REGISTRO DOI: 10.5281/zenodo.7689914
Leandro Moraes Pinto1
Rafael Martins Andrade1
Carlos José Dias1,2
Carlos Alberto Alves Dias Filho1,5,6
Andressa Coelho Ferreira1
Alexandro Guimarães Reis5
Mariana Barreto Serra5
Cinthia Daniele Machado de Moraes5
Aécio Assunção Braga5
Nivaldo de Jesus Soares Jr1
Cristiano Teixeira Mostarda1,2,3,4
ABSTRACT
Objectives: To evaluate the blood pressure response after two types of Blood Flow Restriction intensity in healthy women over 60 years of age. Material and Methods: Thirty healthy elderly women aged over 60 years were were randomly assigned to three groups (control placebo: 20% one maximus repetitions + 0% BFR, RF60: 20% one maximus repetitions + 60% BFR and, RF80: 20% one maximus repetitions + 80% BFR) performed the exercises of Leg Press, Elbow Extension, Knee Extension and Elbow Flexion, did the training protocol composed of 3 sets of 15 repetitions, with a 60-second interval between each series. The data were analyzed by Prism 5 with significance level of p<0.05 was adopted. Results: the RF60 group induced a significant decrease in the behavior of Systolic Arterial Pressure (SAP) and Heart Rate (HR) in the period of 24h and 48h after the exercise session, promoting hypotensive responses and bradycardic response in 48h when compared to the initial evaluation baseline. The RF80 group promote changes in SAP in 24 and 48h when compared to baseline but not in Diastolic Arterial Pressure (DAP) and HR. Conclusion: we conclude that acutely 60% and 80% of BFR training was effective in to promote decrease of the blood pressure in the elderly in up to 48 hours after the session.
Key Words: Hemodynamic Responses; Strength Training; Elderly Women; Crhronic deseases; hypertension; Blood Flow Restriction.
INTRODUCTION
Currently, life expectancy around the world is increasing and the population over the age of 60 is the one that has grown the most in comparison with other age groups [1].
This increase in the elderly population and longevity is leading to higher rates of morbidity and mortality, mainly due to changes in dietary patterns and lifestyle, leading to an increase in chronic diseases [2].
One of the main chronic diseases affecting this population is hypertension, with multifactorial causes, characterized by a sustained elevation of blood pressure levels > 140 and / or 90 mmHg [3], as well as being the highest risk of cardiovascular diseases in elderly people [4].
However, even when hypertension is not present in the elderly, an important factor is to be analyzed, it is isolated systolic blood pressure that has values systolic blood pressure above 140 mmHg and diastolic blood pressure below 90 mmHg [5]. It affects 87% of the elderly who are not treated hypertension [6]. One of the main factors responsible for isolated systolic hypertension in the elderly is the increased collagen production [7], an increase in sodium sensitivity and deficiency in production nitric oxide, which leads to vasoconstriction and decreased arterial compliance [8] .
In an attempt to improve the quality life and the reduction chronic diseases in the elderly, more and more have been studying the non-pharmacological strategies that help to improve the quality of life of the elderly [9, 10].
In recent years, despite few studies in the area, in addition to aerobic training, strength training has also been used as an important ally to the physical training program and to reduce the incidence of cardiovascular diseases, mainly because after an exercise session hypotension occurs in both normal and normotensive individuals [11], but there is controversy about the load to be used.
In this sense, emerged a new technique, called Blood Flow Restriction (BFR), that is the exercise with low intensity strength combined with BFR, which assists in the execution of strength exercises to the populations that are unable to perform force exercises with higher loads [12].
In this study we evaluate the blood pressure response after two types of BFR intensity in healthy women over 60 years of age.
MATERIALS AND METHODS
Locations of the study
The familiarization and exercise protocols were performed at the Laboratory of Physiology and Strength Training of the Federal University of Maranhão. All other evaluations were performed at the Laboratory of Cardiovascular Adaptations to the Exercise of the Federal University of Maranhão. All analyzes of the blood samples were performed at Gemma Galgani Laboratory in São Luís do Maranhão.
