, lymphatic vessels, nerves, and glands present there (PARKER, 2012). However, the pain will still be classified as superficial somatic nociceptive if muscles, bones, tendons, and ligaments are not affected (BARROS; PAULINO, 1999).
Neuropathic pain originates from dysfunction in the peripheral or central nervous system or the inadequate activation of nerves responsible for identifying and transmitting pain (such as nerve compression by a herniated disk or the pain in an already amputated limb, known as phantom limb pain) (TEIXEIRA; YENG; KAZIYAMA, 2008; ARGOFF; DUBIN; PILITSIS, 2019; PARKER, 2012). Argoff, Dubin, and Pilitsis (2019) mention that psychogenic pain is not classified as nociceptive or neuropathic, and therefore, the origin is purely mental, emotional, or psychological. However, they warn that rarely does someone suffer from purely psychogenic pain and people that suffer with such pain actually had chronic pain that was overlooked due to an incorrect assessment.
Another way to classify pain is according to duration which may be acute or chronic. According to the International Association for the Study of Pain, pain is considered acute if it lasts up to three months and chronic if it exceeds that time which is the standard tissue healing time (ARGOFF; DUBIN; PILITSIS, 2019; PREUSS; KALAVA; KING, 2021). Acute pain starts suddenly, with the expectation that it will disappear after elimination of the cause including not recurrence of the pain. Chronic pain consists of repeated stimulation of nociceptors leading to changes in the central nervous system and adaptation to this continuous or recurrent pain (BRASIL, 2001).
The intensity of pain is also an important characteristic to be evaluated. It may be mild, moderate, or severe (ARGOFF; DUBIN; PILITSIS, 2019). However, the subjective and emotional aspects of pain have a critical role interfering with the perception of the intensity. In some cases, there is no need for a stimulus to be captured by nociceptors for pain what could be purely psychological (psychogenic). Moreover, it should be emphasized that even pain that have their origin in a stimulus captured by nociceptors in tissue injury do not constitute pain in itself because it occurs at a subsequent stage after perception that may be emotional and subjective (RAJA, 2021).
Normally, pain is treated by Allopathic Medicine through common analgesics and also with opioids. Each medication has its most appropriate indication and limitations, and moreover, drugs have various side effects, some of which may be very harmful (ANVISA, 2021a; 2021b; 2021c; 2021d; 2021e; 2021f). Opioid analgesics are synthetic drugs that have narcotic effects similar to those of opium-derived products (opioids); when linked to certain receptors in the central nervous system reduce pain signals to the brain (PREUSS; KALAVA; KING, 2021).
Opioids interfere with many organic systems and several bodily functions. Respiratory depression and constipation are common effects requiring care and even motivating their suspension of use (BENYAMIN; TRESCOT et al., 2008). Considering that each person may present a unique response and different levels of pain tolerance, the dosage of an opioid must be administered with caution to achieve adequate pain relief without exceeding limits. Their use is more appropriate when other non-opioid drugs are ineffective. Opioids are more indicated for moderate to severe pain and are usually used in cases of intense acute pain, although they are also used in some cases of chronic pain (PREUSS; KALAVA; KING, 2021).
There are controversies about the long-term use of opioids for non-oncologic chronic pain, due to the risk of dependence and other complications. The use of other less aggressive therapies that are effective instead of allopathic medication is an option that may be considered in a painful condition.
Some potent drugs have aggressive side effects making their use as the first option not viable when there are other less harmful options that are also effective. However, not even some common drugs sold without a prescription and apparently harmless are exempt from causing harm as may be seen in their labels (ANVISA, 2021a; 2021b; 2021c; 2021d; 2021e; 2021f).
Each individual has their own characteristics, allergies, and unique responses. Pain, as a result of subjective perception, is a personal and unique experience (BRASIL, 2001). For example, if a patient has kidney problems great caution is necessary for the use of NSAID (Non-steroidal Anti-inflammatory Drugs) considering their high potential for renal damage, in addition to the hepatic and gastrointestinal damage of this type of drug (ARGOFF; DUBIN; PILITSIS, 2019). A prior analysis of pain and the available treatment tools, verifying the benefit versus risk, is recommended before choosing a therapy or drug. It must be applied especially in cases of narcotics and opioids administration (PREUSS; KALAVA; KING, 2021) requiring adequate medical history to identify the characteristics of the patient’s pain in order to making a direction for the best course of action (ARGOFF; DUBIN; PILITSIS, 2019).
Every medication has pharmacological characteristics that determine its efficacy for each type of pain and the time it takes for the maximum analgesic effect to be achieved after administration. Initially, as the concentration of the active agent of a drug increase in the blood its action in the body becomes greater. There is a point where the concentration, or serum level, reaches the maximum effect after the administration of the medication. The highest plasma level achieved after the administration of a drug in an individual is called the Maximum Plasma Level or Maximum Concentration (Cmax) (LORENZI, 2006).
Paracetamol (acetaminophen) and NSAID are the first options for treating most patients with mild to moderate acute pain, while opioids (which are synthetic products with similar effects to morphine and other opium-derived opioids) such as tramadol are more commonly used for severe acute pain (AMAECHI; HUFFMAN;
FEATHERSTONE, 2021). It is also found that some opioids are especially indicated for moderate to severe chronic pain, such as fentanyl and oxycodone, but the onset of their analgesic effect is slow. Thus, their use become unfeasible for acute pain which requires rapid initial analgesia (ANVISA, 2021a, 2021e, 2021f).
