Running Head
IMT IN CARDIAC SURGERY PATIENTS
REGISTRO DOI: 10.69849/revistaft/th102410300929
Ângela Maria Rolim Igino1
Fernanda Antico Benetti2
Antônio Carlos Palandri Chagas3
ABSTRACT
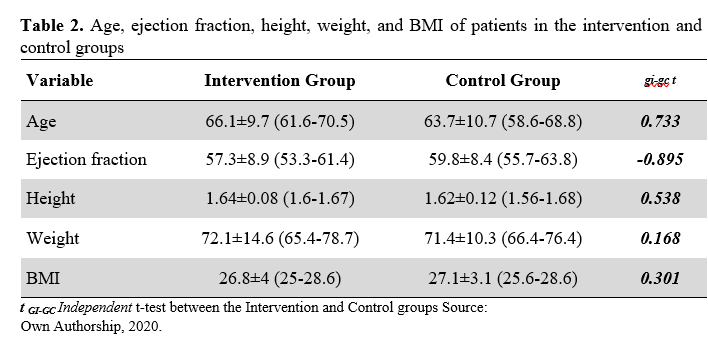
Objective: The purpose of this study was to evaluate the effect of inspiratory muscle training Powerbreathe® in postoperative patients undergoing elective cardiac surgery and cardiopulmonary bypass. Method: A prospective randomized clinical trial was conducted with 40 patients subjected to cardiac surgery, 21 of which were included in the control group, whereas 19 patients were included in the interventional group. Anthropometric data, gender, age, muscle mass index, and height, as well as physiological variables such as systolic and diastolic blood pressure, heart and respiratory rates, peripheral oxygen saturation, were recorded in the early and final stages of inspiratory muscle training. These patients were also evaluated according to the Borg scale of perceived exertion and the visual analog scale for pain in both stages. Results: The research population consisted predominantly of male subjects (75%), most living in urban areas (67.5%) and self-declared as white (50%) or brown (45%). The heart and respiratory rates, as well as diastolic blood pressure presented significantly different when comparing the pre- and post-intervention periods. The intervention group showed a statistically significant increase in the values of maximal inspiratory pressure when considering the 1st and 5th post-surgery. Conclusion: Inspiratory muscle training using Powerbreathe® was capable of improving the maximum inspiratory pressure in postoperative patients undergoing cardiac surgery.
KEYWORDS: Myocardial revascularization. Muscle weakness. Cardiac rehabilitation. Postoperative care. Maximal Respiratory Pressures.
INTRODUCTION
Patients undergoing cardiac surgery are likely to develop a variety of postoperative complications, among which pulmonary complications stand out for impacting postoperative morbidity and mortality, in addition to significantly increasing hospital costs (1).
Major postoperative pulmonary complications include pneumonia, bronchospasm, respiratory failure, prolonged ventilation time (greater than 48 hours), atelectasis, hypoventilation, hypoxia, and infection, which can be associated with preoperative, intraoperative, and postoperative factors (2).
Studies have shown that such pulmonary complications may result from surgeryassociated factors, such as anesthesia, surgical incision, extracorporeal circulation (ECC), ischemia time, the intensity of surgical manipulation, and the number of pleural drains, leading to alterations in pulmonary functions (3).
Postoperative pulmonary dysfunction, a common complication in cardiac surgery patients, is characterized by a reduction in lung volumes and capacities, triggering damage to lung mechanics and resulting in increased respiratory work (4). In addition, the patients present respiratory muscle dysfunction, i.e., their muscles lose the capacity of generating force, culminating in the reduction of maximum inspiratory muscle pressure (5).
The respiratory muscle force can be measured through maximum inspiratory and expiratory pressures (MIP and MEP, respectively). The assessment of these pressures has gained importance due to their great utility in the laboratory, clinics, and hospital environments, as they can be easily verified at the bedside, allowing the assessment of respiratory muscles strength and therefore, can be useful in the determination of diaphragmatic dysfunction (2).
Evidence has demonstrated that cardiac surgery patients have significantly lower MIP values in the postoperative period compared to the preoperative period (5).
Inspiratory muscle training (IMT) is a therapeutic modality with proven results in the gain of MIP, which can influence the performance of the peripheral muscles, improving the physical capacity for walking and sports activities (6).
