DOR CENTRAL PÓS-AVC: UMA REVISÃO DE ESCOPO
REGISTRO DOI: 10.69849/revistaft/ar10202409252058
Matheus Soares Ribeiro Guimarães1; Alan Bessa Aguiar2; Francisco Machado Junior3; Michele da Silva Melo4; Fernanda Martini de Matos Barros5; George Franco de Oliveira6; Paula Villena Teixeira Santos Silva7; Gessica Albuquerque Pedrosa Dias8; Daniel Mota Coelho9; Marissa Prudente Pinheiro Guizardi10; Júlio César Claudino dos Santos11.
Abstract
Introduction: Central post-stroke pain (CPSP) is a neuropathic pain syndrome that can affect individuals who have suffered a stroke and which is still under-recognized by doctors. CPSP has an estimated prevalence of 11% and is more common in lesions involving the thalamus. Diagnosis is challenging due to the variable clinical manifestations and the lack of specific diagnostic criteria. The study aims to gather up-to-date information on this condition and highlight the importance of its early recognition. Methodology: This is a descriptive review of the literature in Medline databases, including articles from 2014 to 2024. A total of 468 articles were initially found, of which 43 were selected after applying inclusion and exclusion criteria. Results and discussion: Risk factors were identified as involvement of the spinothalamic pathway, presence of sensory deficits, female gender, young age, and initial stroke severity. The clinical characteristics of CPSP include pain and sensory abnormalities in the regions corresponding to the injured brain territory. The differential diagnosis includes other etiologies, such as post-stroke spasticity, complex regional pain syndrome, headache and shoulder pain. CPSP has a significant impact on quality of life and is associated with psychological disorders and functional limitations. Conclusion: It is understood that early recognition and appropriate management of CPSP are essential for improving patients’ quality of life, highlighting the need for clear diagnostic criteria and effective treatments.
Keywords: Central post-stroke pain; Stroke; Pain.
Resumo
Introdução: A dor central pós-acidente vascular cerebral (CPSP) é uma síndrome de dor neuropática que pode acometer indivíduos que sofreram acidente vascular cerebral (AVC) e que continua a ser pouco reconhecida pelos médicos. A CPSP tem uma prevalência estimada de 11%, sendo mais comum em lesões que envolvem o tálamo. O diagnóstico é desafiador devido à clínica variável e à ausência de critérios diagnósticos específicos. O estudo objetiva reunir informações atualizadas sobre essa condição e destacar a importância de seu reconhecimento precoce. Metodologia: Trata-se de uma revisão descritiva da literatura nas bases de dados Medline, com inclusão de artigos de 2014 a 2024. Foram inicialmente encontrados 468 artigos, dos quais 43 foram selecionados após aplicação de critérios de inclusão e exclusão. Resultados e discussão: Identificou-se fatores de risco como acometimento da via espinotalâmica, presença de déficits sensoriais, sexo feminino, idade jovem, e gravidade inicial do AVC. As características clínicas da CPSP incluem dor e anormalidades sensoriais nas regiões correspondentes ao território cerebral lesionado. O diagnóstico diferencial abrange outras etiologias, como espasticidade pós-AVC, síndrome de dor regional complexa, cefaleia e dor no ombro. A CPSP tem impacto significativo na qualidade de vida, associando-se a distúrbios psicológicos e limitações funcionais. Conclusão: Entende-se que o reconhecimento precoce e o manejo adequado da CPSP são essenciais para melhorar a qualidade de vida dos pacientes, destacando a necessidade de critérios diagnósticos claros e de tratamentos eficazes.
Palavras-chave: Dor central pós-AVC; Acidente vascular cerebral; Dor.
1. Introduction
Although the incidence of new and recurrent strokes is decreasing, probably due to the increased use of specific preventive drugs such as statins and antihypertensives, the rates of this disease are still quite significant (Guzik et al., 2017). Risk factors such as hypertension, diabetes mellitus, smoking and hyperlipidemia, as well as obesity, inadequate diet/nutrition and physical inactivity are conditions that favor the perpetuation of a high incidence of this pathology (Furie et al., 2020; Kuklina et al., 2012). However, it is a fact that death from stroke has decreased in the last decade, becoming only the fifth leading cause of death in the United States, which indicates the need for a more orderly management of post-stroke patients in order to improve their quality of life (Guzik et al., 2017).