Subjects
Thirty elderly women aged over 60 years, from the São Luís City from the state of Maranhão, who had no involvement with any training in the six months before the study, were recruited and, as inclusion criteria, healthy elderly women who had not been diagnosed with hypertension and other chronic disease. All participants were informed about the risks associated with the research, in which all signed the informed consent form. The study was approved by the Human Research Ethics Committee of the Federal University of Maranhão (UFMA), Brazil under the protocol number 2.076.159.
The participants of this study were randomly assigned to three groups (control placebo: 20% one maximus repetitions + 0% BFR, RF60: 20% one maximus repetitions + 60% BFR and, RF80: 20% one maximus repetitions + 80% BFR). After randomization, on the first day the participants were submitted to body composition assessment, blood pressure monitoring and blood collection. On the second day it was evaluated the Blood Flow Restriction and Evaluation of Maximum Dynamic Force to estabilish the intensity and percentage of restriction during the exercise. And, o the third day the volunteers were submitted one acute strength training session with blood flow restriction and Hemodynamic evaluation before 1, 24 and 48 hours after exercise session.
Anthropometric variables
The anthropometric measurements were performed on the first day of the participants’ visit to the laboratory and the variables of body weight, height and body mass index were determined. Individuals have been instructed to avoid caffeine, on the day of the evaluations and tests, in which the blood collection was made, blood pressure and heart rate measurements were made before the start of the test. For the measurement of body weight, a digital scale (Balmak®) was used, with a capacity of 150 kilograms and a precision of 100 grams. Stature evaluation was done using a compact vertical stadiometer (Sanny®), type EST 23, on the millimeter scale. The BMI was calculated considering the ratio between body weight (in kg) and height (in meters) squared (kg / m²) and classified according to the World Health Organization [13].
Blood Flow Restriction
For the BFR, pneumatic cuff (WCS® – Cardiomed, 7×80 cm) inserted in the most proximal portion of the upper and lower limbs, more precisely at the deltoid insertion and the inguinal line, respectively, was used during the exercise session position in which Doppler was performed to assess total occlusion pressure. BFR was applied and maintained throughout the exercise session, including in the intervals between sets and released only during exercise change.
Evaluation of maximum dynamic force
To evaluate the strength of the elderly participants in the research and to prescribe the intensity of the training, the test of 1 maximal repetition, applied in the same exercises used during the session, was used. Before the test, participants were shown to perform correctly in order to avoid execution errors during the test and then performed a specific heating (<50% of the estimated maximum load). For the determination of the maximum load, the participants made three to five attempts, with intervals between 3-5 minutes. The weight was increased from two to five kilos, and then a new attempt was made, and the recorded result of the weight lifted immediately before the attempt was not successful.
2.6 Blood collection
Blood collection was performed before the day of the exercise session. Participants were fasted postprandial 2 hours. After a blood collection, it was distributed in 5 ml tubes, a collection tube with separator gel and another with EDTA. The separator gel tube was centrifuged at a rate of 3,500 rpm for 5 minutes to be red cell separation, stored at -20 ° C [14].
Triglycerides (TG), Total Cholesterol (CT), Low-Density Lipoprotein (LDL-C), High-Density Lipoprotein (HDL-C) were carried out on the equipment of the make and model BS-200-E, Mindray, following the manufacturer’s recommendations [14].
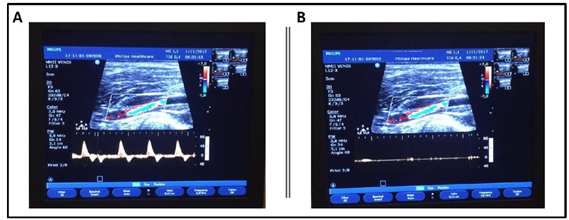
2.7 Total occlusion pressure (TOP)
To evaluate the total occlusion pressure, a vascular Ecocolordoppler apparatus (HD11 XE Revision 2.0.8, Philips Ultrasound, Andover, MA, USA) and a linear array transducer of 5-12 MHz were used to optimize the depth resolution of the arteries. The subjects were placed in the supine position, while a pneumatic cuff (WCS® – Cardiomed), 7 cm wide by 80 centimeters long, the same used during the exercise session, was placed in the right arm at a distance of five centimeters above the fossa to evaluate the total occlusion pressure for the upper limbs and in the inguinal region of the right thigh to assess the total inflated lower limb pressure to the point where the auscultatory pulse of the brachial and popliteal arteries respectively, was interrupted, and the pulse wave generated by the ultrasound image disappeared, guaranteeing the total occlusion pressure. These values were used to calculate the percentage of BFR of the groups during the exercise session, using intensities of 0% (PGC), 60% (RF60) and 80% (RF80%).
