KNOWLEDGE ABOUT SCREENING AND EARLY DIAGNOSIS OF CERVICAL CANCER AMONG WOMEN WHO ATTEND AN OUTPATIENT CLINIC AT A UNIVERSITY CENTER IN PORTO VELHO – RO – BRAZIL
REGISTRO DOI: 10.69849/revistaft/cs10202411150407
Júlia Bissoli Alves1
Sabrina Amaral Muniz2
Anna Luiza Castro de Figueiredo3
Natália Moreira de Carvalho4
Rita de Cássia Alves5
Dr. Paulo Ricardo Dell’Armelina Rocha6
Summary
Cervical cancer (CCU) is one of the most common types among women, making early diagnosis essential for better prognoses. It is characterized by slow progression, but it is amenable to screening and rapid detection, which can lead to effective treatment and a promising prognosis. Human papiloma virus (HPV) infection, especially by subtypes 16 and 18, is a necessary but not sufficient condition for the development of cervical cancer. The oncotic cytology test (Pap smear) aims to detect precursor lesions of CCU. This study investigated the level of knowledge about cervical cancer screening and early diagnosis among women attending an outpatient clinic at a University Center in Porto Velho, RO. A qualitative and descriptive approach was used through questionnaires to assess understanding of the preventive exam (Pap smear), risk factors, and preventive practices. The results showed: (i) high adherence to the cervical cancer preventive exam among participants; (ii) non-use of condoms (70%); (iii) educational actions on the preventive exam (60%); (iv) structural and personal barriers limiting access to the preventive exam; (v) 56.7% of participants had information about HPV; (vi) 83.3% of participants reported knowledge of cervical cancer; (vii) lack of knowledge about the frequency of the preventive exam in 55% of participants; (viii) 88.3% believe that early diagnosis improves prognosis and treatment success. The results of this study may help to develop effective educational interventions that encourage the preventive exam, contributing to reducing incidence and mortality rates associated with CCU, and improving women’s health in the region.
Keywords: Cervical cancer. Screening. Early diagnosis. Pap smear. Prevention.
1. INTRODUCTION
Cervical cancer (CCU) is one of the most prevalent cancers among women due to its high incidence. It is characterized by slow progression, but it is amenable to screening and rapid detection, which can lead to effective treatment and a promising prognosis (Ferreira et al., 2021). CCU is the fourth leading cause of death among women worldwide, with estimates of around 570,000 new cases per year and 311,000 deaths estimated in 2018 (Ferreira et al., 2021). In Brazil, the incidence in 2016 was 16,340 cases, which underscores the importance of screening and early diagnosis (Carvalho et al., 2017). Furthermore, CCU was among the ten most prevalent cancers in Brazil, accounting for approximately 5.7% of cancer cases in women in 2022 (INCA, 2022).
The Human Papillomavirus (HPV) is a double-stranded DNA virus, circular, with about 8,000 base pairs (Galloway & Laimins, 2016). These viruses are potentially oncogenic, especially subtypes 16 and 18, and are considered the primary cause of CCU, with an estimated 15 years from the initial phase of infection to the development of dysplasia and subsequent neoplasia (INCA, 2022). However, due to stigmas and cultural patterns embedded in society, adherence to the oncotic cytology preventive exam, which aims to detect precursor lesions of cervical cancer, remains low (Moreira & Andrade, 2018). Additionally, although CCU can be widely prevented, studies have shown that 45.1% of women who have never taken the exam reported not considering it necessary, and 14.8% were not advised to take it (INCA, 2022). These facts highlight the need to strengthen health education and raise awareness about the risks and importance of screening.
Given this issue, this research aimed to investigate the level of knowledge and awareness among women treated at the Integrated Health Center (CIS) of the São Lucas University Center, in Porto Velho – RO, Brazil, about cervical cancer and the Pap smear. In addition, it sought to identify barriers limiting exam adherence and to understand the impact of educational actions in raising awareness about CCU and the preventive exam, providing a brief context and introduction to the topic to be studied or the theme to be addressed in the research project.
2. LITERATURE REVIEW DATA ABOUT CCU
2.1 Epidemiological Context and Relevance of Cervical Cancer
Cervical cancer (CCU) is one of the most common cancers due to its high incidence. It is characterized by slow progression, but it is amenable to screening and rapid detection, which can lead to effective treatment and a promising prognosis (Ferreira et al., 2021).