Among the morbidities that aggravate individuals affected by this disease, central pain after stroke (CPSP) remains a problem that is little recognized by doctors (Delpont et al., 2018; Hassaballa et al., 2020). CPSP consists of a neuropathic pain syndrome that can occur after a stroke, characterized by pain and sensory abnormalities in the parts of the body that correspond to the brain territory affected by the cerebrovascular lesion (Anosike et al., 2024; Cheng et al., 2023; Akyuz et al., 2016). The exact prevalence of this entity is not known, since patients may not describe it due to aphasia, neglect syndrome, dementia, mood disorders and other conditions that they are concomitantly affected by (Smith et al., 2013; O’Donnell et al., 2013; Lundström et al., 2009). However, a recent meta-analysis points to a prevalence of around 11% in stroke patients, and it is even more frequent among those whose thalamic region is affected, reaching more than 50% (Liampas et al., 2020).
The definitive diagnosis of central post-stroke pain is difficult, mainly due to its variable clinical nature, the existence of a wide range of other causes of pain in these patients – which will be discussed later in this article – the lack of well-established diagnostic scales and criteria and medical inexperience in recognizing it (Klit et al., 2009). It is known, however, that a combination of history, clinical examination, imaging of the lesions and exclusion of other possible causes of pain is necessary for this diagnosis (Mohanan et al., 2023). Likewise, treatment is also challenging and is often based on trial and error until the patient’s pain is relieved, which is commonly achieved with a combination of various medications (Widar et al., 2002).
According to the above information, and given the high prevalence of central post-stroke pain, this study aims to gather up-to-date information on the subject and highlight the importance of recognizing this condition in order to improve well-being and reduce secondary complications in these patients through an earlier and more appropriate approach.
2. Methodology
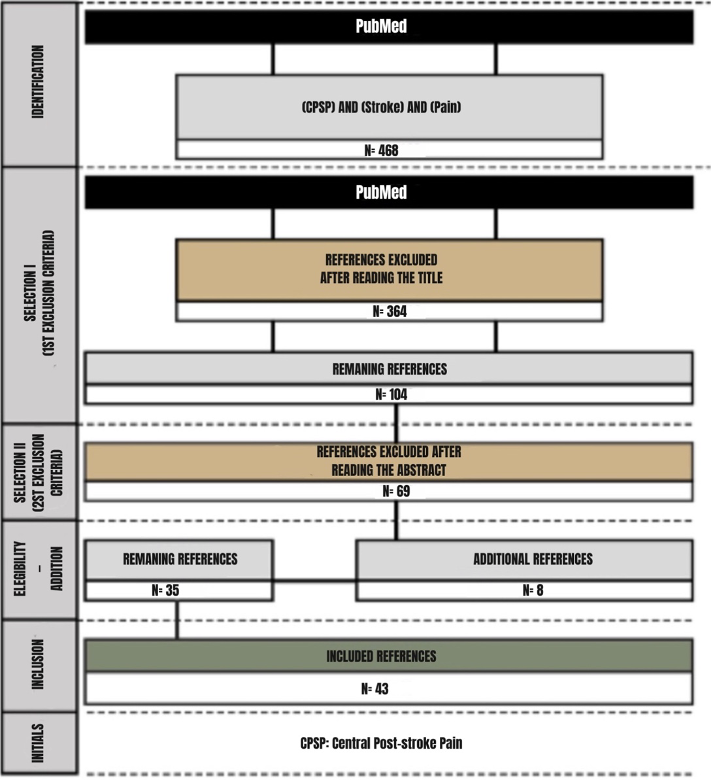
A descriptive literature review was conducted in the Medline Databases from 2014 to 2024 on central post-stroke pain. In Medline, 468 articles were found by the Mesh descriptor “(central post-stroke pain) AND (stroke) AND (pain)”, of which 104 were selected after the first set of criteria — exclusion of titles not addressing the topic “central post-stroke pain and/or stroke”, articles not included in the search period 2014-2024, as well as non- English articles. The second set of criteria — exclusion of the abstracts not addressed to central post-stroke pain, as well as articles with animal models — was applied, by which 69 articles were excluded. To ensure content saturation, the authors checked the included research references and related reviews on topics to identify missing publications. Furthermore, eight (8) articles from the Medline Database were manually screened and added according to their relevance in the qualitative evidence synthesis. Of the total, 43 original articles remained (Figure 1).