Figure 1 : Image of the ultrasound screen before (A) and after (B) the total occlusion
Training protocol used in the session
Participants performed the exercises of Leg Press, Elbow Extension, Knee Extension (Matrix Fitness Systems®, Johnson Health Tech Brazil, Indaiatuba, SP, Brazil), and Low-intensity Elbow Flexion, equivalent to 20% of the maximum dynamic force in all groups. All participants did the training protocol composed of 3 sets of 15 repetitions, with a 60-second interval between each series. A metronome (Tagima®, São Paulo, Brazil) was used to control the execution time, with 2 seconds in the concentric phase and 2 seconds in the eccentric muscle phase.
Hemodynamic variables
To monitor the behavior and obtain the hemodynamic variables, we used a digital blood pressure, and heart rate monitor (Omron ® HEM-705 CP model, Kyoto, Japan) performed at baseline, immediately after, 1, 24 and 48 hours after exercise session. At all blood pressure measurements, participants were rested for a period of 3 to 5 minutes in a calm environment and instructed not to talk at the time of measurement. It was certified that the participants would not be with a full bladder, without the ingestion of alcoholic beverages, coffee and tobacco. At the moment of gauging, participants sat with their legs uncrossed and feet resting on the floor. Blood pressure was measured in the arm, after measuring the arm circumference at the midpoint between the acromion and the olecranon, a cuff was used that was adequate for the circumference of the limb of the participants. The arm was positioned at the level of the heart, supported and with the palm facing upwards. All these steps were performed according to the recommendations of the Brazilian Society of Cardiology [3].
Table 1 : Anthropometric, hemodynamic and metabolic variables of the elderly participants
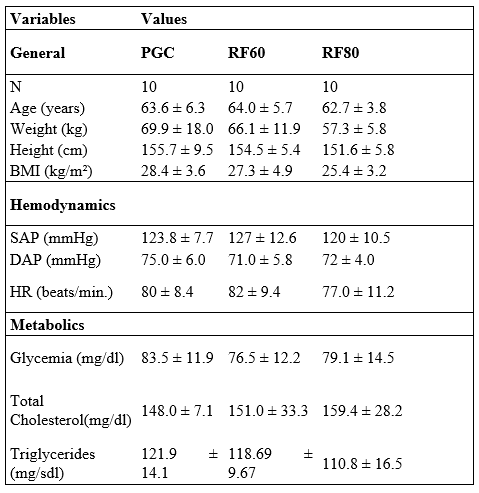
Subtitle: PGC = Placebo control group; FR = Flow restriction; BMI = Body mass index; SAP = Systolic arterial pressure; DAP = Diastolic arterial pressure; HR = Heart rate;
Table 2. Herythogram, Leukogram and Plaquetogram of the elderly participants.
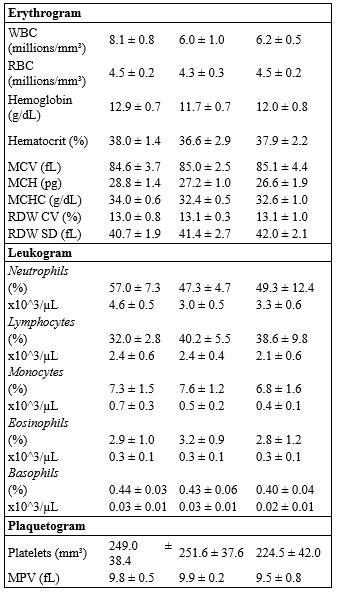
Subtitle: WBC = White blood cells; RBC = Red blood cells; MCV = Mean Corpuscular Volume; MCH = Mean corpuscular hemoglobina; MCHC = Mean corpuscular hemoglobin concentration; RDW = Red cell distribution width; MPV = Mean platelet volume.