Currently, TMI has been recommended to increase inspiratory muscle strength in both healthy and sick individuals, as it has effects on the cardiovascular and respiratory systems, improving peak oxygen consumption, preventing dyspnea, and increasing the patient’s quality of life (7).
According to Oliveira (8), Powerbreathe® is a respiratory muscle stimulator that is used to improve inspiratory muscle strength and, consequently, conditioning in athletes and patients with respiratory diseases. Such equipment also allows the performance of muscles to be monitored and evaluated. Although the use of Powerbreathe® has grown significantly worldwide since 2011, this device is still little known in Brazil, which might explain the scarce number of research regarding its use.
Given the importance of pulmonary function rehabilitation associated with inspiratory muscle training, this research aims to evaluate the effectiveness of an inspiratory muscle training program using Powerbreathe®, an innovative therapeutic procedure to optimize the rehabilitation of patients undergoing cardiac surgery.
METHOD
This study was approved by the Research Ethics Committee of the “FACULDADE DE MEDICINA DO ABC – FMABC” Medical School (CAAE: 95272618.2.0000.0082) and all procedures were carried out in accordance with the Declaration of Helsinki. All participants signed the Informed Consent Form (TCLE) one day before surgery. It was registered on the REBEC platform – Brazilian Registry of Clinical Trials, with registration number: RBR942kk6s.
An experimental randomized clinical trial study was carried out in the Heart Hospital of Cariri (HCC), located in Barbalha – CE. The study population consisted of 40 patients who underwent elective cardiac surgery via sternotomy and using CPB, from July 2020 to October 2020.
Inclusion criteria considered patients aged 18 years and older, with left ventricular ejection fraction above 40% and body mass index lower than 30 kg/m2. The study excluded patients who required additional surgery during the postoperative period, as well as those who had complications such as cardiorespiratory arrest, prolonged sedation, mechanical ventilation time greater than twenty-four hours, and neurological complications. Patients who could not understand or collaborate with the procedures were also excluded since the conducts applied in the IMT are volitional. The volunteer patients who participated in this study signed the Informed Consent Form prior to the procedure.
The control group (19 patients) received conventional physical therapy assistance, while and the intervention group (21 patients), in addition to receiving conventional physical therapy assistance, were stimulated with IMT with the linear pressure load resistor Powerbreathe® with a load set at 30% of the MIP obtained on the 1st postoperative day (POD). IMT was applied from the 1st POD to the 5th POD. The IMT protocol consisted of three sets of ten repetitions, each set with 1-minute intervals, twice a day (morning and afternoon).
For the assessment of respiratory muscle strength (RMS), MIP and MEP were measured using manuovacuometry 24h before surgery (preoperative) and 1st POD to the 5th POD (postoperative). These parameters were evaluated after the second IMT of the day. The following data were evaluated and recorded preoperatively: sex, race, age, height, weight, body mass index, and ejection fraction. Physiological variables, including blood pressure, heart rate, respiratory rate, and peripheral oxygen saturation were measured one day before surgery, as well as from the 1st POD to the 5th POD, both before and after each IMT period. The Borg scale of perceived exertion and the visual analog scale (VAS) for pain were applied and their values were recorded in the same period described for the physiological variables.
The data collected during the evaluations were analyzed for normality using the Shapiro-Wilk test and later evaluated by the t-test for paired (before and after) and independent variables (intervention group and control group). These analyzes were performed using the Statistical Package for Social Science for Windows (SPSS, version 25), and the results were presented in tables.
RESULTS
Table 1 shows the sociodemographic parameters of the subjects in the control and intervention groups with regard to gender, race, and place of residence. The variables gender and place of residence were carefully considered in the division of groups in order to minimize their influence on patients’ outcomes.