Figure 1 – Flowchart of the article selection.
3. Results and Discussion
3.1 Risk factors
There are some factors that are related to a higher risk of developing central pain in individuals who have been affected by a stroke. As for the location of the lesion, it has been found that involvement of the spinothalamic pathway and areas such as the thalamus, medulla and sensory cortex are strongly correlated with the development of CPSP (Singer et al., 2017; Vukojevic et al, 2018; Choi-Kwon et al., 2017). Furthermore, the presence of sensory deficits, such as allodynia, hyperesthesia and dysesthesia, soon after the stroke, is also an important predictor (Klit et al., 2009).
In terms of gender and age group, younger and female patients are more likely to develop this disease (Harrison et al., 2015). Finally, a greater initial severity of the stroke, measured by scales such as the NIHSS, the presence of comorbidities such as diabetes mellitus, depressive symptoms, smoking, use of statins and a higher level of previous functional incapacity are also risk factors for CPSP (O’Donnell et al., 2013; Xiong et al., 2023).
3.2 Clinical characteristics
The clinical characteristics of central post-stroke pain are similar to those of other central and peripheral neuropathic pain syndromes. There are no pathognomonic signs or characteristics, and the onset, presentation and intensity of pain can vary widely. Furthermore, the characteristics and descriptions of CPSP differ significantly from one patient to another (Li et al., 2022; Segatore et al., 1996).
CPSP is an entity that manifests itself in different ways, with pain presenting itself as throbbing, penetrating, acute and burning, and can occur with or without triggers (Anosike et al., 2024). Onset usually occurs between 1 and 6 months after the stroke, but in some cases it can take more than a year to manifest itself, which makes early diagnosis difficult (Harno et al., 2014). Symptoms can be classified into broad categories, such as allodynia to heat, allodynia to cold, spontaneous dysesthesia, evoked dysesthesia, hyperalgesia and paresthesia (Betancur et al., 2021). The distribution of pain can vary from a small area, such as the hand, to larger areas, such as the entire side of the body. The larger areas are the most frequently affected, and may or may not include the trunk and face (Klit et al., 2009).
A controlled cross-sectional study identified 39 patients with post-stroke central neuropathic pain, 79.5% of whom had pain in the upper limbs, face and lower limbs. The main symptoms observed were a burning sensation in 82.1%, tingling in 66.7%, and pain evoked by cold stimuli in 64%. In addition, hyperalgesia was responsible for 71.8% of patients with CPSP, appearing frequently. Sensory abnormalities, such as thermal and mechanical allodynia, also had a prevalence of 61.5% (Barbosa et al., 2022).
Thus, a focused history emphasizing sensory aspects, as opposed to motor or range of motion deficits, together with a comprehensive physical examination, particularly of the cranial nerves and sensory function, help to locate lesions and identify responses to pain sensation, hyperalgesia, hypoalgesia and evoked dysesthesias, differentiating CPSP from other post-stroke diseases (Harrison et al., 2015; Treister et al., 2017).
3.3 Differential diagnosis
In addition to CPSP, there are numerous other etiologies for pain in stroke patients, each with specific characteristics and mechanisms that are relevant in this context (Zakel et al., 2024; Paolucci et al., 2016). Thus, adding up all the possible causes for this symptom, there are studies that report a prevalence of up to 74% of patients (Kim et al., 2009). The most common subtypes – apart from central origin – of post-stroke pain are complex regional pain syndrome, shoulder pain, spasticity-related pain and headache (Yang et al., 2021).
Post-stroke spasticity is a common condition that presents with stiffness during flexion of the upper limbs and extension of the lower limbs, and results from increased muscle tone and exaggerated reflexes due to lesions in the corticospinal tract, leading to significant pain and functional limitations (Wissel et al., 2015; Glaess-Leistner et al., 2021). Post-stroke shoulder pain, also known as hemiplegic shoulder pain – because it is usually present on the side of the body affected by the stroke – can be generated by a number of mechanisms, such as shoulder subluxation, adhesive capsulitis, traction/compression neuropathy and other soft tissue injuries (Sun et al., 2022; Anwer et al., 2020). The prevalence can reach 72% in the first year after the stroke (Li et al., 2023).
