REGISTRO DOI: 10.69849/revistaft/cs10202505130349
Alexandre Cesar Biriba Filho
Abstract
Antibiotic prophylaxis in oral surgery has become a standard practice aimed at preventing postoperative infections, which can lead to complications such as wound infections, dry socket, or more severe systemic issues. The primary purpose of prophylactic antibiotic use is to reduce the risk of bacterial contamination at surgical sites, especially in procedures that involve bone, soft tissues, or the mucosal membrane. This article reviews the current guidelines, the efficacy of commonly prescribed antibiotics, and the potential risks associated with antibiotic overuse in oral surgery.
While numerous studies support the benefits of antibiotic prophylaxis in preventing infection after certain surgical procedures, the decision to use antibiotics should be based on specific clinical factors, including the type of surgery, the patient’s overall health, and the presence of risk factors such as immunocompromised conditions or the presence of chronic diseases like diabetes. The most commonly prescribed antibiotics in oral surgery include amoxicillin, clindamycin, and metronidazole, each of which targets a broad spectrum of bacteria typically found in the oral cavity. However, the widespread and sometimes unnecessary use of antibiotics has raised concerns about the emergence of antibiotic-resistant bacteria, which poses a significant threat to public health.
This article further explores the balance between effective prophylaxis and the risks of antibiotic resistance, presenting a comprehensive review of the existing literature and offering recommendations for future research. The role of individualized therapy, based on patient characteristics and procedure type, is also discussed to ensure optimal outcomes and reduce unnecessary antibiotic use in oral surgery.
Keywords: Antibiotic prophylaxis, Oral surgery, Postoperative infection, Antibiotic resistance, Surgical guidelines.
Antibiotic prophylaxis has become a cornerstone in modern oral surgery, aiming to prevent postoperative infections, which can lead to significant complications, including wound infections, dry socket, abscess formation, osteomyelitis, or even life-threatening systemic infections. The primary goal of prophylactic antibiotic use is to reduce the risk of bacterial contamination at the surgical site, particularly during procedures that involve bone, soft tissues, or mucosal membranes. Infections following oral surgical procedures are common, and these infections can complicate recovery, increase treatment costs, and pose risks to patients’ overall health. As a result, the use of antibiotics before, during, and sometimes after surgery has become a standard practice in many oral surgical procedures.
Oral surgery encompasses a wide range of procedures, from simple tooth extractions to more complex surgeries such as dental implants, periodontal surgeries, and corrective jaw surgeries. Each of these procedures involves varying degrees of tissue manipulation, and certain high-risk surgeries, such as wisdom tooth extractions, carry an increased likelihood of infection. The oral cavity is home to a rich and diverse microbiota composed of a variety of microorganisms, many of which can contribute to postoperative infections if they gain access to deeper tissues during surgery. Common bacteria found in the oral flora include Streptococcus species, Staphylococcus aureus, Prevotella species, Fusobacterium species, and Enterococcus, all of which are capable of causing infections when introduced into surgical wounds.
The evolution of antibiotic prophylaxis in oral surgery has been influenced by advances in microbiology and clinical practice. Initially, prophylactic antibiotics were used indiscriminately in an attempt to prevent infections in all patients undergoing oral surgery. However, as research progressed, the need for more tailored approaches became apparent. The development of guidelines and protocols for antibiotic use in oral surgery has allowed for more precise indications, reducing unnecessary antibiotic administration while still providing adequate protection for high-risk procedures and patients with specific underlying conditions.
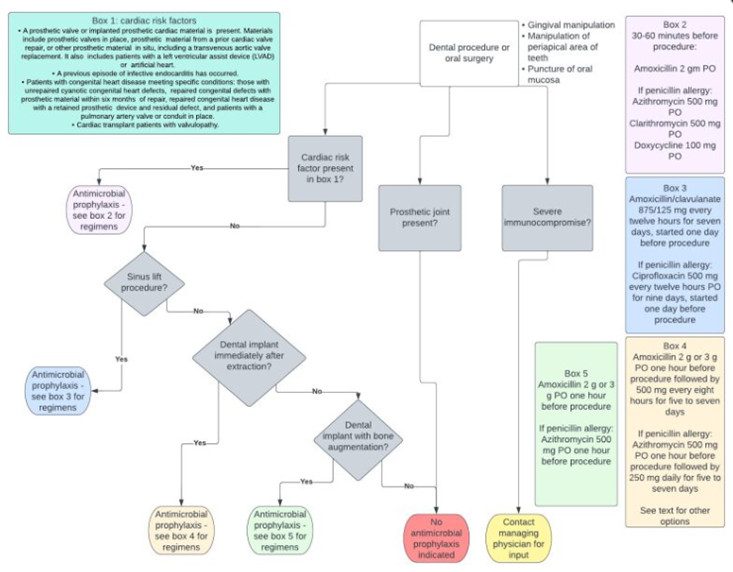
Source: StatPearls Publishing, via the National Center for Biotechnology Information (NCBI, 2023.