Statistical analysis
The data were analyzed by Prism 5 (GraphPad, La Jolla, CA, USA) software. The Shapiro-Wilk test was used to assess data normality, presented the means and standard deviation. To analyze the statistical differences between the groups with standard distribution variables, the unpaired Student t-test. Repeated Measures ANOVA with the Tuckey post hoc test was used to evaluated dependent variables in different conditions. The significance level of p<0.05 was adopted.
RESULTS
The initial evaluation did not present significative difference the anthropometric variables, hemodynamic variables and metabolic variables when compared to the PGC, RF60 and RF80 groups (Table 1), since all groups presented approximate results in the analyzed components. After initial evaluation, the elderly women underwent a single strength training session with BFR at different intensities for posterior analysis of the variables SAP, DAP and HR (Figure 2).
After acute exercise training session the was demonstrate that a single low intensity strength training session (20% of 1RM) does not promote changes in SAP, DAP and HR in the periods: post, 1h, 24h and after 48h of the exercise session when compared to baseline period their SAP and HR results from the initial (baseline) evaluation, being unable to improve them. (SAP = 117±3 in baseline; 125±3 in post; 126±3 in1h; 121±4 in 24h; 118±3 mmHg in 48h / DAP=74±2 in baseline; 75±4 in post; 75±3 in1h; 71±5 in 24h; 72±3 mmHg in 48h / HR= 80±4 in baseline; 79±4 in post; 72±4 in1h; 76±5 in 24h; 79±5 bpm in 48h).
However, the RF60 group induced a significant decrease in the behavior of SAP and HR in the period of 24h and 48h after the exercise session, promoting hypotensive responses ( SAP= 116±3.5 in 24h and 113±4 in 48h vs. 129±2 mmHg in baseline) and bradycardic response in 48h when compared to the initial evaluation baseline ( HR= 74±2 in 48h vs. 82±3 bpm in baseline). However DAP were similar among the period (DAP=71±2 in baseline; 74±4 in post; 71±3 in1h; 75±5 in 24h; 69±3 mmHg in 48h ). From another perspective, there were no improvements in hemodynamic variables in RF80.
Figure 2: Comparative in moments post baseline in groups control, 60% and 80% BFR
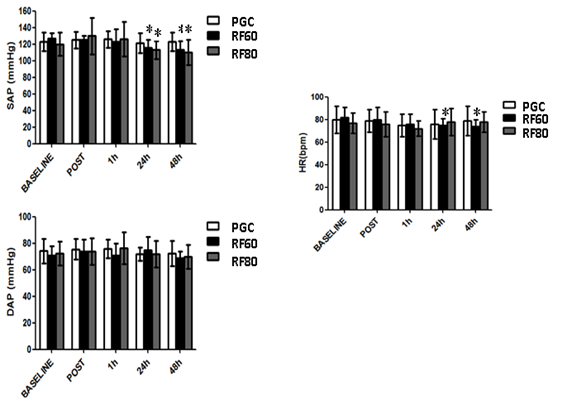
Simillarly RF80 group promote changes in SAP in 24 and 48h when compared to baseline but not in DAP and HR in the periods: post, 1h, 24h and after 48h of the exercise session when compared to baseline period their SAP and HR results from the initial (baseline) evaluation, being unable to improve them. (SAP = 120±3 in baseline; 130±6 in post; 126±5 in1h were similar but 24h= 113±4 and 48h= 111±4 mmHg were lower than baseline period / DAP=72±2 in baseline; 73±4 in post; 76±3 in1h; 71±5 in 24h; 70±3 mmHg in 48h / HR= 77±3 in baseline; 76±4 in post; 72±3 in1h; 78±4 in 24h; 78±2 bpm in 48h).
DISCUSSION
In this study we evaluate the blood pressure response after two types of BFR intensity in healthy women over 60 years of age.
Analysis of the results showed that training with 60% and 80% flow restriction seems to be more efficient in promoting post exercise hypotension when compared to the PGC group. To our surprise , this effect remained until 48 hours after the exercise session.
Additionally, training with a 60% restriction promoted a decrease in heart rate also after the periods of 24 and 48 hours.
Previous studies have reported the hypotensive effect of flow restriction after an exercise session under various conditions. However, we did not find studies comparing the hypotensive effect of up to 48 hours in different percentages of restriction in healthy elderly women.
