REGISTRO DOI: 10.5281/zenodo.8311109
Hassan Chequer Bou Habib Alcure;
Abdo Magnago de Mattos Junior;
Gabriel Moreira;
Claudio Ferreira Borges;
Juliano Bertollo Dettoni.
Abstract
The project consists of a case report of a patient diagnosed with granulomatous prostatitis confirmed by biopsy but initially with physical examination, radiological and laboratory test results, it appeared to have prostate cancer. A review of the patient’s medical record and examinations were performed. laboratory, radiological and anatomopathological tests were performed to understand how the differential diagnosis of this patient was performed and to discuss the benefits of the study of this pathological entity to the medical community.
1. Introduction
Granulomatous prostatitis is a clinical entity of low incidence and prevalence worldwide, with clinical characteristics that resemble prostate adenocarcinoma in several aspects, requiring histopathological examinations for a safe diagnosis. It was first described in the literature in 1920 by Kinoshita, and until 1993, there were only 6 cases described worldwide [4].
We present here a case of a patient who presented with a confirmed clinical diagnosis of granulomatous prostatitis to discuss the clinical, laboratory, radiological and histopathological similarities and differences of this disease with prostatic neoplasia, its main differential diagnosis.
We reviewed the data from the patient’s medical records and his laboratory, radiological and anatomopathological exams to understand and discuss the differential diagnosis of the disease and the impact of the diagnosis on the quality of life of the patient, addressing physical aspects and mental and functional statuses of the individual.
2. Case description
A 59-year-old farmer who had been previously vasectomized underwent a medical consultation complaining of dysuria and a weak urine stream and voiding effort for 15 days, with sudden onset and spontaneous partial improvement. At the time of the consultation, he complained of left testicular pain. He reported a history of gastric adenocarcinoma and denied a family history of prostate or breast cancer. On physical examination, a nodule was detected in the left apex of the prostate, measuring approximately 2 centimetres. Ultrasound showed a prostate of 30 g with negligible residue, and laboratory tests showed a prostate-specific antigen (PSA) level of 20 ng/ml and abnormal sediment elements (ASE) with 10 leukocytes per high-power field according to microscopic urinalysis. Then, ciprofloxacin was prescribed, and magnetic resonance imaging (MRI) of the prostate was requested.
On MRI, a 41-gram prostate was observed, showing an area of low signal on the right posterolateral base on T2-weighted imaging, insinuating into the seminal vesicle and measuring approximately 1.9 x 1.2 centimetres (Figure 1). A slight irregularity of the prostatic capsule was also detected in a region adjacent to the low signal area. The organ was classified as PI-RADS grade 5 according to the results of the examination.
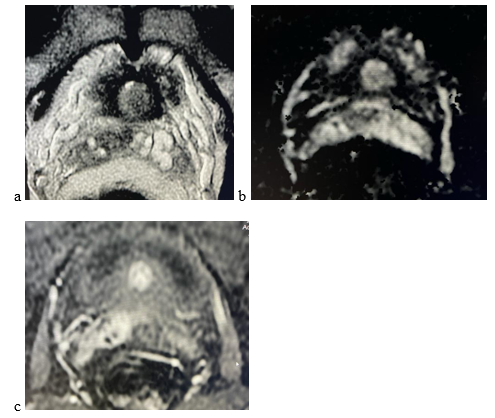
Figure 1. Multiparametric magnetic resonance imaging of the prostate. (a) A low signal area is shown at the right prostatic base on T2-weighted imaging; (b) In the diffusion phase, contrast restriction can be seen; (c) In the perfusion phase, contrast enhancement is visualized in the same location.
The patient then underwent transrectal prostate biopsy, and anatomopathological examination at first showed bilateral marked chronic prostatitis. A slide review was requested, and a new histopathological analysis revealed granulomatous prostatitis (Figure 2).