Paracetamol (acetaminophen) and dipyrone (metamizole) are the most prescribed analgesics in Brazil and may be bought without a prescription. However, the health risks are serious what becomes their restricted use in the US and several European countries. For example, these drugs may cause aplastic anemia, gastrointestinal complications, anaphylaxis, and agranulocytosis (QUEIROZ; SANTOS et al., 2013; NORONHA; GURGEL et al., 2009). In the case of paracetamol, when used appropriately, pain relief may begin 15-30 minutes after the use but the greatest effect occurs after the Cmax active ingredient is reached in the blood. To paracetamol, generally takes up to an hour to reach the Cmax, continuing to act for 4-6 hours (ANVISA, 2021b).
Dipyrone (metamizole) is a non-steroidal anti-inflammatory drug that, in addition to being antipyretic and analgesic, acts as a spasmolytic. One hypothesis to explain the analgesic effect is the desensitization of peripheral nociceptors. The analgesic effects of dipyrone occur 30-60 minutes after use. A study called “Dipyrone versus paracetamol in the control of postoperative pain” indicated the superior analgesic efficacy of dipyrone compared to paracetamol (QUEIROZ, SANTOS et al., 2013).
Tramadol (Tramadol hydrochloride) is an opioid that has a central action to inhibit the reuptake of norepinephrine in neurons. In addition, this drug may increase the release of serotonin similar to some antidepressant drugs; its potency is 1/10 to 1/6 of the potency of morphine but analgesic doses usually do not depress the respiratory system, which differs from morphine. It is indicated for moderate to severe pain. According to research, the time it takes to reach the Cmax of tramadol after its administration is: 45 minutes to intramuscular application; one hour related to oral solution; 1,5 hours to pill; 2,2 hours to capsule; 4,9 hours for 100mg of prolonged pill release (ANVISA, 2021d).
Fentanyl is an opioid medication indicated for chronic pain in cases of moderate to severe pain. However, depending on its dosage, respiratory arrest may occur posing a risk to life. The dosage is individualized depending on the intensity of pain and the individual characteristics. Thus, gradual tests are necessary until finding the ideal dosage. This medication is used in the form of a transdermal slow absorption patch. It is contraindicated for acute severe pain because the peak analgesic effect (Cmax) is concentrated between 18-24 hours after application. Therefore, the initial supplementary analgesia must be implemented with another analgesic that has a shorter onset time (ANVISA, 2021e).
Oxycodone is another potent opioid pharmacodynamically comparable to morphine for continuous use in cases of moderate to severe chronic pain. A study mentions that 91% of patients achieved pain control which was reduced to a mild intensity after 1.6 days after administration of this medication. It usually takes about 24-36 hours for plasma elevation; thus, the use is not recommended if there is an immediate need for pain relief. In the initial phase of treatment with oxycodone for chronic pain – similarly to what occurs with Fentanyl – it is necessary to previously use another faster-acting medication (ANVISA, 2021f; LUGO; KERN, 2004). Table 1 shows the indications of use for each medication and the time normally elapsed between the application and the onset of its maximum analgesia (corresponding to Cmax):
Table 1 – Recommendations for the use of each drug related to Cmax.
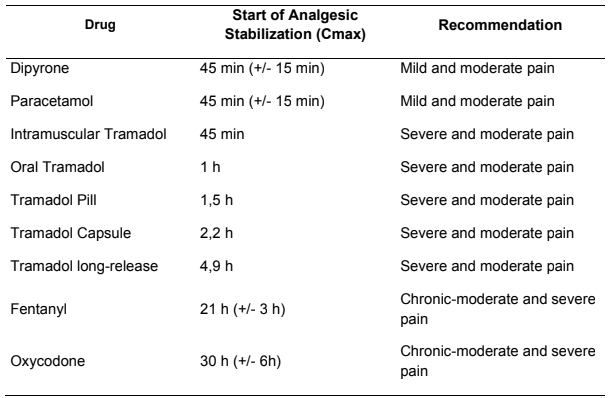
Source: The authors, 2021 (based on the leaflet of the drugs analyzed) (ANVISA, 2021 a,b,c,d,e,f).
Non-pharmacological alternatives may be used for pain relief, such as biophysical treatments including transcutaneous electrical nerve stimulation (TENS), low-intensity lasers, and shock waves. TENS may modify abnormal responses of damaged nerves promoting muscle stimulation and vasodilation which favors pain relief, reduce edema, and stimulate healing. It has been used for chronic and acute pain; its analgesic effect may last from a few minutes to two hours. TENS is commonly used for neurogenic pain and has also been recently applied to wound treatment to accelerate healing and closure of cutaneous lesions (SILVA; LIMA et al., 2017).
TENS has been applied as an adjuvant for pain relief in acute post-thoracotomy pain in patients undergoing thoracic surgery. Freynet and Falcoz (2010) found that TENS applied in conjunction with narcotic analgesics produced good results in 78% of the analyzed articles, contributing to the reduction of medications. Thus, the authors concluded that in the case of thoracic surgery, the association of TENS with postoperative medications is effective for pain relief. They also found that the use of TENS as the sole treatment for mild post-thoracotomy pain was very effective; however, in the case of intense pain, this therapy was ineffective as a standalone treatment.
Low-level lasers (therapeutic lasers) change the metabolic process of affected cells and promote beneficial biological effects through bio-stimulation including analgesic, anti-inflammatory, and healing properties. Depending on the wavelength the results may vary (LINS; LUCENA et al, 2010). There are many studies investigating the effect of laser treatment for various situations. Rocca, Zhao et al. (2018) discuss the effect of laser treatment on aphthous ulcers using devices with different wavelengths. The 635 nm diode laser produced the best result reducing pain during application and maintaining pain relief after treatment. The 450 nm and 808 nm diode lasers reduced pain only after application, with gradual reduction during the following week. However, the Er:YAG (Erbium-Yttrium-Aluminum-Garnet) laser had no lasting effect, as pain relief was only observed during treatment.