This flowchart provides a clear visual representation of the decision-making process for prescribing antibiotic prophylaxis in dental and oral surgery. It considers factors such as the type of procedure, patient-specific risk factors (e.g., cardiac conditions), and current clinical guidelines.
The efficacy of antibiotic prophylaxis in preventing postoperative infections is well-documented in the literature. Studies have shown that prophylactic antibiotics significantly reduce the incidence of infections in certain high-risk procedures, such as impacted wisdom tooth extractions and implant surgeries. However, the decision to use antibiotics must be carefully considered, as inappropriate or excessive use can lead to serious consequences. The rise of antibiotic-resistant bacteria, driven by the overuse and misuse of antibiotics, has become a major public health concern. Resistance to common antibiotics, such as amoxicillin and clindamycin, can complicate treatment and result in more difficult-to-treat infections. This is particularly concerning in the context of oral surgery, where the risk of infection is ever-present, and the need for effective antibiotics is crucial.
While antibiotic prophylaxis remains a vital tool in oral surgery, its use is not without controversy. Overuse of antibiotics, particularly for low-risk procedures or in patients with minimal risk factors, can contribute to the growing issue of antimicrobial resistance. Furthermore, certain patient populations, such as those with allergies to antibiotics or those with specific comorbidities, may require alternative approaches. For instance, patients with a history of anaphylaxis to penicillin may need to receive clindamycin as a substitute, requiring careful consideration by the oral surgeon.
The choice of antibiotic, the timing of administration, and the duration of prophylaxis are critical factors in ensuring the effectiveness of the treatment while minimizing the risk of side effects and resistance. Standard protocols suggest administering prophylactic antibiotics within one hour of the surgical incision to ensure adequate tissue concentrations during the procedure. However, the optimal duration and selection of antibiotics depend on the patient’s specific condition and the nature of the surgical procedure.
The aim of this article is to review current antibiotic prophylaxis protocols in oral surgery, analyze the effectiveness of commonly prescribed antibiotics, and discuss the risks associated with the overuse of antibiotics. It will also explore the latest evidence on the development of antibiotic resistance in oral pathogens and provide recommendations for improving antibiotic stewardship in the field of oral surgery. By reviewing current practices and guidelines, this article seeks to provide a comprehensive understanding of the role of antibiotic prophylaxis in oral surgery, offering insight into how future clinical practices can evolve to balance the benefits of infection prevention with the growing concern of antibiotic resistance.
In a systematic review by Milic et al. (2020), the authors aimed to evaluate the use of prophylactic antibiotics in oral and maxillofacial surgery. Their analysis recommended the use of prophylactic antibiotics in specific procedures, such as surgical extractions of third molars, comminuted mandibular fractures, temporomandibular joint replacements, clean-contaminated tumor removals, and complex implant surgeries. However, they concluded that prophylactic antibiotics are not routinely recommended for fractures of the upper or midface facial thirds, emphasizing the need for case-by-case assessment.
Lodi et al. (2012) conducted a Cochrane systematic review to assess the effectiveness of antibiotics in preventing complications following tooth extractions. The study found that antibiotics may reduce the risk of postoperative infections and dry socket after the removal of wisdom teeth. However, the evidence was of low certainty, and the authors noted that antibiotics might cause more (generally brief and minor) unwanted effects. They concluded that while antibiotics can be beneficial in certain cases, their routine use should be carefully considered.
Hollingshead and Brizuela (2023) explored the rationale for antimicrobial prophylaxis in dental and oral surgery. They highlighted that antimicrobial prophylaxis is given in certain situations before dental and oral surgery to avoid infective endocarditis. The authors emphasized the importance of targeting prophylaxis toward the most vulnerable patients to prevent adverse events and contribute to antimicrobial stewardship.
The American Dental Association (ADA) provides guidelines on antibiotic prophylaxis prior to dental procedures. Their recommendations state that for patients with an indication for antibiotic prophylaxis, the antibiotic should be given before the procedure to ensure adequate blood levels. They also note that if the dosage is inadvertently not administered before the procedure, it may be administered up to two hours after the procedure. The ADA emphasizes the importance of appropriate antibiotic prescribing in accordance with evidence-based guidelines.