Complex post-stroke regional pain syndrome is a chronic pain entity that can occur after peripheral or central nerve lesions. It is characterized by intense pain, edema, trophic disorders and autonomic dysfunction, as well as bone demineralization, commonly affecting one extremity and in an asymmetrical manner (Altas et al., 2020; Katsura et al., 2022; Do et al., 2022). Finally, post-stroke headache is also a complication, with a prevalence ranging from 1% to 23%. It often presents as a tension-type headache and can persist for more than three months after the initial event (Chan et al., 2023; Wee et al., 2018).
3.4 Complications
Central post-stroke pain has significant consequences and negative impacts on patients. Studies show that these individuals have a severely compromised quality of life, both physically and mentally (Aprile et al., 2015; Payton et al., 2020).
It is known that psychological disorders are commonly seen, manifesting as anxiety and depression, which can lead to self-mutilation and even suicide (Klit et al., 2009). Sleep disorders are also common (Xu et al., 2020). In addition, patients’ functionality and independence are affected. The presence of CPSP is associated with greater functional dependence and cognitive decline, which can limit patients’ ability to carry out daily activities and reduce their autonomy (Delpont et al., 2018).
The complexity of CPSP also creates challenges in terms of adherence to treatment and the rehabilitation process, leading to a worse prognosis (Aprile et al., 2015). Early identification of these psychological and behavioral manifestations by healthcare professionals is crucial to optimizing therapeutic outcomes and patient well-being (Anosike et al., 2024).
4. Conclusion
Stroke continues to be a condition with significant impacts on public health, despite falling mortality rates and the increasing use of preventive strategies. In this context, central post-stroke pain emerges as a relevant complication, often underdiagnosed and underestimated, with significant prevalence. Identifying and managing this condition is challenging due to the variability of symptoms and the overlap with other painful conditions. However, CPSP is associated with a marked negative impact on patients’ quality of life, with important psychological, functional and behavioral consequences.
Thus, it is understood that new studies specifically dedicated to consolidating clear diagnostic criteria, as well as evaluating the effectiveness of treatment for post-stroke central pain, are profoundly necessary, so that health professionals are more aware of the early recognition of this condition and enabled to manage it more appropriately, which can substantially improve the well-being of patients and reduce the associated secondary complications.
References
Akyuz, G., & Kuru, P. (2016). Systematic Review of Central Post Stroke Pain: What Is Happening in the Central Nervous System?. American journal of physical medicine & rehabilitation, 95(8), 618–627. https://doi.org/10.1097/PHM.0000000000000542
Altas, E. U., Onat, Ş. Ş., Konak, H. E., & Polat, C. S. (2020). Post-stroke complex regional pain syndrome and related factors: Experiences from a tertiary rehabilitation center. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association, 29(9), 104995. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104995
Anosike, K. C., & Rajaram Manoharan , S. V. R. (2024). Central Post-Stroke Pain Syndrome. In StatPearls. StatPearls Publishing.
Anwer, S., & Alghadir, A. (2020). Incidence, Prevalence, and Risk Factors of Hemiplegic Shoulder Pain: A Systematic Review. International journal of environmental research and public health, 17(14), 4962. https://doi.org/10.3390/ijerph17144962
Aprile, I., Briani, C., Pazzaglia, C., Cecchi, F., Negrini, S., Padua, L., & Don Carlo Gnocchi Pain-Rehab Group (2015). Pain in stroke patients: characteristics and impact on the rehabilitation treatment. A multicenter cross-sectional study. European journal of physical and rehabilitation medicine, 51(6), 725–736.