In a case study, Misra, Maite et al. (2013) report on a man who had recurrent aphthous stomatitis (RAS) with a burning sensation and whose pain was perceived as being very intense and classified at 80% on the EVA scale. This condition usually recurred three times a month. The patient received laser therapy using a 940 nm diode. After a single session, the patient reported that the pain had been relieved and that no longer felt the burning sensation. Four days later, healing had already occurred, and two months after treatment, there was no recurrence of those symptoms.
Shockwave therapy is another biophysical treatment that involves sending sound waves through the body. It contributes to reducing certain types of inflammation, relieving swelling and local pain. Shockwave therapy also stimulates the formation of collagen and new blood vessels which increases oxygenation in the region that facilitates the repair of injuries. Tendinopathies resulting from excessive sports use are musculoskeletal disorders in which extracorporeal shockwave therapy (ESWT) has been applied for many years. Diabetic and non-diabetic chronic ulcers and other tissue repairs are also treated with this therapy, and most of the scientific articles published on ESWT have shown positive and beneficial effects (WANG, 2012).
The therapeutic system of Medicinal Biomagnetism (MB) uses magnets with a magnetic flux density ranging from 1000 Gauss to 7500 Gauss which is necessary to achieve adequate bioelectric and biochemical balance, useful in pain relief. The system differs from Magnet Therapy which uses low-intensity magnets (usually from 100-500 Gauss) (DURÁN; CASTELÁN; CASTELÁN, 2005). The developer of MB was Isaac Goiz Durán who combined knowledge from various sources to systematize the technique. In addition, Durán added the experience as a physiotherapist and physician, as well as experiences in acupuncture, reflexology, and various other alternative therapies. The training made with Richard Broeringmeyer, a physician of the National Aeronautics and Space Administration (NASA) was also fundamental to the development of this technique (DURÁN, 2020; DURÁN, 2008).
Durán (2020; 2008) reports that Richard Broeringmeyer studied the effects of magnetic fields on living organisms in the 1930; In the 1970 worked for NASA investigating why astronauts’ immunity was very low upon returning from space (leaving them vulnerable to various diseases) and what effect zero gravity had on them. One of Broeringmeyer’s experiments was to balance space professionals with static magnetic fields generated in order to improve their health. Broeringmeyer found that using a medium-intensity magnet it was possible to detect regions corresponding to internal organs or internal parts of the body that were out of balance in terms of pH which could also be corrected with magnets (DURÁN, 2020; DURÁN, 2008).
The MB considers that energetic and bioelectric imbalances are related to disturbances in the potential of Hydrogen (pH) which indicates the level of acidity or alkalinity. It is possible to perceive that there is an electromagnetic and pH imbalance at a point or area of the body by placing the north pole of a medium-intensity magnet in the location. If there is an imbalance there, there will be an involuntary reaction of muscular contraction in the entire right hemisphere of the individual. It may be more easily perceived by visualizing the patient’s feet as there will be a variation in the length of their right leg as a result of the contraction. If there is no imbalance, the organism will not generate the aforementioned reaction and there will be no variation in leg length (MARTINEZ, 2018; 2021; DURÁN; CASTELÁN; CASTELÁN, 2005; DURÁN, 2020; DURÁN, 2008).
According to the theory of magnetoception developed by David Goiz Martinez, the muscular reaction in the right hemibody is due to the neurophysiological withdrawal reflex after activation of specific brain areas (which are more sensitive to bioelectrical changes, stress, and anxiety stimuli) resulting from the bioelectrical reaction caused by the magnetic field of the magnet in the unbalanced point (Martinez, 2018; Bear, Connors, & Paradiso, 2007; Breiter, Etcoff, et al., 1996).
Martinez (2018) points out that the most sensitive area to emotions is the cerebral amygdala including the parietal lobe related to perception of senses. In a situation of danger, fear, or stress, the amygdala area is activated together with the left parietal lobe, as observed in a magnetic resonance imaging study. When people viewed faces with expressions of fear, the cerebral reaction activated these brain structures, as shown in Figure 1 below:
Figure 1 – Response from both amygdala and left parietal lobe during visual processing of fear face expressions.
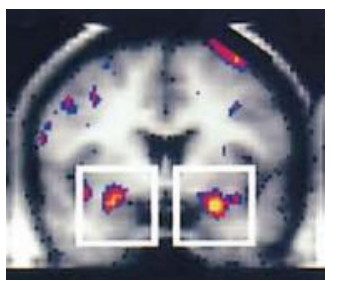
Source: BREITER; ETCOFF et al. (1996).
It is known that the left side of the brain controls the right side of the body and the right side of the brain controls the left side of the body. Therefore, considering that the left parietal lobe becomes activated in response to a stressful stimulus it is clear why it is the right half of the body reacting with an involuntary movement when a bioelectrical stimulus occurs. When a magnet is placed on a point of the body that is in energetic imbalance, the mentioned brain activation occurs together with involuntary muscle contraction in the right half of the body. This contraction also occurs in the right iliopsoas muscle causing a shortening of the right leg which may be observed by looking at the patient’s feet lying on the stretcher (MARTINEZ, 2018; BEAR; CONNORS; PARADISO, 2007; BREITER; ETCOFF et al., 1996).
Biomagnetic Pair (BMP) considers the imbalance of the Hydrogen potential (pH) and measures the energetic variation of specific points in the body where acidity and alkalinity dysfunctions occur outside of physiological limits. Magnetic energy is a tool to restore bioenergetic balance and pH for the benefit of health, including pain relief. It is also considered that the imbalance always occurs in pairs and that an imbalance of pH towards alkalinity in one point corresponds to an imbalance towards acidity in another point, forming a Biomagnetic Pair. Furthermore, there is a vibrational and resonance phenomenon between these two points (DURÁN; CASTELÁN; CASTELÁN, 2005).