CCU ranks fourth among the most common types of cancer, and is the fourth leading cause of death among women worldwide, with an estimated 570,000 new cases and 311,000 deaths in 2018 (Ferreira et al., 2021). In Brazil, the estimated incidence of cervical cancer is 16,340 cases, which may vary across regions of the country. Over the years, survival rates for this type of cancer have improved, with global prevalence rates ranging from 50% to over 70%, while in Brazil, it was around 60% (Carvalho et al., 2017).
2.2 Risk Factors and Pathogenesis of Cervical Cancer
Risk factors associated with CCU include infection with HPV, early sexual debut, multiple sexual partners, history of sexually transmitted diseases, immunosuppression, multiparity, low socioeconomic status, prolonged use of oral contraceptives, smoking, and low intake of vitamins A and C (INCA, 2022).
In terms of disease pathogenesis, HPV plays a central role in cervical cancers, presenting more than 40 subtypes that can infect genital mucosa, and among them, at least 15 have oncogenic potential, particularly HPV 16 and 18. Additionally, HPV infection is a necessary but not sufficient condition for CCU development. After infection persists, it takes approximately 15 years from the initial infection phase to the development of dysplasia, primarily affecting the cervix, but it can also impact the vagina, vulva, anus, penis, oropharynx, and mouth (INCA, 2022).
Precancerous lesions of cervical cancer, such as cervical intraepithelial neoplasia (CIN), are identifiable through cytological changes in the Pap smear. These lesions, usually caused by human papillomavirus (HPV), present different degrees of cellular abnormalities, classified from low (CIN 1) to high grade (CIN 2 and 3). Low-grade lesions often correspond to a short-term infection and may regress without intervention. High-grade lesions have a greater potential for malignant progression, and treatment should be preventive to avoid progression to invasive carcinoma. Typical cytological changes include atypical squamous cells of undetermined significance (ASC-US), low-grade squamous intraepithelial lesions (LSIL), and high-grade squamous intraepithelial lesions (HSIL), each requiring follow-up and, in some cases, biopsy for a more accurate diagnosis. The use of HPV tests in conjunction with the Pap smear is recommended for a more precise risk assessment, improving cervical cancer screening and prevention (Cancer.gov, 2020; American Cancer Society, 2020).
2.3 Importance and Effectiveness of Screening: The Pap Smear and Other Methods
The oncotic cytology test, commonly known as the Pap smear, aims to detect precursor lesions of cervical cancer. However, due to stigmas and cultural patterns embedded in society, this preventive method still has low adherence (Moreira & Andrade, 2018).
Furthermore, research has shown that 45.1% of women who have never taken the test reported not finding it necessary, and 14.8% were not advised to take it (INCA, 2022). In this gynecological test, a scraping of the cervix is performed, and a smear is made with cells from the ectocervix and endocervix (Guilar et al., 2015).
An effective cervicovaginal smear can determine the risk of neoplasia development and facilitate diagnosis by identifying changes in the cervix, such as cervical intraepithelial neoplasia, squamous intraepithelial lesions, and dysplasia (Iglesias et al., 2019). The squamocolumnar junction (SCJ) of the cervix is the site where squamous metaplasia (detected by the Pap smear) allows HPV development, which is responsible for about 90% of cervical cancers (Freitas et al., 2023).
2.4 Primary and Secondary Prevention Strategies
The HPV vaccine serves as a preventive measure against cervical cancer only for individuals who received it before the onset of sexual activity. Beyond this context, combating cervical cancer must also involve detecting precursor lesions and ensuring appropriate treatment and clinical follow-up (Nakagawa et al., 2019).
Secondary prevention strategies for cervical cancer focus on the early diagnosis of lesions before they become invasive. This is generally achieved through screening techniques, such as oncotic cytology (Pap smear), colposcopy, cervicography, and, more recently, HPV DNA detection tests in cytological smears or histopathological specimens (Claro et al., 2021).