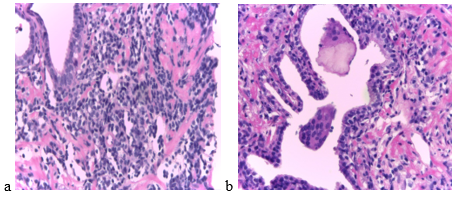
Figure 2. Haematoxylin and eosin-stained slide showing granulomatous prostatitis. (a) Dilated and acini ducts filled with multinucleated giant cells, chronic inflammatory reaction with lymphocytes and histiocytes within the acini epithelium and extension of the infiltrate in the surrounding stroma; (b) Dense lobular infiltrate with fibrous stroma.
The patient progressed with improvement of symptoms and progressive reduction of the PSA level (2.1 ng/ml after 1 month, 1.35 ng/ml after 6 months). An analysis was performed for tuberculosis, which was negative, and computed tomography of the chest showed no changes.
4. Discussion
Prostate adenocarcinoma is the most prevalent nondermatological cancer among men, affecting one in eight men at some point during their lifetime. The mean age at diagnosis is 66 years, and most cases occur after age 65[1,2]. Granulomatous prostatitis does not have a well-defined epidemiology in the literature due to the low number of diagnoses or studies on the disease worldwide.
Both diseases are initially indolent, and in advanced stages, patients may manifest with dysuria, weak urine stream, haematuria or involuntary loss of urine[4]. These symptoms are highly nonspecific and can be found not only in granulomatous prostatitis and prostatic adenocarcinoma but also in other diseases that affect the gland more benignly, such as benign prostatic hyperplasia.
GP can be classified into five groups: (I) associated with systemic granulomatosis (Churg-Strauss syndrome, sarcoidosis, Wegener granulomatosis, etc.); (II) malako-plakia; (III) infective (tuberculosis, syphilis, mycosis, etc.); (IV) idiopathic GP; and (V) iatrogenic (transurethral surgery, BCG therapy);[5]
All these factors highlight the fact that granulomatous prostatitis is an underdiagnosed disease, since anatomopathological examinations are necessary for its definitive diagnosis. In addition, due to the clinicoradiological similarities, granulomatous prostatitis is sometimes diagnosed and erroneously treated as a prostate neoplasia in several cases, resulting in functional impairment to the patient [3]. Thus, there is a clear need to promote the discussion and study of this disease, since lack of knowledge can negatively impact medical practice.
Data availability
The data that support the findings of this case report are available from the corresponding author, Hassan Chequer Alcure, upon reasonable request.
Conflicts of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors’ contributions
Alcure H.C.B.H., Mattos Junior A.M. and Moreira G., were responsible for drafting of the manuscript. Alcure H.C.B.H, Mattos Junior A.M., Borges C.F., and Dettoni J.B. were responsible for conceptualization. Borges C.F., Alcure H.C.B.H, Mattos Junior A.M. and Dettoni J.B., were responsible for the revision of the manuscript. Borges C.F., and Dettoni J.B., were responsible for the supervision. All authors have read and approved the final manuscript.
References
[1] H. Grönberg, “Prostate cancer epidemiology,” The Lancet, vol. 361, no. 9360, pp. 859-864, 2003
[2] R. L. Siegel, K. D. Miller, and A. Jemal, “Cancer statistics, 2019,” CA: A Cancer Journal for Clinicians, vol. 69, no. 1, pp. 7-34, 2019
[3] Y. Ambe, M. Nakamura, N. Shirakawa et al., “Granulomatous prostatitis with high suspicion of prostatic adenocarcinoma on radiological imaging,” IJU Case Reports, vol. 4, no. 4, pp. 247-249, 2021
[4] E. Miękoś, W. Włodarczyk, and S. Szram, “Xanthogranulomatous prostatitis,” International Urology and Nephrology, vol. 18, no. 4, pp. 433-437, 1986
[5] Kitzing YX, Prando A, Varol C, Karczmar GS, Maclean F, Oto A. Benign conditions that mimic prostate carcinoma: MR imaging features with
histopathologic correlation. Radiographics 2016; 36: 162–75.
Hospital Cassiano Antônio de Moraes – Hucam, Federal University of Espírito Santo
Department of Urology at the Federal University of Espírito Santo, Vitória, ES, Brazil
Corresponding author
Correspondence should be addressed to Hassan Chequer Bou Habib Alcure;
hassanalcure1@gmail.com