To balance dysfunctional resonant points, a point or area of imbalance (scanning point) is detected using the positive pole (north pole) of a magnet. Then, using the positive pole (south pole) of another magnet, the point or area generating the balance (impaction or resonance point) is detected. By keeping the negative magnet applied to the scanning point and the positive magnet applied to the impaction point, a pair of magnets (magnetic pair) is applied to a Biomagnetic Pair in the body. Performed for an appropriate amount of time (dependent on several variables) will contribute to the bioelectric balance of the BMP (MARTINEZ, 2018; 2021; DURÁN; CASTELÁN; CASTELÁN, 2005; DURÁN, 2020; DURÁN, 2008).
If a point has an excess of hydroxide ions (OH–) – corresponding to an alkaline imbalance – and another point with an excess of hydrogen ions (H+) – corresponding to an acid imbalance – there is magnetic resonance between them which these two points will be part of a BMP. Balance may be achieved with a pair of medium-intensity magnets placing the north pole of magnet on the alkaline point and the south pole of another magnet on the acid point. Considering the hypothesis that the mentioned ions move away from their original positions and towards the intermediate point between the two points, a chemical reaction between them may occur, as H+ and OH– combining to form H2O, which is the formula for water. This results in the neutralization of the ions that would be causing the pH imbalance in the two points (MARTINEZ, 2018; DURÁN; CASTELÁN; CASTELÁN, 2005).
Biomagnetic Therapy holds various procedures, strategies, and protocols for applying magnets in different illnesses. Among these, the “Modern Trauma Pair” (MTP) used in various types of pain, inflammation, wound healing, and reduction of edema would be considered as a therapy option for pain relief. The advantage of being simple, non-invasive, and having mild and transient side effects such as relaxation, drowsiness, and increased diuresis is a positive point (MARTINEZ, 2018; 2021). The MTP protocol consists of applying a double magnet (north pole of one magnet next to the south pole of another magnet) at the site of the problem (pain or inflammation), a double magnet in the liver region, and a double magnet in the region near each kidney.
The aim of this study was to verify the effects of the Modern Trauma Pair (MTP) protocol of MB on the relief of severe acute pain and the time for the onset of analgesia after the application of magnets.
MATERIAL AND METHODS
The present investigation is a case study that consists of exploratory, descriptive research with a quantitative approach analyzing the medical record of an individual who received therapy from MB to relieve pain. The research participant is a 51-year-old female from Joaçaba (Santa Catarina state) who was treated with MB for severe acute pain of somatic nociceptive origin. The inclusion criteria were having symptoms of severe acute pain and having previously received MB treatment. The exclusion criteria were using medication in conjunction with MB treatment and not signing the informed consent form.
The medical record of the research participant contains information about the treatment which were collected and analyzed after the exclusion criteria applied. The Visual Analog Scale (VAS) was the instrument used to quantify the intensity of pain felt on the day of treatment, before and after MTP application, as well as the pain felt the day before treatment (PIMENTA; CRUZ, 2006).
According to Martinez, Grassi, and Marques (2011), this scale consists of a line of 10 cm where one border corresponds to “no pain” and the other one to “unbearable pain”. The patient indicates where their pain is on this line. They may be asked the following question: “On a scale of 0 to 10, where 0 means no pain and 10 means the worst pain you can imagine, how is your pain right now?”
The medical record also collected data on the level of interference/impediment of pain in their daily and work activities, as well as the level of sensitivity of wounds to touch and pressure (using a scale from zero to ten), before and after each treatment.
The MB protocol used for treatment was the “Modern Trauma Pair” (MTP) described by Martinez (2018) which consists of applying a double magnet (a north pole and a south pole) of medium intensity simultaneously to the site of pain, the liver region, and the area of each kidney. The recommended application time for MTP is approximately half an hour to an hour; there is no need to remove clothing for magnet placement. The frequency of MTP application may be once or multiple times a day, on consecutive or alternate days, depending on the organism’s response.
RESULTS
The volunteer reported that handled hundreds of concrete blocks without gloves on June 12th and 13th, 2021. Thus, she had all fingers abraded (Figure 2). Despite starting to feel pain she did not take any action during those days to alleviate the discomfort.
Figure 2 – Hands with fingers abraded.

Source: The authors, 2021.
On the 14th day, the pain increased and the sensitivity to touch and pressure also increased to the point where the volunteer could hardly do any of her normal daily activities, as touching anything would increase the pain. She could not – without immense suffering – hold a pen, a fork or even wear clothes.
On the night of the 14th, she could not sleep and spent the following early morning hours awake. On the morning of the 15th, she was undergoing treatment from Biomagnetism Medicine. She reported feeling like “a heart was beating in each of her fingers” as they throbbed so much. She reported that she had not taken any medication or sought medical or hospital treatment. There are no imaging exams to present.
Before starting treatment, visual observation of the lesions and evaluation of pain intensity was carried out using the Visual Analog Scale (VAS). In the most affected fingers (thumb, ring, and middle) where there were some points with signs of bleeding, the patient rated the pain as having a high intensity (10). In the other fingers less injured the intensity was rated as 8 (severe or intense pain).
The research participant was treated with the Modern Trauma Pair (MTP) protocol of MB. This involves a double magnet (one north pole and one south pole) of medium intensity, simultaneously placed on the site of pain, in the liver region, and in the area of each kidney (Figure 3A, 3B, and 3C, respectively).