2.5 Need for Awareness and Challenges in Health Education
Awareness of the importance of preventive and diagnostic exams, such as the Pap smear, is essential for health promotion and the prevention of severe conditions like cervical cancer. Health education plays a crucial role in changing behaviors, contributing to early detection and timely treatment of diseases (INCA, 2022). However, the effectiveness of preventive campaigns faces challenges such as a lack of knowledge and restricted access to quality information. The World Health Organization emphasizes that well-directed educational actions can sensitize the population to the importance of regular care and prevention, promoting greater adherence to essential exams for women’s health (WHO, 2020).
The challenges in health education are numerous, including cultural barriers, social stigma, and limited educational resources in vulnerable communities. According to Pereira et al. (2021), many women still face stigma and misinformation about the preventive exam, reducing adherence to the Pap smear. Additionally, a shortage of trained professionals and infrastructure conditions limit the reach of effective educational interventions. Overcoming these barriers requires innovative and collaborative strategies that involve training healthcare professionals and creating culturally adapted and accessible campaigns to encourage awareness and adherence to preventive care (Pereira et al., 2021).
Objective of the Theoretical Foundation
This theoretical foundation aimed to provide a solid basis on risk factors, the importance of early screening, and the barriers that limit adherence to the preventive exam. This research seeks to contribute data that supports educational actions to inform the female population about the benefits of early diagnosis and the possibilities of effective treatment.
3. METHODOLOGY
The study was characterized as a descriptive qualitative research. The main objective was to analyze knowledge about cervical cancer screening and early diagnosis among women who attended the Integrated Health Center (CIS) of the São Lucas University Center, in Porto Velho, Rondônia State, Brazil. The methodology was established to ensure a detailed and reliable analysis of the participants’ responses, allowing for future reproduction and validation of the research with comparable results.
3.1 Population and Sample
The target population of this study consists of sexually active women up to 64 years of age who attend the CIS of the São Lucas University Center. A voluntary selection was applied to obtain a representative sample. The goal was to establish a diverse group in terms of age range, educational level, and history of preventive exams, following ethical guidelines and the established inclusion criteria.
3.2 Data Collection Instruments
Data collection was conducted through questionnaires, comprising both open-ended and closed-ended questions. These addressed topics such as knowledge about cervical cancer, frequency of Pap smear tests, perceptions and barriers regarding the test, and information about prevention. This type of questionnaire was chosen to facilitate both quantitative and qualitative analysis, allowing for the identification of patterns and changes in knowledge on the subject.
3.3 Data Collection Procedures
The data collection was carried out in person at the CIS, located at the São Lucas University Center. Participants were informed about the research objectives, the way the questionnaire would be applied, and ultimately signed the Informed Consent Form (TCLE). Data collection took place in the second half of 2024.
3.4 Data Analysis
After collection, the data were organized and analyzed with the help of specific software (Microsoft Excel). Open-ended responses were carefully examined to identify themes and patterns that revealed the participants’ perceptions and understanding of cervical cancer. Numerical data were presented in tables and charts, providing a clear and detailed visualization of the results obtained.
3.5 Ethical Procedures
The project was submitted and approved by a Research Ethics Committee (CEP) at São Lucas University Center to ensure that all procedures complied with established ethical standards. The confidentiality and anonymity of the participants were assured throughout all phases of the study to guarantee the participants’ safety. The protocol number was 77028723.6.0000.0013.
4. RESULTS AND DISCUSSION
The results of this study showed a high adherence to the preventive cervical cancer exam among participants, which is a positive indicator of awareness regarding the importance of regular screening for early detection. The 95% approval rate of the exam aligns with previous findings that highlight the positive impact of public health campaigns aimed at encouraging the preventive exam (Silva et al., 2019).
Graphic 01 – Main Questionnaire Responses.
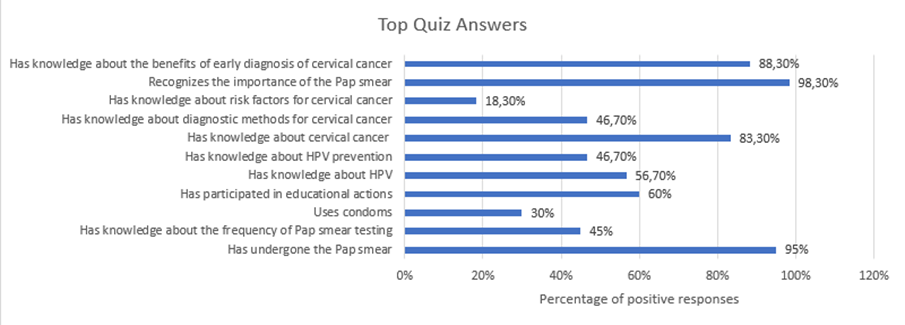
Source: Own authorship
The non-use of condoms, reported by 70% of the participants, demonstrates a risky behavior that increases vulnerability to HPV infection, a risk factor associated with the development of CCU. This behavior is corroborated by previous studies, which suggest the implementation of educational programs aimed at raising awareness about the importance of condom use as a protective measure against sexually transmitted infections (STIs), including HPV, highlighting the need for sexual education actions in health policies to help reduce these risky behaviors (Panobianco et al., 2012).