Barbosa, L. M., da Silva, V. A., de Lima Rodrigues, A. L., Mendes Fernandes, D. T. R., de Oliveira, R. A. A., Galhardoni, R., Yeng, L. T., Junior, J. R., Conforto, A. B., Lucato, L. T., Lemos, M. D., Peyron, R., Garcia-Larrea, L., Teixeira, M. J., & Ciampi de Andrade, D. (2022). Dissecting central post-stroke pain: a controlled symptom-psychophysical characterization. Brain communications, 4(3), fcac090. https://doi.org/10.1093/braincomms/fcac090
Betancur, D. F. A., Tarragó, M. D. G. L., Torres, I. L. D. S., Fregni, F., & Caumo, W. (2021). Central Post-Stroke Pain: An Integrative Review of Somatotopic Damage, Clinical Symptoms, and Neurophysiological Measures. Frontiers in neurology, 12, 678198. https://doi.org/10.3389/fneur.2021.678198
Chan, M., & Thaler, A. (2023). Post-stroke Headache. Current pain and headache reports, 27(11), 673–678. https://doi.org/10.1007/s11916-023-01169-4
Cheng, Y., Wu, B., Huang, J., & Chen, Y. (2023). Research Progress on the Mechanisms of Central Post-Stroke Pain: A Review. Cellular and molecular neurobiology, 43(7), 3083–3098. https://doi.org/10.1007/s10571-023-01360-6
Choi-Kwon, S., Choi, S. H., Suh, M., Choi, S., Cho, K. H., Nah, H. W., Song, H., & Kim, J. S. (2017). Musculoskeletal and central pain at 1 year post-stroke: associated factors and impact on quality of life. Acta neurologica Scandinavica, 135(4), 419–425. https://doi.org/10.1111/ane.12617
Delpont, B., Blanc, C., Osseby, G. V., Hervieu-Bègue, M., Giroud, M., & Béjot, Y. (2018). Pain after stroke: A review. Revue neurologique, 174(10), 671–674. https://doi.org/10.1016/j.neurol.2017.11.011
Do, J. G., Choi, J. H., Park, C. H., Yoon, K. J., & Lee, Y. T. (2022). Prevalence and Related Factors for Poststroke Complex Regional Pain Syndrome: A Retrospective Cross-Sectional Cohort Study. Archives of physical medicine and rehabilitation, 103(2), 274–281. https://doi.org/10.1016/j.apmr.2021.08.003
Furie K. (2020). Epidemiology and Primary Prevention of Stroke. Continuum (Minneapolis, Minn.), 26(2), 260–267. https://doi.org/10.1212/CON.0000000000000831
Glaess-Leistner, S., Ri, S. J., Audebert, H. J., & Wissel, J. (2021). Early clinical predictors of post stroke spasticity. Topics in stroke rehabilitation, 28(7), 508–518. https://doi.org/10.1080/10749357.2020.1843845
Guzik, A., & Bushnell, C. (2017). Stroke Epidemiology and Risk Factor Management. Continuum (Minneapolis, Minn.), 23(1, Cerebrovascular Disease), 15–39. https://doi.org/10.1212/CON.0000000000000416
Harno, H., Haapaniemi, E., Putaala, J., Haanpää, M., Mäkelä, J. P., Kalso, E., & Tatlisumak, T. (2014). Central poststroke pain in young ischemic stroke survivors in the Helsinki Young Stroke Registry. Neurology, 83(13), 1147–1154. https://doi.org/10.1212/WNL.0000000000000818
Harrison, R. A., & Field, T. S. (2015). Post stroke pain: identification, assessment, and therapy. Cerebrovascular diseases (Basel, Switzerland), 39(3-4), 190–201. https://doi.org/10.1159/000375397
Hassaballa, D., & Harvey, R. L. (2020). Central pain syndromes. NeuroRehabilitation, 47(3), 285–297. https://doi.org/10.3233/NRE-208003
Katsura, Y., Ohga, S., Shimo, K., Hattori, T., Yamada, T., & Matsubara, T. (2022). Post-Stroke Complex Regional Pain Syndrome and Upper Limb Inactivity in Hemiplegic Patients: A Cross-Sectional Study. Journal of pain research, 15, 3255–3262. https://doi.org/10.2147/JPR.S379840
Kim J. S. (2009). Post-stroke pain. Expert review of neurotherapeutics, 9(5), 711–721. https://doi.org/10.1586/ern.09.19