Figure 3: Modern Trauma Pair (MTP) from Medicinal Biomagnetism
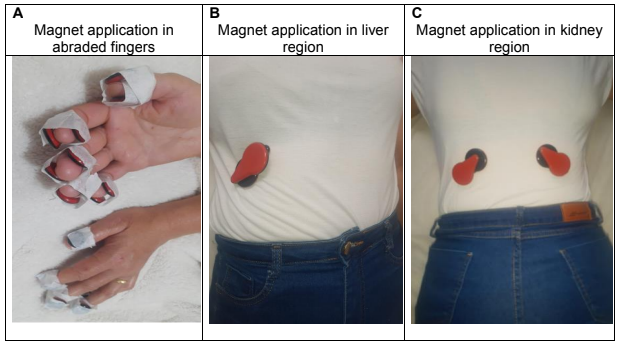
Source: The authors, 2021.
Although the usual application time for this protocol is approximately 30 minutes, it was maintained for one hour due to the intense pain. Ten minutes after receiving the magnet application, the patient reported that the throbbing pain had ceased; analgesia was stabilized 15 minutes after the start of the session. The fingers that had a pain intensity of 8 completely stopped hurting, while those with 10 of pain intensity had reduced to mild intensity (evaluated as being equal to 2).
Later, the patient reported that a few hours after the MB session all fingers were pain-free although they still remained sensitive to touch and pressure. However, she was able to perform several activities on the same day. She was recommended to return for evaluation and treatment two days later. However, if the pain returned, the treatment would be brought forward for a new application of the MB Protocol.
The patient also reported on June 16, 2021 (the day after the session) who continued to have no pain in fingers; the sensitivity to touch and pressure had decreased. Only about 20% of her daily activities were still slightly affected. On the morning of June 17, 2021, she still had no pain; the painful sensitivity to touch and pressure was almost zero. Encouraged by the excellent and rapid improvement, she began to wash and rub clothes without taking proper care causing the scabs to fall off and re-injuring her fingers, interrupting the healing process and generating new pain.
She reported that if this had not occurred, she would have continued to be pain-free that day and probably the next day would be able to wash clothes without problems and perform all her work activities without difficulty or impediment, having received only one application of the MB-MTP protocol.
With the new injury, a new application of the MTP protocol was necessary on June 17. Using the EVA Scale, the pain felt before application was measured as 4 (moderate) for some fingers and 7 (severe) for others. Work activities were again affected by 80%. Immediately after the application, all fingers were pain-free. On the same day, the painful sensitivity to touch and pressure also began to decrease, allowing her to perform about 60% of her normal activities.
On June 22, 2021, she returned and it was found that the injury had completely healed. She reported that since the 20th, she had been able to perform her work activities normally without any hindrance and had not felt pain in her fingers. Therefore, there was no further need for therapy.
Next, tables (Table 2 and Table 3) are presented containing information on the intensity of pain before and after each treatment, as well as the percentage of work activities that were prevented from being performed due to painful interference, both before and after the applications of Medicinal Biomagnetism.
Table 2 – Evaluation of pain intensity by Visual Analog Scale (VAS) in abraded fingers before and after MTP application
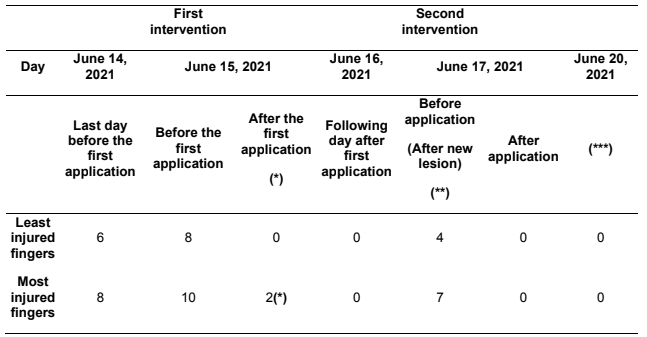
(*) The pain intensity classified as level 10 on the EVA before the application was reduced to 2 by the end of the Biomagnetism session, however, a few hours later on the same day, with the continued effect of the treatment on the body, the pain was completely eliminated dropping to intensity level 0. (**) On the morning of June 17th, 2021, the pain intensity was “0”; however, encouraged by the improvement, as she no longer had any painful sensitivity to pressure or touch, she reported that rubbed her fingers while doing laundry, causing the scab to fall off resulting in bleeding, interrupting the healing process and causing pain with the indicated intensity (moderate/severe). (***) On June 22nd, 2021, she returned for an evaluation appointment, reporting that by the 20th everything was already healed and painless and there was no more painful sensitivity to touch or pressure in her fingers. Source: The authors, 2021.
Table 3 – Pain interference in everyday activities (% of labor impediment)
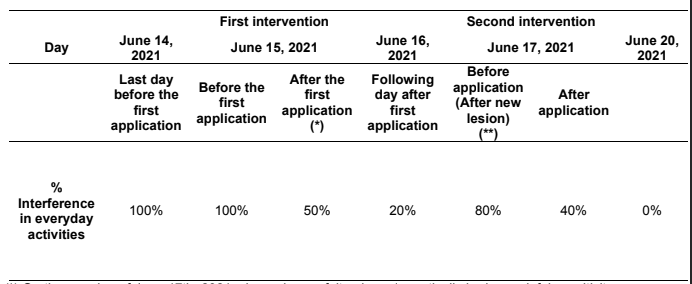
(*) On the morning of June 17th, 2021, she no longer felt pain and practically had no painful sensitivity to pressure or touch; she reports having rubbed clothes and injured her fingers again, causing the scab to fall off the wounds, interrupting the healing process and resulting in bleeding and pain; she got again painful sensitivity to touch and pressure which once prevented 80% of her daily activities on that day. Source: The authors, 2021.
DISCUSSION
As shown in Table 1, there are several drugs for pain relief, that is, for each type of pain there is one or more suitable drugs. The shortest time to onset of analgesic effects (Cmax) for these drugs mentioned are non-opioids (applicable to mild to moderate pain) and it is on average 45 minutes (30 minutes to 1 hour). The minimum time to reach maximum pain relief for opioids ranges from 45 minutes to several hours, depending on the drug and administration form. A non-invasive alternative therapy that may relieve pain quickly and, in less time, than mentioned above may generate great benefit, especially in the case of severe or unbearable acute pain, reducing the suffering time.