Participation in educational activities about the preventive exam, reported by 60% of the participants, demonstrates the effectiveness of such activities in raising awareness about cervical cancer. Interestingly, another study emphasized that such initiatives significantly increase adherence to the preventive exam but also pointed out the need to highlight and diversify educational approaches to provide more detailed information about prevention and early diagnosis (Casarin & Piccoli, 2009). This aligns with our study, as despite high adherence to the preventive exam, a lack of knowledge was observed regarding HPV prevention and CCU screening. This suggests that educational campaigns need to be continuous and targeted to provide a broad and detailed understanding of risk factors and preventive strategies.
Regarding barriers to the exam and the main difficulties encountered, lack of availability (28.3%), shyness (23.3%), childcare responsibilities (10%), and professional demands (11.7%) were noted. These data demonstrated structural and personal obstacles that limit access to the preventive exam, an issue already raised by Aguilar & Soares et al. (2015), who pointed out that family responsibilities and time limitations affect acceptance of the preventive exam, especially among low-income women. The need for planning to overcome these challenges is evident; initiatives such as flexible appointment hours and social support for family responsibilities could be effective strategies to increase screening adherence.
Graph 02 – Main results on variables contributing to the lower uptake of the Pap smear exam.
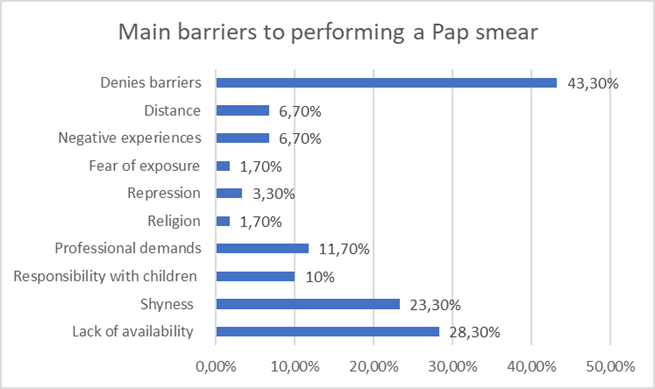
Source: Own authorship
Regarding knowledge about HPV, it was noted that 56.7% of participants had information about HPV, while only 46.7% knew how to prevent it. This is consistent with previous research data, which identified a lack of preventive knowledge about HPV, despite a general awareness of HPV. The authors of this study highlighted that the low level of knowledge about prevention reflects a limited perspective in health campaigns, which repeatedly focus on the preventive exam without seeking to reinforce primary preventive measures. Indeed, increased education about HPV, including the benefits of condom use and the importance of vaccination, is essential to promote awareness and reduce cervical cancer cases (Silva & Lima, 2021).
Although 83.3% of participants reported having knowledge about CCU, more than half (53.3%) did not understand the diagnostic methods for it. This finding resembles previous research where participants had knowledge about the Pap smear, but when asked about the purpose of the cytopathological test, 80.9% of respondents lacked correct knowledge about the procedure; 68.1% believed the exam serves to prevent diseases in general, 10.7% thought it was for treating vaginal infections, and 2.1% were unsure about the topic. Therefore, it is suggested that a significant portion of women were unaware of the exam’s purpose, which is a tool for detecting cellular changes in the cervix that may indicate the presence of cervical cancer or precursor conditions of CCU (Santiago, Andrade, & Paixão, 2014).