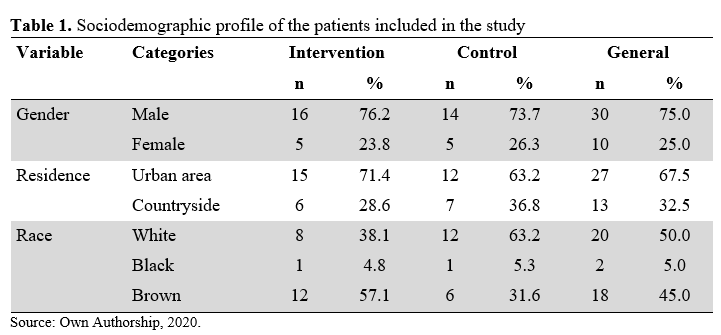
As can be seen, 75% of individuals undergoing myocardial revascularization (MR) surgery with CPB were male. Regarding the area of residence, 67.5% lived in an urban area. Regarding the most frequent race, 50% of the participants were white, followed by brown (45%).
Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), peripheral blood oxygen saturation (SPO2), and respiratory rate (RR) were evaluated only in the patients of the intervention group. In these patients, these measurements were taken before surgery, as well as before and after each of the two daily interventions.
Table 3 shows the results obtained before surgery, pre-intervention (before the first intervention after surgery), and post-intervention (after the last intervention), comparing the results between these three different moments.
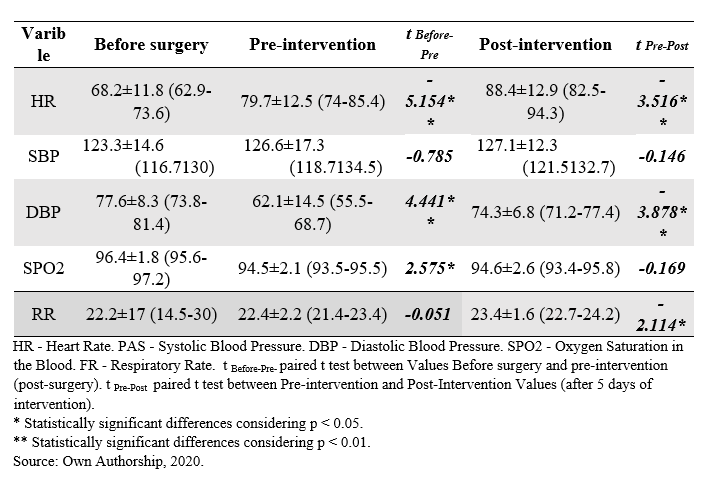
After surgery, statistically significant differences were observed in RR, DBP, and SpO2, while SBP and HR values, despite changing between different moments, did not show statistically significant differences. After the interventions performed (Post Intervention), statistically significant differences were observed in the variables HR, DBP, and RR compared to the period before the first intervention.
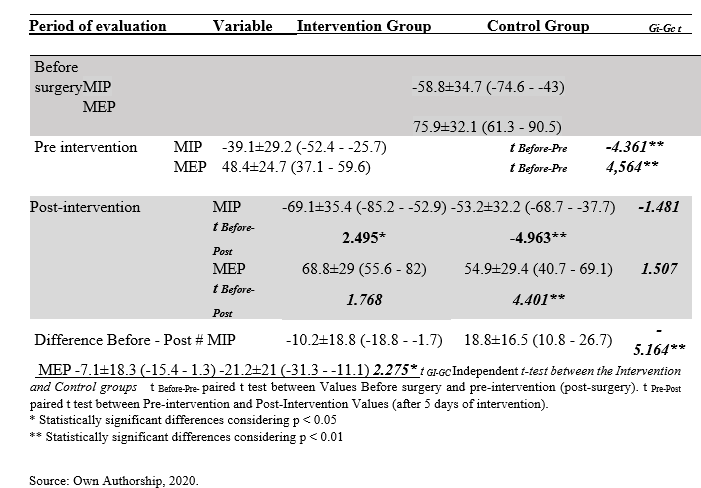
Considering the period immediately after surgery and before performing the first intervention, a statistically significant deficit in the values of MIP and MEP was observed. After 5 days of intervention, there were statistically significant changes in the MIP variable in relation to the pre-intervention time, while in the control group there were statistically significant differences for the in the negativity gain of MIP.
Table 4. Mean, standard deviation, and confidence interval (95%) of the variables HR, SBP, DBP, SPO2 and RF Before surgery, Pre-intervention and Post-intervention. Differences between the moments Before surgery, Pre-intervention, and Pre- and Post-intervention were evaluated with paired t-test.