There are several alternative and complementary therapies, and among them are biophysical treatments, such as TENS, extracorporeal shock waves, and low-level laser therapy. All these therapies may be used as an option to allopathic medications in pain management. There has also been a combination of drugs with some of these therapies to complement and enhance the effect of medication.
Some of these alternative or complementary treatments have shown positive results in certain situations. For example, according to a case study conducted by Misra, Maite et al. (2013), a single session using 940 nm diode laser was able to completely eliminate severe pain caused by recurrent aphthous stomatitis (RAS), and the symptoms and signs that previously occurred about 3 times a month, disappeared for at least 2 months.
Freynet and Falcoz (2010), after analyzing several scientific articles, reported that TENS was also very effective as the only treatment for mild post-thoracotomy pain; in the case of severe pain, the use of this therapy alone was ineffective. The use of TENS in conjunction with medication contributed to reducing the amount of these drugs.
The use of extracorporeal shock wave therapy (ESWT) as a biophysical therapy has also been employed to treat chronic diabetic and non-diabetic ulcers (which may cause associated pain) and other tissue repairs, with positive and beneficial outcomes (WANG, 2012).
In this case study, Medicinal Biomagnetism (BM) is presented as another option for complementary alternative therapy to promote health and well-being, including pain relief, through the Modern Trauma Pair (MTP) protocol using static magnetic fields.
Three noteworthy studies found in the literature where Medicinal Biomagnetism was applied have reported beneficial results. Two of them refer to the combined use of Medicinal Biomagnetism with another alternative therapy (Insulin Potentiation Therapy – IPT) in cancer patients. The study concludes that 20% of the sample had complete remission with a large portion obtaining partial remission (DAMYANOV; MASLEY; TODOROV, 2019a, 2019b). The third article refers to 13 patients with typhoid fever followed by a positive laboratory test. After a single isolated application of Medicinal Biomagnetism, most of them (10 people) showed negative laboratory results and all of them improved from the symptoms, indicating the potential of this technique (FRANK, 2017).
In this case study, it was observed that in severe acute pain (intensity 8 on the VAS scale) there was total relief in just 15 minutes after initiating the MTP protocol of MB and even in the case of extremely severe pain (intensity 10), it was reduced to mild pain (intensity 2) in the same amount of time; a few hours later, the other fingers also had total relief from the pain.
It was also observed that immediately after the MB session, there was a significant reduction in painful sensitivity to touch and pressure in the participant’s fingers, thus reducing the difficulties or impediments in carrying out daily work activities.
Another relevant finding is that the application of MB did not present harmful side effects, but only mild and transient recovery symptoms, such as drowsiness and increased diuresis, indicating the beneficial effects of static magnetic fields on the body.
Based on the information presented, it is evident that several alternative and complementary therapies are demonstrating positive and beneficial results, including Medicinal Biomagnetism. In this case study that analyzed the application of the MTP protocol of MB for pain relief, excellent results were also observed.
CONCLUSION
This case study demonstrated that the application of the Modern Trauma Pair (MTP) protocol of Medicinal Biomagnetism (MB) improved the participant’s pain and may have therapeutic potential as an innovative complementary alternative for rapid pain relief. With a single application of this protocol – after 15 minutes of initiation – severe acute pain (intensity 8 on the EVA scale) was completely relieved, and the highest severe pain (intensity 10) was reduced to mild pain (intensity 2) with no pain remaining after several hours. The secondary effects are mild, transient, and not harmful, such as drowsiness and increased diuresis. Therefore, it may be concluded that MTP may be an option for pain relief, even in cases of intense acute pain. However, it is not appropriate to generalize the results of this study and further research with significant clinical samples regarding the application of MB is necessary.
REFERENCES
AMAECHI, O.; HUFFMAN, M. M.; FEATHERSTONE, K. Terapia farmacológica para dor aguda. V. 104, n. 1, p. 63-72. 2021. PMID: 34264611. Disponível em: https://pubmed.ncbi.nlm.nih.gov/34264611/. Acesso em: 31 out. 2021
ANVISA – AGÊNCIA NACIONAL DE VIGILÂNCIA SANITÁRIA. Bulário eletrônico. Brasília. 2021. Disponível em: https://www.gov.br/anvisa/pt-br/sistemas/bularioeletronico. Acesso em: 31 out. 2021
ANVISA – AGÊNCIA NACIONAL DE VIGILÂNCIA SANITÁRIA. Bulário eletrônico; paracetamol. Brasília. 2021. Disponível em: https://consultas.anvisa.gov.br/#/bulario/q/?nomeProduto=paracetamol. Acesso em: 31 out. 2021
ANVISA – AGÊNCIA NACIONAL DE VIGILÂNCIA SANITÁRIA. Bulário eletrônico: dipirona. Brasília. 2021. Disponível em: https://consultas.anvisa.gov.br/#/bulario/q/?nomeProduto=dipirona. Acesso em: 31 out. 2021
ANVISA – AGÊNCIA NACIONAL DE VIGILÂNCIA SANITÁRIA. Bulário eletrônico: cloridrato de tramadol. Brasília. 2021. Disponível em: https://consultas.anvisa.gov.br/#/bulario/q/?nomeProduto=CLORIDRATO%20DE%20 TRAMADOL. Acesso em: 31 out. 2021
ANVISA – AGÊNCIA NACIONAL DE VIGILÂNCIA SANITÁRIA. Bulário eletrônico: fentanila. Brasília. 2021. Disponível em: https://consultas.anvisa.gov.br/#/bulario/q/?nomeProduto=citrato%20de%20fentanila. Acesso em: 31 out. 2021
ANVISA – AGÊNCIA NACIONAL DE VIGILÂNCIA SANITÁRIA. Bulário eletrônico: oxicodona. Brasília. 2021. Disponível em: https://consultas.anvisa.gov.br/#/bulario/q/?nomeProduto=cloridrato%20de%20oxico dona. Acesso em: 31 out. 2021
ARGOFF, C. E.; DUBIN, A.; PILITSIS, J. G. Secrets – Tratamento da Dor. 4. ed. Rio de Janeiro RJ. Thieme. 2019. Disponível em: https://books.google.com.br/books?hl=pt-BR&lr=&id=-fGPDwAAQBAJ&oi=fnd&pg=PT3&dq=vis%C3%A3o+geral+da+dor&ots=ebCPFo9Tl c&sig=VrDpj5KHVl4-wolrqFiwP51m2lQ#v=onepage&q=vis%C3%A3o%20geral%20da%20dor&f=false Acesso em: 31 out. 2021
BARROS, C.; PAULINO, W. R. O Corpo Humano. São Paulo, SP: Ática. 1999. 232 p.
