REGISTRO DOI: 10.69849/revistaft/ar10202201311208
Juciane Valentim
Abstract
The COVID-19 pandemic, declared in 2020, has led to the rapid use of various treatments to combat the disease, often based on limited preliminary evidence. This urgent approach has introduced significant challenges related to drug interactions and polypharmacy, as the simultaneous use of COVID-19 therapeutics and medications for pre-existing comorbidities can increase the risk of adverse drug reactions (ADRs) and complicate clinical outcomes. Studies have examined the risks associated with drug interactions between COVID-19 treatments and other medications. Hodge et al. (2020) explored drug interactions in critically ill COVID-19 patients using experimental therapies. Their findings emphasized the need for careful management of high-risk medications such as lopinavir/ritonavir and hydroxychloroquine due to concerns like QT interval prolongation. Similarly, Plasencia-García et al. (2020) reviewed interactions between COVID-19 treatments and antipsychotics, finding that while some antiviral agents could be safely co-administered with antipsychotics, others required caution due to risks of QT prolongation and hematological issues. Davoutis et al. (2023) focused on the potential interactions between antidepressants and COVID-19 medications, highlighting that while some treatments, like monoclonal antibodies, pose lower risks, others, such as remdesivir and Nirmatrelvir-Ritonavir, carry a higher risk for serious interactions. Cuomo et al. (2023) examined the increased use of psychotropic medications during the pandemic and the DDIs that may arise, emphasizing the need for vigilant monitoring and dose adjustments. Awortwe and Cascorbi (2020) investigated interactions between COVID-19 treatments and medications for comorbidities, revealing that comorbid conditions like cardiometabolic syndrome and chronic kidney disease are associated with worsened clinical outcomes. Kumar and Trivedi (2020) highlighted how the pandemic’s hyperinflammatory state impacts drug metabolism, underscoring the need for continued research and evidence-based treatment protocols. Overall, these studies stress the importance of rigorous pharmacological monitoring, adherence to evidence-based guidelines, and ongoing research to ensure the safe and effective treatment of COVID-19 patients, especially those with complex medication regimens and comorbidities.
Keywords: Drug-Drug Interactions (DDIs); COVID-19 Treatments; Comorbidities; Pharmacological Monitoring; Evidence-Based Guidelines.
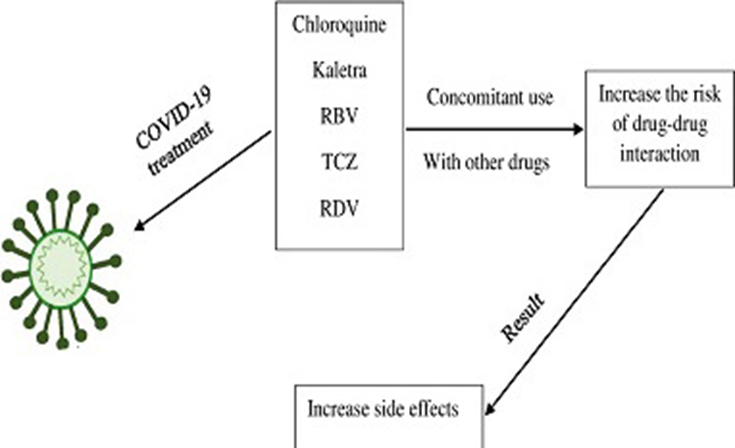
Since the onset of the COVID-19 pandemic in 2020, the urgent need for effective treatments has led to the emergency use of a range of medications, often with limited supporting evidence. This approach, while crucial given the global health crisis, has introduced significant challenges related to drug interactions and the risks of combining multiple therapies. Drug interactions occur when one medication affects the action of another, potentially enhancing or diminishing its effects and increasing the risk of adverse reactions. This issue is particularly critical in COVID-19, where patients may be prescribed antivirals, corticosteroids, anticoagulants, and other supportive treatments, especially those with pre-existing conditions who are already on multiple drugs.
The early use of treatments such as hydroxychloroquine, ivermectin, and azithromycin was often based on preliminary studies rather than robust clinical trials, raising concerns about unknown drug interactions. The common practice of polypharmacy in patients with comorbidities like hypertension, diabetes, and heart disease further complicates this issue. For example, drugs such as remdesivir and tocilizumab, metabolized by the liver, may interact with other medications that share the same metabolic pathways, leading to altered drug levels and affecting their safety and efficacy. Potential risks from drug interactions include serious adverse effects such as liver and kidney toxicity, cardiac arrhythmias, and neurological disorders. Additionally, drug interactions can compromise therapeutic efficacy by interfering with the absorption, distribution, metabolism, or excretion of medications, potentially increasing the risk of hospitalization and, in severe cases, mortality. To mitigate these risks, rigorous pharmacological monitoring is essential, particularly for patients at high risk of interactions. Evidence-based treatment protocols should be prioritized, utilizing medications with established safety profiles, and continuous education for healthcare professionals is necessary to effectively manage and adjust treatments.
The study by Hodge et al. (2020) highlights the risks of drug interactions in critically ill COVID-19 patients, particularly when using experimental therapies. By searching ClinicalTrials.gov, the authors identified 249 drugs and categorized their interactions into different risk levels. Medications such as lopinavir/ritonavir, chloroquine, and hydroxychloroquine were found to have significant interaction risks, especially concerning QT interval prolongation. The study provided a database of these interactions to aid in medication review, emphasizing the need for careful management of these therapies.