Klit, H., Finnerup, N. B., & Jensen, T. S. (2009). Central post-stroke pain: clinical characteristics, pathophysiology, and management. The Lancet. Neurology, 8(9), 857–868. https://doi.org/10.1016/S1474-4422(09)70176-0
Kuklina, E. V., Tong, X., George, M. G., & Bansil, P. (2012). Epidemiology and prevention of stroke: a worldwide perspective. Expert review of neurotherapeutics, 12(2), 199–208. https://doi.org/10.1586/ern.11.99
Li, C., Shu, X., & Liu, X. (2022). Research Hotspots and Frontiers in Post Stroke Pain: A Bibliometric Analysis Study. Frontiers in molecular neuroscience, 15, 905679. https://doi.org/10.3389/fnmol.2022.905679
Li, Y., Yang, S., Cui, L., Bao, Y., Gu, L., Pan, H., Wang, J., & Xie, Q. (2023). Prevalence, risk factor and outcome in middle-aged and elderly population affected by hemiplegic shoulder pain: An observational study. Frontiers in neurology, 13, 1041263. https://doi.org/10.3389/fneur.2022.1041263
Liampas, A., Velidakis, N., Georgiou, T., Vadalouca, A., Varrassi, G., Hadjigeorgiou, G. M., Tsivgoulis, G., & Zis, P. (2020). Prevalence and Management Challenges in Central Post-Stroke Neuropathic Pain: A Systematic Review and Meta-analysis. Advances in therapy, 37(7), 3278–3291. https://doi.org/10.1007/s12325-020-01388-w
Lundström, E., Smits, A., Terént, A., & Borg, J. (2009). Risk factors for stroke-related pain 1 year after first-ever stroke. European journal of neurology, 16(2), 188–193. https://doi.org/10.1111/j.1468-1331.2008.02378.x
Mohanan, A. T., Nithya, S., Nomier, Y., Hassan, D. A., Jali, A. M., Qadri, M., & Machanchery, S. (2023). Stroke-Induced Central Pain: Overview of the Mechanisms, Management, and Emerging Targets of Central Post-Stroke Pain. Pharmaceuticals (Basel, Switzerland), 16(8), 1103. https://doi.org/10.3390/ph16081103
O’Donnell, M. J., Diener, H. C., Sacco, R. L., Panju, A. A., Vinisko, R., Yusuf, S., & PRoFESS Investigators (2013). Chronic pain syndromes after ischemic stroke: PRoFESS trial. Stroke, 44(5), 1238–1243. https://doi.org/10.1161/STROKEAHA.111.671008
Paolucci, S., Iosa, M., Toni, D., Barbanti, P., Bovi, P., Cavallini, A., Candeloro, E., Mancini, A., Mancuso, M., Monaco, S., Pieroni, A., Recchia, S., Sessa, M., Strambo, D., Tinazzi, M., Cruccu, G., Truini, A., & Neuropathic pain special interest group of the Italian Neurological Society (2016). Prevalence and Time Course of Post-Stroke Pain: A Multicenter Prospective Hospital-Based Study. Pain medicine (Malden, Mass.), 17(5), 924–930. https://doi.org/10.1093/pm/pnv019
Payton, H., & Soundy, A. (2020). The Experience of Post-Stroke Pain and The Impact on Quality of Life: An Integrative Review. Behavioral sciences (Basel, Switzerland), 10(8), 128. https://doi.org/10.3390/bs10080128
Segatore M. (1996). Understanding central post-stroke pain. The Journal of neuroscience nursing : journal of the American Association of Neuroscience Nurses, 28(1), 28–35. https://doi.org/10.1097/01376517-199602000-00006
Singer, J., Conigliaro, A., Spina, E., Law, S. W., & Levine, S. R. (2017). Central poststroke pain: A systematic review. International journal of stroke : official journal of the International Stroke Society, 12(4), 343–355. https://doi.org/10.1177/1747493017701149
Smith, J. H., Bottemiller, K. L., Flemming, K. D., Michael Cutrer, F., & Strand, E. A. (2013). Inability to self-report pain after a stroke: a population-based study. Pain, 154(8), 1281–1286. https://doi.org/10.1016/j.pain.2013.04.006