BEAR, M. F.; CONNORS, B.; PARADISO, M. Neurociencia La Exploración del Cerebro. 3 ed. Philadelphia, PA, USA: Lippincot Williams and Wilkins. 2007.
BENYAMIN, R; TRESCOT, A. M. et al. Opioid complications and side effects. Pain Physician. v. 11, n. 2, Suppl: S, p. 105-120. 2008. PMID: 18443635. Disponível em: https://pubmed.ncbi.nlm.nih.gov/18443635/. Acesso em: 31 out. 2021
BREITER, H. C. M.; ETCOFF, N. L. et al. Response and Habituation of the Human Amygdala during Visual Processing of Facial Expression. Neuron, Vol. 17, p. 875–887. 1996. doi: 10.1016/s0896-6273(00)80219-6. PMID: 8938120. Disponível em: https://pubmed.ncbi.nlm.nih.gov/8938120/. Acesso em: 31 out. 2021.
BRASIL. Ministério da Saúde. Instituto Nacional de Câncer. Cuidados paliativos oncológicos: controle da dor. Rio de Janeiro: INCA, 2001.
DAMYANOV, C.; MASLEV, I; TODOROV, A. Um Novo Método de Tratamento de Tumores Metastáticos Avançados. Anais de Relatos de Casos Clínicos. Bulgária.
Remedy Publications LLC. v. 4, art. 1647, 2019a. Disponível em: blob:https://web.telegram.org/519a520a-8c14-421e-814d-057349a6d9f7.
DAMYANOV, C.; MASLEV, I.; TODOROV, A. Clinics in Oncology Integrative Oncology at the Clinicist’s Look Chronology for the Creation and Development of the IPT & BMP Method for Treatment of Oncological Diseases. Bulgária.Remedy Publications LLC. v. 4, art. 1671, 2019b. Disponível em: https://www.researchgate.net/publication/338358292_Clinics_in_Oncology_Integrativ e_Oncology_at_the_Clinicist%27s_Look_Chronology_for_the_Creation_and_Develo pment_of_the_IPT_BMP_Method_for_Treatment_of_Oncological_Diseases_OPEN_ ACCESS
DURÁN, I. G. El Par Biomagnético. Universidade de Nuevas Ciencias Médicas. México, 2020.
DURÁN, I. G. O par biomagnético. Universidade de Nuevas Ciencias Medicas. Mexico, 2008.
DURÁN, I. G.; CASTELÁN, G. M.; CASTELÁN, P. M. Par biomagnético, biomagnetismo médico y bioenergética, experiencias de curación, v. 1. 2005. Universidade Autónoma de Chapingo. Mexico, 2005.
FRANK, B. L. Biomagnetic Pair Therapy and Typhoid Fever: A Pilot Study. Med Acupunct. v. 29, n. 5, p. 308-312. 2017. doi:10.1089/acu. 2017.1253 Disponível em: https://pubmed.ncbi.nlm.nih.gov/29067141/ e https://www.scielo.br/j/jbpml/a/Hj6QN7mmmKC4Q9SNNt7xRhf/?lang=pt. Acesso em: 08 dez. 2021.
FREYNET, A.; FALCOZ, P.E. Is transcutaneous electrical nerve stimulation effective in relieving postoperative pain after thoracotomy?. Interact Cardiovasc Thorac Surg. V.10, n. 2, p. 283-288. 2010. doi:10.1510/icvts.2009.219576. Disponível em: https://pubmed.ncbi.nlm.nih.gov/19910359/. Acesso em: 31 dez. 2021.
LINS, D.A.U.; LUCENA, K.C.R. et al. Efeitos bioestimulantes do laser de baixa potência no processo de reparo. An. Bras. Dermatol. 2010. v. 85, n. 6, p. 849-55. 2010. Disponível em: https://www.scielo.br/j/abd/a/PDZDkSSQdZkL5xdjYZh4VVN/?format=pdf&lang=pt. Acesso em: 31 dez. 2021.
LORENZI, T. F. Manual de Hematologia: propedêutica e clínica. 4. ed. Rio de Janeiro: Guanabara Koogan, 2006.
LUGO, R. A.; KERN, S. E. The pharmacokinetics of oxycodone. Journal of pain palliative care pharmacotherapy. v. 18, n. 4, p. 17-30. 2004. doi:10.1300/j354v18n04_03. Disponível em: https://pubmed.ncbi.nlm.nih.gov/15760805/. Acesso em: 31 out. 2021.
MARTINEZ, D. G. Manual del Biomagnetista. Ciudad de Mexico. Biomagnetism Research Institute. 168 p. 2018.