In a recent article, the ADA discussed antibiotic stewardship, highlighting that antibiotic prophylaxis prior to dental procedures should be reserved for patients at high risk of post-treatment complications. They stress the importance of prescribing antibiotics only when needed and selecting the right antibiotic at the right dose and duration. This approach aims to minimize the risk of antimicrobial resistance and ensure patient safety.
A systematic review by Alsharif et al. (2017) focused on systemic antibiotic prophylaxis for preventing infectious complications in maxillofacial trauma surgery. The study concluded that while antibiotics might reduce the risk of postoperative infections, the evidence was of low quality, and the benefits should be weighed against potential adverse effects and the risk of developing antibiotic resistance.
The American Academy of Pediatric Dentistry (AAPD) recognizes that numerous medical conditions predispose patients to bacteremia-induced infections. They recommend prophylactic antibiotics when patients with a high risk of adverse outcomes from bacteremia and infection undergo invasive oral or dental procedures. These guidelines aim to protect vulnerable patient populations while minimizing unnecessary antibiotic use.
In summary, the literature underscores the importance of judicious antibiotic use in oral surgery. While prophylactic antibiotics can be beneficial in specific high-risk scenarios, their routine use in all patients is not supported by current evidence. Adherence to established guidelines and consideration of individual patient risk factors are essential to optimize outcomes and mitigate the development of antibiotic resistance.
The reviewed studies demonstrate a nuanced consensus regarding the use of antibiotic prophylaxis in oral surgery. While the use of prophylactic antibiotics can reduce the incidence of postoperative infections in high-risk surgical cases—such as impacted third molar extractions, extensive bone manipulation, and procedures in immunocompromised individuals—routine use in healthy patients undergoing simple extractions or minor surgery is largely discouraged. Findings from Cochrane reviews and other systematic analyses indicate that antibiotics confer only a modest benefit in infection prevention in routine procedures but may contribute significantly to antibiotic resistance and adverse drug events.
Moreover, the studies show variability in recommended antibiotic regimens and timing, which reflects a lack of standardization in clinical practice. However, across the literature, the importance of adhering to evidence-based guidelines and patient-specific risk stratification remains clear. It is evident that clinical decision-making should be guided by individual risk factors, the complexity of the procedure, and principles of antibiotic stewardship to mitigate the risk of resistance.
Antibiotic prophylaxis in oral surgery continues to be a subject of clinical significance, demanding a balanced approach between infection prevention and the global responsibility to combat antibiotic resistance. The body of evidence reviewed supports a selective, risk-based strategy for prescribing antibiotics rather than a routine or universal approach.
High-quality studies such as those by Alsharif et al. (2017), Lodi et al. (2012), and Milic et al. (2020) emphasize that antibiotics can be effective in reducing postoperative infections primarily in complex oral and maxillofacial surgeries or in patients with systemic vulnerabilities. However, for healthy individuals undergoing minor procedures, the risk-benefit ratio often does not justify prophylactic use. Inappropriate or excessive prescribing can lead to unnecessary exposure to adverse drug reactions, contribute to the development of resistant microbial strains, and diminish the long-term effectiveness of antibiotics.
Professional organizations like the American Dental Association and American Academy of Pediatric Dentistry echo these findings and have issued guidelines that support targeted prophylaxis based on clinical risk assessment. These guidelines recommend specific protocols for patients with conditions such as prosthetic heart valves, prior infective endocarditis, or compromised immune systems.
In summary, antibiotic prophylaxis in oral surgery should not follow a one-size-fits-all model. Instead, clinicians must incorporate current scientific evidence, individual patient risk factors, procedural complexity, and antimicrobial stewardship principles into their decision-making process. By doing so, dental professionals can optimize patient outcomes, prevent complications, and contribute responsibly to the global effort against antimicrobial resistance.