The lack of knowledge about the recommended frequency of the preventive exam, reported by 55% of participants, also indicates a communication error regarding medical recommendations, which is crucial for early detection. Previous studies already report that women have inadequate knowledge about the Pap smear, with some research participants never having heard of the preventive exam, or having heard of it but not knowing its purpose or the necessary care for its performance and frequency. Thus, a lack of understanding about the frequency of the preventive exam contributes to lower adherence, compromising timely identification of precancerous lesions. Intensifying guidance on the recommended frequency can be a practical intervention to improve adherence and the impact of screening (Melo et al., 2019).
The near-unanimous recognition (98.3%) of the importance of the preventive exam is a relevant finding, but the lack of knowledge about risk factors associated with cervical cancer, with 81.7% of participants unaware of these factors, indicates a significant gap in public health policy guidance. In fact, previous studies have already reported awareness gaps, noting that half of the women questioned identified only two (multiple partners and poor diet) among the various risk factors for CCU (early sexual activity, low socioeconomic status, multiparity, multiple partners, smoking, long-term use of oral contraceptives, and HPV infection). Therefore, for greater adherence to prevention strategies, it is necessary for women to have a broader understanding of the risk factors for CCU development (Chiconela & Chidassicua, 2017).
Finally, 88.3% of participants believe that early diagnosis improves prognosis and treatment success, a finding aligned with the literature that reinforces the importance of screening for patient survival (Ferreira et al., 2021). This demonstrates a significant level of awareness about the benefits of early diagnosis, but gaps in areas such as condom use and HPV knowledge reveal a challenge still present in health promotion. Indeed, although advances in awareness of cervical cancer are evident, improvements in knowledge about primary prevention measures and diagnostic methods are still essential, requiring constant educational strategies tailored to population needs (Ferreira et al., 2021).
The results of this study indicate a satisfactory level of adherence to the preventive exam, while also exposing a superficial understanding of CCU and identifying significant barriers and other knowledge gaps that need to be addressed to improve prevention and early diagnosis of the disease. Therefore, public health campaigns are recommended that consider the identified gaps and incorporate approaches to broadly disseminate information, from condom use and HPV vaccination to communication about procedures and the frequency of the preventive exam, to strengthen preventive practices and reduce CCU incidence and mortality in the population.
5. CONCLUSION
The study revealed that misinformation and doubts persist regarding knowledge about risk factors, recommended frequency, and the objectives of early diagnosis. It is essential for such programs to include information about the risk factors and pathophysiology of cervical cancer, explaining the importance of preventive measures and vaccination. Similarly, it is crucial to prepare healthcare professionals to act as facilitators of this knowledge, providing detailed and accessible guidance to enhance the impact of public health campaigns, thereby promoting a deeper understanding among patients.
Data analysis demonstrated a lack of knowledge among participants regarding fundamental aspects of cervical cancer screening and diagnosis. Therefore, to reduce the incidence and mortality of this cancer, it is vital that campaigns adopt a more informative and culturally adapted approach, going beyond warnings about CCU and focusing on the importance of regular preventive exams.
Furthermore, it is necessary to strengthen infrastructure, extend service hours, and develop strategies to overcome the stigma and cultural barriers associated with the gynecological exam. These measures aim to create a better-informed and empowered female population, consolidating preventive practices and adherence to screening and diagnosis for cervical cancer, with a direct impact on the quality of life and health of women in the region.
6. REFERENCES
AGUILAR, Rebeca Pinheiro; SOARES, Daniela Arruda. Barriers to Pap Smear Testing: perspectives of users and professionals of the Family Health Strategy in the city of Vitória da Conquista-BA. Physis: Revista de Saúde Coletiva, Rio de Janeiro, v. 25, n. 2, p. 359-379, 2015. Available at: https://www.scielo.br/j/physis/a/X8LrndjnkY6tM9ZR5WfRd7C/?format=pdf&lang=en. Accessed on: Nov. 4, 2024.
AMERICAN CANCER SOCIETY. Cervical Cancer Prevention and Early Detection. 2020. Available at: https://www.cancer.org/cancer/cervical-cancer/prevention-and-early-detection.html. Accessed on: Oct. 29, 2024.
AZEVEDO E SILVA, G.; DAMACENA, G. N.; RIBEIRO, C. M.; ALCANTARA, L. L. M.; SOUZA JR, P. R. B.; SZWARCWALD, C. L. Pap Smear in Brazil: analysis of the National Health Survey in 2013 and 2019. Revista de Saúde Pública, São Paulo, v. 57, p. 55, 2023. DOI: 10.11606/s1518-8787.2023057004798.