Sun, W., Ji, G., Lu, L., Sun, J., Guo, H., Yao, Y., Gao, S., Li, J., Chen, J., & Song, B. (2022). Tuina for shoulder pain after stroke: A protocol for systematic review and meta-analysis. Medicine, 101(46), e31828. https://doi.org/10.1097/MD.0000000000031828
Treister, A. K., Hatch, M. N., Cramer, S. C., & Chang, E. Y. (2017). Demystifying Poststroke Pain: From Etiology to Treatment. PM & R : the journal of injury, function, and rehabilitation, 9(1), 63–75. https://doi.org/10.1016/j.pmrj.2016.05.015
Vukojevic, Z., Dominovic Kovacevic, A., Peric, S., Grgic, S., Bjelica, B., Basta, I., & Lavrnic, D. (2018). Frequency and features of the central poststroke pain. Journal of the neurological sciences, 391, 100–103. https://doi.org/10.1016/j.jns.2018.06.004
Wee T. C. (2018). Poststroke Headache: An Underdiagnosed Entity?. American journal of physical medicine & rehabilitation, 97(6), e56–e57. https://doi.org/10.1097/PHM.0000000000000835
Widar, M., Samuelsson, L., Karlsson-Tivenius, S., & Ahlström, G. (2002). Long-term pain conditions after a stroke. Journal of rehabilitation medicine, 34(4), 165–170. https://doi.org/10.1080/16501970213237
Wissel, J., Verrier, M., Simpson, D. M., Charles, D., Guinto, P., Papapetropoulos, S., & Sunnerhagen, K. S. (2015). Post-stroke spasticity: predictors of early development and considerations for therapeutic intervention. PM & R : the journal of injury, function, and rehabilitation, 7(1), 60–67. https://doi.org/10.1016/j.pmrj.2014.08.946
Xiong, F., Shen, P., Li, Z., Huang, Z., Liang, Y., Chen, X., Li, Y., Chai, X., Feng, Z., & Li, M. (2023). Bibliometric Analysis of Post-Stroke Pain Research Published from 2012 to 2021. Journal of pain research, 16, 1–20. https://doi.org/10.2147/JPR.S375063
Xu, X. M., Luo, H., Rong, B. B., Zheng, X. M., Wang, F. T., Zhang, S. J., & Li, Z. X. (2020). Nonpharmacological therapies for central poststroke pain: A systematic review. Medicine, 99(42), e22611. https://doi.org/10.1097/MD.0000000000022611
Yang, S., & Chang, M. C. (2021). Poststroke Pain. Seminars in neurology, 41(1), 67–74. https://doi.org/10.1055/s-0040-1722641
Zakel, J., Chae, J., & Wilson, R. D. (2024). Innovations in Stroke Recovery and Rehabilitation: Poststroke Pain. Physical medicine and rehabilitation clinics of North America, 35(2), 445–462. https://doi.org/10.1016/j.pmr.2023.06.027
1University Center Christus, Brazil
E-mail: matheussrg1@gmail.com
https://orcid.org/0009-0008-4089-843X
2University Center Christus, Brazil
E-mail: alanaguiarr123@gmail.com
https://orcid.org/0000-0002-0679-0133
3University Center Christus, Brazil
Email: machadojr1702@gmail.com
https://orcid.org/0009-0007-7058-694X
4University Center Christus, Brazil
E-mail: michelemelo.med@gmail.com
https://orcid.org/0009-0001-7824-2689
5University Center Christus, Brazil
E-mail: fernandamartinib@gmail.com
https://orcid.org/0000-0003-4730-3423
6University Center Christus, Brazil
E-mail: georgegfo22@gmail.com
https://orcid.org/0009-0000-1871-7948
7University Center Christus, Brazil
E-mail: paulavillena09@gmail.com
https://orcid.org/0009-0006-5517-0025
8Paraíso College, Brazil
Email: gessica.apd@gmail.com
9University Center Christus, Brazil
Email: danielmama1980@gmail.com
https://orcid.org/0009-0002-3807-8885
10University Center Christus, Brazil
E-mail: marissaprudente.med@gmail.com
11University Center Christus, Brazil
E-mail: cesar.claudino@unifesp.br
https://orcid.org/0000-0001-6543-481X