References
Alsharif, M. H., Halboub, E., Ghanem, A., Al‐Moraissi, E. A., & Al‐Harbi, F. A. (2017). Systemic antibiotic prophylaxis for prevention of postoperative infectious complications in maxillofacial trauma surgery. Cochrane Database of Systematic Reviews, (11), CD012603. https://doi.org/10.1002/14651858.CD012603.pub2
American Academy of Pediatric Dentistry. (2020). Guideline on antibiotic prophylaxis for dental patients at risk for infection. Retrieved from https://www.aapd.org/globalassets/media/policies_guidelines/bp_antibioticprophylaxis.pdf
American Dental Association. (n.d.). Antibiotic prophylaxis prior to dental procedures. Retrieved from https://www.ada.org/resources/ada-library/oral-health-topics/antibiotic-prophylaxis
American Dental Association. (n.d.). Antibiotic stewardship. Retrieved from https://www.ada.org/resources/ada-library/oral-health-topics/antibiotic-stewardship
Hollingshead, S., & Brizuela, B. (2023). Antimicrobial Prophylaxis In Dental And Oral Surgery. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK587360/
Lodi, G., Figini, L., Sardella, A., Carrassi, A., Del Fabbro, M., & Furness, S. (2012). Antibiotics to prevent complications following tooth extractions. Cochrane Database of Systematic Reviews, (11), CD003811. https://doi.org/10.1002/14651858.CD003811.pub3
Milic, J. V., Milic, N. V., Jovicic, N., Milosevic, B., & Milosevic, D. (2020). Antibiotic prophylaxis in oral and maxillofacial surgery: A systematic review. Medicinski Pregled, 73(9–10), 287–293. https://pubmed.ncbi.nlm.nih.gov/34016464/
Silva, J. F. (2024). SENSORY-FOCUSED FOOTWEAR DESIGN: MERGING ART AND WELL-BEING FOR INDIVIDUALS WITH AUTISM. International Seven Journal of Multidisciplinary, 1(1). https://doi.org/10.56238/isevmjv1n1-016
Silva, J. F. (2024). SENSORY-FOCUSED FOOTWEAR DESIGN: MERGING ART AND WELL-BEING FOR INDIVIDUALS WITH AUTISM. International Seven Journal of Multidisciplinary, 1(1). https://doi.org/10.56238/isevmjv1n1-016
Silva, J. F. (2024). Enhancing cybersecurity: A comprehensive approach to addressing the growing threat of cybercrime. Revista Sistemática, 14(5), 1199–1203. https://doi.org/10.56238/rcsv14n5-009
Venturini, R. E. (2025). Technological innovations in agriculture: the application of Blockchain and Artificial Intelligence for grain traceability and protection. Brazilian Journal of Development, 11(3), e78100. https://doi.org/10.34117/bjdv11n3-007
Turatti, R. C. (2025). Application of artificial intelligence in forecasting consumer behavior and trends in E-commerce. Brazilian Journal of Development, 11(3), e78442. https://doi.org/10.34117/bjdv11n3-039
Garcia, A. G. (2025). The impact of sustainable practices on employee well-being and organizational success. Brazilian Journal of Development, 11(3), e78599. https://doi.org/10.34117/bjdv11n3-054
Filho, W. L. R. (2025). The Role of Zero Trust Architecture in Modern Cybersecurity: Integration with IAM and Emerging Technologies. Brazilian Journal of Development, 11(1), e76836. https://doi.org/10.34117/bjdv11n1-060
Antonio, S. L. (2025). Technological innovations and geomechanical challenges in Midland Basin Drilling. Brazilian Journal of Development, 11(3), e78097. https://doi.org/10.34117/bjdv11n3-005
Moreira, C. A. (2025). Digital monitoring of heavy equipment: advancing cost optimization and operational efficiency. Brazilian Journal of Development, 11(2), e77294. https://doi.org/10.34117/bjdv11n2-011
Delci, C. A. M. (2025). THE EFFECTIVENESS OF LAST PLANNER SYSTEM (LPS) IN INFRASTRUCTURE PROJECT MANAGEMENT. Revista Sistemática, 15(2), 133–139. https://doi.org/10.56238/rcsv15n2-009
SANTOS,Hugo;PESSOA,EliomarGotardi.Impactsofdigitalizationontheefficiencyandqualityofpublicservices:Acomprehensiveanalysis.LUMENETVIRTUS,[S.l.],v.15,n.40,p.44094414,2024.DOI:10.56238/levv15n40024.Disponívelem:https://periodicos.newsciencepubl.com/LEV/article/view/452.Acessoem:25jan.2025.