Plasencia-García et al. (2020) focused on the careful management of symptoms like anxiety and delirium in COVID-19 patients, especially when antipsychotics are used concurrently. Their systematic review assessed drug interactions between COVID-19 treatments and antipsychotics, identifying that while some drugs could be safely combined, others, such as chloroquine and hydroxychloroquine, posed higher risks. The study called for evidence-based guidelines to help clinicians select safe treatment combinations and monitor patients effectively.
Davoutis et al. (2023) examined the potential interactions between antidepressants and COVID-19 therapies, noting that while some COVID-19 drugs present higher interaction risks, such as remdesivir and Nirmatrelvir-Ritonavir, others like monoclonal antibodies appear safer. The study highlighted critical interactions such as serotonin syndrome and QTc prolongation, stressing the need for careful monitoring and flexible antidepressant use.
Cuomo et al. (2023) explored the impact of increased psychotropic medication use during the COVID-19 pandemic and the associated drug-drug interactions. They categorized these interactions and emphasized the need for vigilant monitoring and dose adjustments to ensure treatment safety and efficacy.
Awortwe and Cascorbi (2020) investigated the risks of drug interactions between COVID-19 treatments and medications for comorbidities. Their meta-analysis identified comorbidities such as cardiometabolic syndrome and chronic diseases as factors worsening clinical outcomes and highlighted interactions that could lead to severe effects. They stressed the need for careful clinical monitoring and potential dose adjustments.
Kumar and Trivedi (2020) reviewed the challenges of managing COVID-19 due to the rapid spread of the disease and the limited effectiveness of available drugs. They discussed the role of drug transporters and metabolizing enzymes and highlighted the importance of understanding drug interactions to optimize treatment safety, calling for continued research to validate the efficacy and safety of these treatments.
In conclusion, the management of COVID-19 has revealed complex challenges associated with drug interactions and polypharmacy, particularly as the pandemic has necessitated the rapid deployment of various treatments. The urgency of addressing this global health crisis led to the use of medications based on preliminary evidence, which introduced significant risks of adverse drug interactions. Studies by Hodge et al. (2020), Plasencia-García et al. (2020), Davoutis et al. (2023), Cuomo et al. (2023), Awortwe and Cascorbi (2020), and Kumar and Trivedi (2020) underscore the critical need for vigilant monitoring and evidence-based practices in managing these interactions.
The findings highlight that while some COVID-19 treatments may be safely combined, others pose considerable risks, particularly concerning cardiovascular effects and interactions with psychotropic medications. The challenges are compounded by the presence of comorbidities in many patients, further increasing the risk of adverse outcomes. To navigate these complexities, it is essential to prioritize the development of comprehensive guidelines and protocols based on robust clinical evidence. Ongoing research, continuous education for healthcare professionals, and careful monitoring are vital to optimizing treatment safety and efficacy. As new data emerges and treatment options evolve, adapting clinical practices to address these drug interactions will be crucial in improving patient outcomes and effectively managing both COVID-19 and its associated comorbidities.
References
Awortwe, C., & Cascorbi, I. (2020). Meta-analysis on outcome-worsening comorbidities of COVID-19 and related potential drug-drug interactions. Pharmacological Research, 161, 105250 – 105250. https://doi.org/10.1016/j.phrs.2020.105250.
Cuomo, A., Barillà, G., Serafini, G., Aguglia, A., Amerio, A., Cattolico, M., Carmellini, P., Spiti, A., & Fagiolini, A. (2023). Drug-drug interactions between COVID-19 therapeutics and psychotropic medications.. Expert opinion on drug metabolism & toxicology. https://doi.org/10.1080/17425255.2023.2288681.
Davoutis, E., Panou, C., Stachika, N., Dalla, C., & Kokras, N. (2023). Drug-drug interactions between COVID-19 drug therapies and antidepressants.. Expert opinion on drug metabolism & toxicology. https://doi.org/10.1080/17425255.2023.2280750.
Hodge, C., Marra, F., Marzolini, C., Boyle, A., Gibbons, S., Siccardi, M., Burger, D., Back, D., & Khoo, S. (2020). Drug interactions: a review of the unseen danger of experimental COVID-19 therapies. Journal of Antimicrobial Chemotherapy, 75, 3417 – 3424. https://doi.org/10.1093/jac/dkaa340.
Kumar, D., & Trivedi, N. (2020). Disease-drug and drug-drug interaction in COVID-19: Risk and assessment. Biomedicine & Pharmacotherapy, 139, 111642 – 111642. https://doi.org/10.1016/j.biopha.2021.111642.
Plasencia-García, B., Rodríguez-Menéndez, G., Rico-Rangel, M., Rubio-Garcia, A., Torelló-Iserte, J., & Crespo-Facorro, B. (2020). Drug-drug interactions between COVID-19 treatments and antipsychotics drugs: integrated evidence from 4 databases and a systematic review. Psychopharmacology, 238, 329 – 340. https://doi.org/10.1007/s00213-020-05716-4.
Rezaee, H., Pourkarim, F., Pourtaghi‐Anvarian, S., Entezari‐Maleki, T., Asvadi‐Kermani, T., & Nouri‐Vaskeh, M. (2021). Drug‐drug interactions with candidate medications used for COVID‐19 treatment: an overview. Pharmacology research & perspectives, 9(1), e00705. https://doi.org/10.1002/prp2.705.