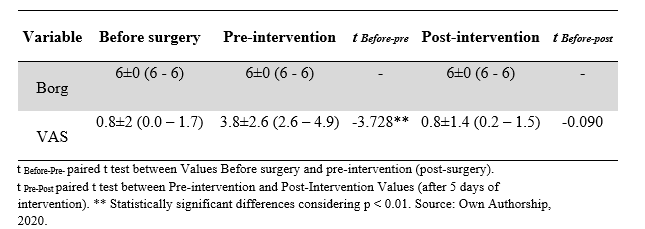
All patients in the intervention group were asked about their perceived exertion based on the Borg scale before and after the intervention. In all evaluation periods, patients reported a Borg value of 6, which was classified as a somewhat difficult task.
Regarding the Visual Analog Pain Scale – VAS, before surgery the mean was 0.8, reaching 3.8 after the surgical procedure, corresponding to a statistically significant increase. However, after 5 days of intervention, the mean value of VAS was 0.8 and, therefore, there was no difference in relation to the period before surgeryThese findings indicate that pain was the symptom presented in the first days after surgery, with the minimum reported pain value being 1 and the maximum being 10 on this scale.
Table 5. Mean, standard deviation, and confidence interval (95%) of the Borg and VAS Scale, Before surgery, Pre-intervention, and Post-intervention. Differences between the moments Before surgery, Pre-intervention, and Pre-and Post-intervention were evaluated with paired ttest.
DISCUSSION
Accordingly, changes in pulmonary function in patients undergoing cardiac surgery through CPB are mostly the cause of morbidity of such patients (1).
In a study conducted by Borba and Gardenghi (4) it was shown evidenced that subjects with respiratory muscle strength deficit have a high risk of developing pulmonary complications after thoracic surgery since IMT is a preventive approach for such adverse occurrences.
Respiratory muscle performance is also impaired after coronary artery bypass graft surgery, a result of a multifactorial phenomenon (9).
In agreement with the previous statement, a study developed by Carneiro et al (12), whose objective was only to evaluate the RMS without performing IMT, showed that the RMS in the preoperative period had a MIP of -60 ± 27.72 cmH2O and MEP of 42 ± 17.35 cmH2O. In the fifth POD, the MIP and MEP found by the authors were -32.5 ± 15.85 cmH2O and 31 ± 12.93 cmH2O, respectively.
In the present study, it was evidenced that the intervention group had decreased MIP values compared to the preoperative period, with a mean of -58.8 ± 34.7 cmH2O, while on the 1st POD the value was -39.1±29, 2 cmH2O. There was a statistically significant increase in MIP from the 1st to the 5th POD, the latter being – 69.1±35.4 cmH2O, which revealed an increase in the negative value of MIP, thus expressing a significant increase in inspiratory muscle strength (p = 0 .02).
The Control group also showed a decrease in the negative value of MIP, when comparing the mean values of the preoperative period (-72 ±34.8 cmH2O) with those of the 5th POD (-53.2±32.2 cmH2O), which highlights the importance of performing the TMI in myocardial revascularization surgery patients.
Significant differences in the MEP values obtained before surgery and after the intervention period also express significant differences between the intervention and control groups, since the expiratory muscle strength loss in the intervention group has a mean of 7.1 cmH2O, while in the control group the mean loss was 21.2 cmH2O, demonstrating that expiratory muscle strength was significantly more preserved in the intervention group.
Study limitations
The limitation of this study was the time factor, as five days of treatment were delimited, with 10 sessions applied using the method tested, as this is the approximate time that patients undergoing cardiac coronary artery bypass grafting remain in the hospital environment.
Funding
This study did not have any type of financing, being fully funded by the authors.
Competing interest
There is no conflict of interest in this study.
CONCLUSION
The findings of this study evidenced that inspiratory muscle training through the linear load pressure resistor Powerbreathe® in these patients provided a gradual increase in the MIP from the first to the fifth POD, ensuring the safety effectiveness of this treatment protocol to increase inspiratory muscle strength.
ACKNOWLEDGEMENTS
To the directors of the Otília Correia Saraiva Foundation, Dr. José Correia Saraiva and Dr. João Correia Saraiva, who allowed this research to be carried out at this Hospital Complex, and to the cardiothoracic surgeon Dr. Samuel Soares Eduardo, who evaluated and surgically treated the patients included in this study.