Freitas,G.B.,Rabelo,E.M.,&Pessoa,E.G.(2023).Projetomodularcomreaproveitamentodecontainermaritimo.BrazilianJournalofDevelopment,9(10),28303–28339.https://doi.org/10.34117/bjdv9n10057
Freitas,G.B.,Rabelo,E.M.,&Pessoa,E.G.(2023).Projetomodularcomreaproveitamentodecontainermaritimo.BrazilianJournalofDevelopment,9(10),28303–28339.https://doi.org/10.34117/bjdv9n10057
Pessoa,E.G.,Feitosa,L.M.,ePadua,V.P.,&Pereira,A.G.(2023).EstudodosrecalquesprimáriosemumaterroexecutadosobreaargilamoledoSarapuí.BrazilianJournalofDevelopment,9(10),28352–28375.https://doi.org/10.34117/bjdv9n10059
PESSOA,E.G.;FEITOSA,L.M.;PEREIRA,A.G.;EPADUA,V.P.Efeitosdeespéciesdealnaeficiênciadecoagulação,Alresidualepropriedadedosflocosnotratamentodeáguassuperficiais.BrazilianJournalofHealthReview,[S.l.],v.6,n.5,p.2481424826,2023.DOI:10.34119/bjhrv6n5523.Disponívelem:https://ojs.brazilianjournals.com.br/ojs/index.php/BJHR/article/view/63890.Acessoem:25jan.2025.
SANTOS,Hugo;PESSOA,EliomarGotardi.Impactsofdigitalizationontheefficiencyandqualityofpublicservices:Acomprehensiveanalysis.LUMENETVIRTUS,[S.l.],v.15,n.40,p.44094414,2024.DOI:10.56238/levv15n40024.Disponívelem:https://periodicos.newsciencepubl.com/LEV/article/view/452.Acessoem:25jan.2025.
Filho, W. L. R. (2025). The Role of Zero Trust Architecture in Modern Cybersecurity: Integration with IAM and Emerging Technologies. Brazilian Journal of Development, 11(1), e76836. https://doi.org/10.34117/bjdv11n1-060
Oliveira, C. E. C. de. (2025). Gentrification, urban revitalization, and social equity: challenges and solutions. Brazilian Journal of Development, 11(2), e77293. https://doi.org/10.34117/bjdv11n2-010
Pessoa, E. G. (2024). Pavimentos permeáveis uma solução sustentável. Revista Sistemática, 14(3), 594–599. https://doi.org/10.56238/rcsv14n3-012
Filho, W. L. R. (2025). THE ROLE OF AI IN ENHANCING IDENTITY AND ACCESS MANAGEMENT SYSTEMS. International Seven Journal of Multidisciplinary, 1(2). https://doi.org/10.56238/isevmjv1n2-011
Antonio, S. L. (2025). Technological innovations and geomechanical challenges in Midland Basin Drilling. Brazilian Journal of Development, 11(3), e78097. https://doi.org/10.34117/bjdv11n3-005
Pessoa, E. G. (2024). Pavimentos permeáveis uma solução sustentável. Revista Sistemática, 14(3), 594–599. https://doi.org/10.56238/rcsv14n3-012
Pessoa, E. G. (2024). Pavimentos permeáveis uma solução sustentável. Revista Sistemática, 14(3), 594–599. https://doi.org/10.56238/rcsv14n3-012
Eliomar Gotardi Pessoa, & Coautora: Glaucia Brandão Freitas. (2022). ANÁLISE DE CUSTO DE PAVIMENTOS PERMEÁVEIS EM BLOCO DE CONCRETO UTILIZANDO BIM (BUILDING INFORMATION MODELING). Revistaft, 26(111), 86. https://doi.org/10.5281/zenodo.10022486
Eliomar Gotardi Pessoa, Gabriel Seixas Pinto Azevedo Benittez, Nathalia Pizzol de Oliveira, & Vitor Borges Ferreira Leite. (2022). ANÁLISE COMPARATIVA ENTRE RESULTADOS EXPERIMENTAIS E TEÓRICOS DE UMA ESTACA COM CARGA HORIZONTAL APLICADA NO TOPO. Revistaft, 27(119), 67. https://doi.org/10.5281/zenodo.7626667
Eliomar Gotardi Pessoa, & Coautora: Glaucia Brandão Freitas. (2022). ANÁLISE COMPARATIVA ENTRE RESULTADOS TEÓRICOS DA DEFLEXÃO DE UMA LAJE PLANA COM CARGA DISTRIBUÍDA PELO MÉTODO DE EQUAÇÃO DE DIFERENCIAL DE LAGRANGE POR SÉRIE DE FOURIER DUPLA E MODELAGEM NUMÉRICA PELO SOFTWARE SAP2000. Revistaft, 26(111), 43. https://doi.org/10.5281/zenodo.10019943