CANCER.GOV. Cervical Cancer Screening (PDQ®️) – Patient Version. 2020. Available at: https://www.cancer.gov/types/cervical/patient/cervical-screening-pdq. Accessed on: Oct. 29, 2024.
CARVALHO, J. P.; REIS, R.; DERCHAIN, S. F. M.; SILVA FILHO, A. L. Screening, diagnosis, and treatment of cervical cancer. Série Orientações e Recomendações FEBRASGO, v. 1, n. 2, Jan. 2017.
CHICONELA, F. V.; CHIDASSICUA, J. B. Women’s knowledge and attitudes toward the preventive cervical cancer exam. Revista Eletrônica de Enfermagem, v. 19, p. a23, 2017. Available at: http://dx.doi.org/10.5216/ree.v19.41334. Accessed on: Nov. 2, 2024.
CLARO, I. B.; LIMA, Luciana D. de; ALMEIDA, P. F. de. Guidelines, prevention strategies, and cervical cancer screening: experiences from Brazil and Chile. Ciência & Saúde Coletiva, v. 26, p. 4497-4509, 2021.
FERREIRA, M. de C. M. et al. Early detection and prevention of cervical cancer: knowledge, attitudes, and practices of Family Health Strategy professionals. Ciência & Saúde Coletiva, v. 27, n. 6, p. 2291–2302, Jun. 2022.
FREITAS, V. C. A. de et al. Cervical cytology and sample adequacy: a randomized controlled clinical trial. Acta Paulista de Enfermagem, v. 36, p. eAPE00972, 2023.
GALLOWAY, D. A.; LAIMINS, L. A. Human papillomaviruses: the role of virus and host factors in cancer progression. Current Opinion in Virology, v. 19, p. 109-115, 2016. DOI: 10.1016/j.coviro.2016.06.004.
GUILAR, R. P.; SOARES, D. A. Barriers to Pap Smear Testing: perspectives of users and professionals of the Family Health Strategy in the city of Vitória da Conquista-BA. Physis: Revista de Saúde Coletiva, v. 25, n. 2, p. 359–379, Apr. 2015.
IGLESIAS, Gabriela A. et al. Knowledge and adherence to Pap smear among women in a Primary Health Care network. Rev. Ciênc. Méd., [s.l.], n. 1, ed. 28, p. 21-30, 2019. DOI: http://dx.doi.org/10.24220/2318-0897v28n1a4008. Available at: https://docs.bvsalud.org/biblioref/2020/01/1047801/med-3-00_4008.pdf. Accessed on: Oct. 7, 2023.
INSTITUTO NACIONAL DE CÂNCER (Brazil). Estimation 2023: cancer incidence in Brazil. Rio de Janeiro: INCA, 2022. 160 p. ISBN 978-65-88517-09-3.
INSTITUTO NACIONAL DE CÂNCER (INCA). Estimation 2022: Cancer Incidence in Brazil. INCA, Ministry of Health, Brazil, 2022. Available at: https://www.inca.gov.br
INSTITUTO NACIONAL DE CÂNCER. Cervical Cancer. Instituto Nacional de Câncer (INCA), 2023. Available at: https://www.gov.br/inca/pt-br/assuntos/cancer/tipos/colo-do-utero. Accessed on: Oct. 6, 2023.
INSTITUTO NACIONAL DE CÂNCER. Cancer Prevention and Surveillance Coordination. Estimation 2014: Cancer Incidence in Brazil. Rio de Janeiro: INCA, 2016. Available at: http://www.saude.sp.gov.br/resources/ses/perfil/gestor/homepage/outros-destaques/estimativa-de-incidencia-de-cancer-2014/estimativa_cancer_24042014.pdf. Accessed on: Oct. 6, 2023.
INSTITUTO NACIONAL DE CÂNCER. José Alencar Gomes da Silva Cancer Institute (INCA), Cancer Prevention and Surveillance Coordination. Data and figures on cervical cancer. Annual Report 2022 [Internet]. Rio de Janeiro: INCA, 2022. Available at: dados_e_numeros_colo_22setembro2022.pdf (inca.gov.br).