Similarly, a study with subjects with a mean age of 45 years also analyzed differences in systolic arterial, diastolic arterial pressure and heart rate, however at 15, 30, 45 and 60 minutes after the session. There was a significant decrease in systolic arterial pressure, also showing that BFR training for hypertensive patients is better when compared to low intensity exercises [15]. Different from our study, these authors evaluated middle-aged individuals and not evaluates after 24h. In addition, this study does not describe the percentage restriction of blood flow used during the experiment, as was done in our study.
Another study, using the same technique but not specifying the percentage of BFR, compared to the results of systolic and diastolic arterial pressure and heart rate in 3 groups: 80% of 1 RM, 20% of 1 RM and 20% of 1 RM with low blood flow restriction. After 30 minutes of movement, the 3 groups showed significant reductions in systolic blood pressure. On the other hand, diastolic arterial pressure dropped significantly only after 30 and 60 minutes in the third group [16].
These results corroborate our findings, in which low-intensity exercise with 60% of BFR also led to a significant decrease in systolic arterial pressure. However, there was a significant increase in diastolic pressure, which was not observed in our study.
On the other hand, a training protocol in the upper and lower limbs in normotensive individuals, with and without BFR, found that, right after the protocol, there was an increase in hemodynamic variables, however without significance, and same response was seen in the post-exercise [17]
A group of women with mean age (67 ± 1.7), similar with our study, but with controlled hypertension, participated in 3 protocols: 3 sessions with 10 repetitions at 20% of 1 RM; 3 sessions with 10 repetitions at 65% of 1 RM and exercise without BFR. All 3 sessions had a significant increase in hemodynamic variables when compared with the control group. However, there was an interesting finding, showing that the low-intensity of BFR helps to avoid the valsalva maneuver, thus being a useful tool for strength training [18].
Moreover, in the study that evaluated hypertensive women groups, with 3 types of training: mild strength training; low resistance with restriction and control, and only the first two underwent a training time, verified that the low intensity group with restriction had an decrease in systolic arterial pressure, and it also could be a form of hypertension control [19].
After analyzing these studies, it is verified that the studies were performed with different methodologies, because they follow the hemodynamic variables in different post-exercise times and most do not show the percentage of BFR. On the other hand, our work was carried out with longer periods of 24 and 48 hours, in addition to relativizing the percentage of BFR.
However, all show strength training with BFR has significant hemodynamic differences, being able to be more a form to help in the treatment of cardiovascular diseases.
One possible explanation for the drop in blood pressure after exercise would be the decrease in peripheral vascular resistance [20, 21].
This reduction may be due to the high number of metabolites present in skeletal muscle during and after the exercise session. These metabolites, such as H +, ADP, lactate, CO2, among others, are vasodilators and, when in high concentrations, can trigger a powerful reduction of local blood pressure [22].
On the other hand some authors show that total peripheral resistance significantly changed with flow restriction, but the inhibition of venous return by restriction results in a decrease in cardiac preload during the exercise causing a drop in systolic volume [23]. However, we did not evaluate these variables in our study.
In this way, it is necessary to study the chronic effect in workflow restriction training for auxiliary help to control pressure levels under different conditions is highlighted.
Thus, we conclude that acutely 60% and 80% of BFR training was effective in to promote decrease of the blood pressure in the elderly in up to 48 hours after the session.
REFERENCE
1. Schneider, R.H. and T.Q. Irigaray, O envelhecimento na atualidade: aspectos cronológicos, biológicos, psicológicos e sociais. Estudos de Psicologia, 2008. 25(4): p. 585-593.
2. Passos, V.M.d.A., T.D. Assis, and S.M. Barreto, Hipertensão arterial no Brasil: estimativa de prevalência a partir de estudos de base populacional. Epidemiologia e serviços de Saúde, 2006. 15(1): p. 35-45.
3. Malachias, M.V.B., et al., 7ª Diretriz brasileira de hipertensão arterial. Arq Bras Cardiol, 2016. 107(3): p. 1-103.
4. Martel, G., et al., Strength training normalizes resting blood pressure in 65‐to 73‐year‐old men and women with high normal blood pressure. Journal of the American Geriatrics society, 1999. 47(10): p. 1215-1221.