MARTINEZ, D. G. Programa de terapias, cursos y praticas 2021: par biomagnético. Ciudad de Mexico. Biomagnetism Research Institute. 2021.
MARTINEZ, J. E.; GRASSI, D. C.; MARQUES, L. G. Análise da aplicabilidade de três instrumentos de avaliação de dor em distintas unidades de atendimento: ambulatório, enfermaria e urgência. São Paulo: Rev. Bras. Reumatol. v. 51, n.4, p. 299308. 2011. Disponível em: https://www.scielo.br/j/rbr/a/NLCV93zyjfqB6btxpNRfBzJ/abstract/?lang=pt. Acesso em: 31 out. 2021.
MISRA, N.; MAITI, D. et al. nm diode laser therapy in management of recurrent apthous ulcer. BMJ Case Rep. 17 abr. 2013. bcr2012008489. doi: 10.1136/bcr2012-008489. PMID: 23598930; PMCID: PMC3644907. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3644907/. Acesso em: 31 dez. 2021.
NORONHA, V. R.; GURGEL, G. D. et al. Analgenic efficacy of lysine clonixinate, paracetamol and dipyrine in lower third molar extraction: a randomized controlled trial. Med Oral Patol Oral Cir Bucal. v. 14 n.8 p. 411-425. 2009. PMid:19415056 Disponivel em: https://europepmc.org/article/MED/19415056. Acesso em: 31 out. 2021
PARKER, S. O livro do corpo humano. 4. ed. Trad. CERQUEIRA, E. P.; SILVA, A. F. da; CHAGAS, C. F. São Paulo. Ciranda Cultural. 2012.
PIMENTA, C. A. M.; CRUZ, D. A. L. M. da. Crenças em dor crônica: validação do Inventário de Atitudes frente à Dor para a língua portuguesa. Revista da Escola de Enfermagem da USP [online]. v. 40, n. 3, p. 365-373. 2006 Disponível em: https://doi.org/10.1590/S0080-62342006000300008. Epub 26 Fev 2008. ISSN 1980220X. https://doi.org/10.1590/S0080-62342006000300008. Acesso em: 08 dez 2021.
PREUSS, C. V.; KALAVA, A.; KING, K.C. Prescription of Controlled Substances: Benefits and Risks. Stat Pearls. 2021. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30726003/. Acesso em: 31 out. 2021
QUEIROZ, T. P.; SANTOS, P. L. et al. Dipirona versus paracetamol no controle da dor pós-operatória. Revista Odontologia da Unesp. São Paulo (SP). 2013. Disponível em: https://www.scielo.br/j/rounesp/a/HTG5ShBM3VyFnThfk65NbPb/?format=pdf&lang= pt. Acesso em: 31 out. 2021
RAJA, S. N.; CARR, D. B. et al. Definição revisada de dor pela Associação Internacional para o Estudo da Dor: conceitos, desafios e compromissos. Tradução: Sociedade Brasileira para o Estudo da Dor. 2021.
ROCCA, J.P.; Zhao, M. et al. Effect of laser irradiation on aphthae pain management: A four different wavelengths comparison. J Photochem Photobiol B. dez. 2018. v. 189. p. 1-4. 2018. doi: 10.1016/j.jphotobiol.2018.09.016. Epub 2018 Sep 20. PMID: 30268950. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30268950/. Acesso em: 31 dez. 2021
SANTOS, M. S. M. dos. Avaliação da sensibilidade no trajeto do nervo intercostobraquial, em mulheres com linfadenectomia axilar, pós cirurgia por câncer de mama. Dissertação (Mestrado de Enfermagem em Saúde Pública). Escola de Enfermagem de Ribeirão Preto/USP. Ribeirão Preto. 67 p. 2008. Disponível em: https://www.teses.usp.br/teses/disponiveis/22/22133/tde-06082008-143331/publico/MarinaScarulis.pdf. Acesso em: 08 dez.2021
SILVA, S.M. da; LIMA, P.R.C. de et al. Trascutaneous Electrical Nerve Stimulation (TENS) de baixa frequência no processo de cicatrização cutânea em ratos. Pará. Research Medical Journal.2017. v. 1, n.1, p. e09. DOI: 10.4322/prmj.2017.009. Disponível em: https://prmjournal.org/article/10.4322/prmj.2017.009/pdf/prmjournal-1-1-e09.pdf. Acesso em: 08 dez. 2021.
TEIXEIRA, M. J.; YENG, L. T.; KAZIYAMA, H. H. S. (org). Dor: Síndrome dolorosa miofascial e dor músculo-esquelética. São Paulo: Rocca. 2008.
VARANDAS. C. M. B. Fisiopatologia da Dor. Dissertação apresentada à Universidade Fernando Pessoa como parte dos requisitos para a obtenção do grau de Mestre em Ciências Farmacêuticas. Universidade Fernando Pessoa. 2013. Disponível em: http://hdl.handle.net/10284/3955. Acesso em 31 out. 2021.
WANG, C. J. Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res. 20 mar. 2012. v. 7, p.11. 2012. doi: 10.1186/1749-799X-7-11. PMID: 22433113; PMCID: PMC3342893. Disponível em: https://pubmed.ncbi.nlm.nih.gov/22433113/. Acesso em: 31 dez. 2021.
1Studian Graduate Program in Biomagnetism and Bioenergy Applied to Health, Par Magnético Institute – IPM / University Center of Technology of Curitiba – UNIFATEC, Paraná, Brazil.
2Co-supervising Professor Program in Biomagnetism and Bioenergy Applied to Health, Par Magnético Institute – IPM / University Center of Technology of Curitiba – UNIFATEC, Paraná, Brazil.
3Advising Professor Program in Biomagnetism and Bioenergy Applied to Health, Par Magnético Institute – IPM / University Center of Technology of Curitiba – UNIFATEC, Paraná, Brazil.