REFERENCES
- Matheus GB, Dragosavac D, Trevisan P, Costa CE, Lopes MM, Ribeiro GCA. Treinamento muscular melhora o volume corrente e a capacidade vital no pós-operatório de revascularização do miocárdio. Rev Bras Cir Cariovasc. 2012; 27(3): 362-369.
- Borja RO, Campos TF, Oliveira KTS, Freitas DA, Mendonça KMPP. Protocolo de treinamento muscular inspiratório pré-operatório em cirurgia cardíaca eletiva: estudo piloto. Cons Scientia e Saúde. 2012; 11(2): 265-273.
- Menezes TC, Barros JESL, Granja KSB, Exel AL, Calles ACN. Análise da força muscular respiratória no pré e pós-operatório de cirurgia cardíaca: estudo preliminar. Ciênc. Biol. e da Saúde. Maceió. 2016; 3(3): 59-70.
- Borba MA, Gardenghi G. Aplicabilidade do treinamento muscular respiratório no préoperatório e pós-operatório de cirurgia cardíaca. [online]. 2017. Available at:www.ceafi.com.br/publicacoes/download/ade186cf8f2c9c9f402c5e59e3062a6c0.
- Barros GF, Santos CS, Granado FB, Costa PT, Límaco RP, Gardenghi G. Treinamento muscular respiratório na revascularização do miocárdio. Rev Bras Cir Cardiovasc. 2010; 25(4): 483-490.
- Nepomuceno Junior B, Oliveira PRB, Pires TQ, Martinez BP, Gomes Neto M. Efeito do treinamento muscular inspiratório associado a reabilitação física após hospitalização prolongada: série de casos. Rev Pesqui em Fisiot. 2015; 5(3): 237-244.
- Medeiros AI, Costa SKA, Oliveira GWS. A eficácia treino muscular respiratório na fase I de reabilitação cardíaca: Um estudo de caso. Catussaba. 2014; 3(2):65-76.
- Oliveira A, Lima M, Guarda GBM, Proner JA, Kroth AA. Efetividade do treinamento muscular respiratório com POWERBreath® em atletas de basquete. Fisioter. ação. [online]. 2017. Available at: https://editora.unoesc.edu.br/index.php/fisioterapiaemacao/article/view/13262.
- Zanini M, Nery RM, de Lima JB, Buhler RP, da Silveira AD, Stein R. Effects of Different Rehabilitation Protocols in Inpatient Cardiac Rehabilitation After Coronary Artery Bypass Graft Surgery: a randomized clinical trial. J Cardiopulm Rehabil Prev. 2019; 39 (6): E19-E25.
- Guedes GP, Barbosa YRA, Holanda G. Correlação entre força muscular respiratória e tempo de internação pós-operatório. Fisioter. Mov. 2009; 22 (4): 605-614.
- Matheus GB. Influência do treinamento muscular pós-operatório sobre as medidas de desempenho da musculatura respiratória em pacientes no pós-operatório de revascularização do miocárdio. [Dissertação]. Universidade Estadual de Campinas – Unicamp: Campinas, 2012.
- Carneiro CM, Vasconcelos TB, Farias FQ, Barros GG, Câmara TMS, Macena RHM. et al. Estudo da Força Muscular Respiratória em Pacientes Submetidos à Cirurgia Cardíaca em um Hospital na Cidade de Fortaleza/CE. UNOPAR Cient Ciênc Biol Saúde. 2013; 15 (4): 265-271.
1 Centro Universitário Faculdade de Medicina do ABC, Santo André, 09060-870, São Paulo, Brazil
https://orcid.org/0000-0002-0846-8025
*Corresponding author: angela.igino@ebserh.gov.br; Phone: +55 (88) 99940-5754
2 Centro Universitário Faculdade de Medicina do ABC, Santo André, 09060-870, São Paulo, Brazil
https://orcid.org/0000-0003-2620-0759,
3 Centro Universitário Faculdade de Medicina do ABC, Santo André, 09060-870, São Paulo, Brazil
https://orcid.org/0000-0003-4455-6740.