5. Sociedade, B.d.H.-S., S.B.d. Cardiologia, and S.B.d. Nefrologia, V Brazilian Guidelines in Arterial Hypertension. Arquivos brasileiros de cardiologia, 2007. 89(3): p. e24.
6. Franklin, S.S., et al., Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension, 2001. 37(3): p. 869-874.
7. Safar, M.E., Systolic hypertension in the elderly: arterial wall mechanical properties and the renin–angiotensin–aldosterone system. Journal of hypertension, 2005. 23(4): p. 673-681.
8. Gonzaga, C.C., M.G. Sousa, and C. Amodeo, Fisiopatologia da hipertensão sistólica isolada. Rev Bras Hipertes, 2009. 16(1): p. 10-14.
9. Fountoulakis, K.N., et al., Unipolar late-onset depression: a comprehensive review. Annals of general hospital psychiatry, 2003. 2(1): p. 11.
10. Mostarda, C., et al., Hipertensão e modulação autonômica no idoso: papel do exercício físico. Rev Bras Hipertens, 2009. 16(1): p. 55-60.
11. Umpierre, D. and R. Stein, Efeitos hemodinâmicos e vasculares do treinamento resistido: implicações na doença cardiovascular. Arq Bras Cardiol, 2007. 89(4): p. 256-62.
12. Teixeira, E.L., et al., Efeito do treinamento resistido com oclusão vascular em idosas. RBPFEX-Revista Brasileira de Prescrição e Fisiologia do Exercício, 2012. 6(36).
13. Organization, W.H., Obesity: preventing and managing the global epidemic: report of a WHO consultation on obesity, Geneva, 3-5 June 1997, 1998, Geneva: World Health Organization.
14. Wayne, P., Clinical and laboratory standards institute. Performance standards for antimicrobial susceptibility testing. 2011.
15. Araújo, J.P., et al., The acute effect of resistance exercise with blood flow restriction with hemodynamic variables on hypertensive subjects. Journal of human kinetics, 2014. 43(1): p. 79-85.
16. Neto, G.R., et al., Hypotensive effects of resistance exercises with blood flow restriction. The Journal of Strength & Conditioning Research, 2015. 29(4): p. 1064-1070.
17. Vilaça-Alves, J., et al., Acute Effect of Resistance Exercises Performed by the Upper and Lower Limbs with Blood Flow Restriction on Hemodynamic Responses. Journal of Exercise Physiology Online, 2016. 19(3).
18. Pinto, R.R., et al., Acute resistance exercise with blood flow restriction in elderly hypertensive women: haemodynamic, rating of perceived exertion and blood lactate. Clinical physiology and functional imaging, 2018. 38(1): p. 17-24.
19. Cezar, M.A., et al., Effects of exercise training with blood flow restriction on blood pressure in medicated hypertensive patients. Motriz: Revista de Educação Física, 2016. 22(2): p. 9-17.
20. Fagard, R., Exercise is good for your blood pressure: effects of endurance training and resistance training. Clinical and Experimental Pharmacology and Physiology, 2006. 33(9): p. 853-856.
21. Umpierre, D. and R. Stein, Hemodynamic and vascular effects of resistance training: implications for cardiovascular disease. Arquivos brasileiros de cardiologia, 2007. 89(4): p. 256-262.
22. Smith, R.C. and O. Rutherford, The role of metabolites in strength training. European journal of applied physiology and occupational physiology, 1995. 71(4): p. 332-336.
23. Takano, H., et al., Hemodynamic and hormonal responses to a short-term low-intensity resistance exercise with the reduction of muscle blood flow. European journal of applied physiology, 2005. 95(1): p. 65-73.
1Cardiovascular Exercise Adaptation Laboratory – LACORE, Federal University of Maranhão, Department of Physical Education, São Luís, Brazil.
2Professor – UFMA – Department of Physical Education;
3Cristiano.mostarda@gmail.com, Phone number: 3272-9270;
4Link with the Maranhão State Education Department.
5Faculdade de Medicina – ITPAC SANTA INÊS – AFYA.
6Faculdade Santa Luzia Santa Inês- MA.