INSTITUTO NACIONAL DE CÂNCER. Cervical Cancer Prevention. Instituto Nacional de Câncer (INCA), 2022. Available at: https://www.gov.br/inca/pt-br/assuntos/gestor-e-profissional-de-saude/controle-do-cancer-do-colo-do-utero/acoes/prevencao. Accessed on: Oct. 7, 2023.
MELO, E. M. F.; LINHARES, F. M. P.; SILVA, T. M.; PONTES, C. M.; SANTOS, A. H. S.; OLIVEIRA, S. C. Cervical cancer: knowledge, attitude, and practice on the prevention examination. Revista Brasileira de Enfermagem, v. 72, suppl. 3, p. 25-31, 2019. DOI: 10.1590/0034-7167-2017-0645.
MOREIRA, A. da S.; ANDRADE, E. G. da S. The importance of the Pap smear test in women’s health. Revista de Iniciação Científica e Extensão – REIcEn, [s.l.], p. 267-271, 2018. Available at: https://revistasfacesa.senaaires.com.br/index.php/iniciacao-cientifica/article/view/94/56. Accessed on: Sep. 8, 2023.
NAKAGAWA, J. T. T.; SCHIRMER, J.; BARBIERI, M. HPV virus and cervical cancer. Revista Brasileira de Enfermagem, v. 63, n. 2, p. 307–311, Mar. 2010.
WORLD HEALTH ORGANIZATION (WHO). Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Geneva: WHO, 2020. Available at: https://www.who.int
PANOBIANCO, Marislei Sanches; LIMA, Aline Daiane Faim de; OLIVEIRA, Iácara Santos Barbosa; GOZZO, Thais de Oliveira. Knowledge about HPV among nursing students. Texto & Contexto – Enfermagem, Florianópolis, v. 22, n. 1, p. 201-207, Jan./Mar. 2013. Available at: https://www.scielo.br/j/tce/a/X8LrndjnkY6tM9ZR5WfRd7C/?format=pdf&lang=en. Accessed on: Nov. 4, 2024.
PEREIRA, L. M.; SILVA, R. J.; SANTOS, C. A. Barriers in access and adherence to the Pap smear test: a literature review. Revista Brasileira de Saúde Materno Infantil, v. 21, n. 1, p. 56-63, 2021. Available at: https://www.scielo.br.
SANTIAGO, T. R.; ANDRADE, M. S.; PAIXÃO, G. P. N. Knowledge and practice of women attended at the family health unit regarding the Pap smear. Revista de Enfermagem da UERJ, v. 22, n. 6, p. 822-829, 2014.
SILVA, Ana Paula de Oliveira; SANTOS, Ana Paula dos; LIMA, Ana Paula de Oliveira; et al. Early detection and prevention of cervical cancer: knowledge, attitudes, and practices of Family Health Strategy professionals. Ciência & Saúde Coletiva, Rio de Janeiro, v. 27, n. 6, p. 2291-2302, 2022. Available at: https://www.scielo.br/j/csc/a/Z3tXcyhpMP6MLcJzTCmq9bn/. Accessed on: Nov. 4, 2024.
SILVA, Valéria Rufino da; LIMA, Luciene Ferreira de. Human Papillomavirus (HPV) and cervical cancer: understanding among students at the decentralized unit of Campos Sales – CE. Revista da Biologia, São Paulo, v. 20, n. 1, p. 4-9, 2020. Available at: https://www.revistas.usp.br/revbiologia/article/download/158327/164303/445093. Accessed on: Nov. 4, 2024.
1Júlia Bissoli Alves, Medical Student at the São Lucas University Center – Campus I, email: juliabissolialves@hotmail.com
2Sabrina Amaral Muniz, Medical Student at the São Lucas University Center – Campus I, email: sabrinaamaralmuniz@gmail.com
3Anna Luiza Castro de Figueiredo, Medical Student at the São Lucas University Center – Campus I, email: annaloloca@hotmail.com
4Natália Moreira de Carvalho, Medical Student at the São Lucas University Center – Campus I, email: moreiran746@gmail.com
5Dr. Rita de Cássia Alves, Master of Science, Faculty Member at the São Lucas University Center, email: Rita.alves@saolucas.edu.br
6Dr. Paulo Ricardo Dell’Armelina Rocha, Ph.D. in Veterinary Sciences, Faculty Member at the São Lucas University Center, email: ricardodellarmelina@gmail.com
