REGISTRO DOI: 10.69849/revistaft/th102412092305
Clara Madureira Siqueira Rodrigues
Gabriela Heringer Almeida
Barbara Eugenio Valentina Scarton
Amanda Martinez Alves Celia Regina Trindade
Carlos Pimentel Moschen Coridon Franco
Antônio Chambô Filho
ABSTRACT
The copper intrauterine device (IUD) in ectopic position during pregnancy is a rare but clinically significant condition. This situation occurs when the IUD, initially inserted into the uterus to prevent pregnancy, is found outside the uterine cavity during gestation.
This study aims to describe a case of a pregnant woman with an ectopic intrauterine device in an intravesical location, reporting the case evolution and addressing possible complications, side effects of treatment, associated risks, and the response to the interventions performed during prenatal follow-up.
This is a case report with a descriptive design, characterized by a narrative and reflective approach. The analyzed case refers to a patient treated at the fetal medicine outpatient clinic of Santa Casa de Misericórdia de Vitória – Pró-Matre Unit. The investigation was based on the reading and interpretation of data from the electronic medical record and exams performed throughout the clinical course. The evaluation included case conceptualization, medical history, diagnosis, evolution, and medical management. This study was submitted for approval by the Ethics Committee in Research with Human Beings of EMESCAM and was initiated with the participant’s consent.
It is expected to highlight the effectiveness of the multidisciplinary approaches adopted since the initial management of the patient, specifically the removal of the intrauterine device and the follow-up of the pregnancy after removal, as well as the safety of the interventions performed, based on the reported case, aiming for favorable outcomes in similar situations.
Keywords: Intrauterine device; Ectopic; Pregnancy.
INTRODUCTION
The copper intrauterine device (IUD) is a widely used long-acting reversible contraceptive method. It consists of a small device inserted into the uterus that releases copper ions, which have spermicidal properties and affect sperm motility (BLACK et al., 2016). A consultation with a healthcare professional is essential to determine the suitability of the copper IUD for each patient, as well as the need for post-insertion monitoring to assess possible displacements and complications.
Despite its safety and effectiveness, some users may experience side effects such as increased menstrual flow and dysmenorrhea, along with other more significant complications (BLACK et al., 2016). Ectopic IUD is a rare condition where the device, originally inserted into the uterus, is found outside the uterine cavity (MONA et al., 2020 and GUANGTAO et al., 2021). Since this results in a loss of contraceptive effectiveness, it can lead to pregnancy and complications such as miscarriage, preterm rupture of membranes, and chorioamnionitis.
This study aims to describe the case of a patient followed at the Obstetrics Service of Santa Casa de Misericórdia de Vitória, who presented with a copper IUD in intravesical location and a concomitant viable intrauterine pregnancy.
CASE REPORT
The case in question involves a 27-year-old patient, L.P.C., G2P1A0, with the last delivery 17 months ago, and no other comorbidities. This study was approved through the Ethics Committee Research Opinion No. 6.975.230.
The patient reports that the IUD was inserted by a physician at the Basic Health Unit closest to her home, three months after her first delivery. She also mentions having undergone an ultrasound after insertion, which showed the IUD in a normal position, although she lost the exam results.
L.P.C. was admitted to the Emergency Department of the Pró Matre Maternity on October 17, 2023, with a gestational age of 7 weeks and 5 days according to an ultrasound performed on the same day. The ultrasound described a single viable embryo, with fetal heartbeats of 158 bpm, and a fetal biometry consistent with 7 weeks and 5 days. Additionally, a hyperechoic image suggestive of an IUD was seen, located in the pelvic cavity, adjacent to the anterior external uterine wall, indicating a displaced IUD. At the time of consultation, the patient was asymptomatic. A speculum examination revealed the IUD thread exteriorizing through the external cervical os. The patient was referred for high-risk prenatal follow-up at the Pró Matre service.
Several ultrasounds were performed to evaluate fetal viability and the exact position of the IUD to plan further management. The first ultrasound conducted at the service revealed a viable gestational sac, an embryo with 138 bpm, a fetal biometry corresponding to 9 weeks and 4 days, and a posterior placenta. An image consistent with an IUD was noted, with the main shaft passing through the myometrium in the isthmic region and projecting its arms into the bladder lumen (Image A). At this point, the possibility of cystoscopic management was considered.
At 11 weeks and 4 days, the patient was then referred to Santa Casa de Misericórdia de Vitória Hospital, where she was admitted for surgical cystoscopy to attempt removal of the device. The patient was informed of the risks, such as rupture of amniotic membranes, placental abruption, retroplacental bleeding, and miscarriage, as well as the benefits of the procedure, including reduced risk of chorioamnionitis, preterm rupture of membranes, and recurrent urinary tract infections.
On November 14, 2023, at 11 weeks and 5 days, the patient underwent surgical cystoscopy, performed by the Gynecology team at Santa Casa de Misericórdia de Vitória. Spinal anesthesia was administered, and the surgery was performed through urethral access with a cystoscope, where the IUD was located (Images B and C), in the anterior bladder wall, with the shaft projecting toward the myometrium. The IUD was removed using a Bertocci forceps from the upper pole of the shaft (Image D).
An ultrasound was performed to ensure fetal vitality, and the patient was discharged early, one day after the procedure. She was kept on a retention catheter for ten days, without any complications.
The patient continued follow-up at the high-risk prenatal service at Pró Matre, with no complications during the pregnancy. She underwent a cesarean delivery at 39 weeks’ gestation due to a short interdelivery interval, achieving a favorable outcome.

Image A: The IUD shaft is seen piercing through the uterus and bladder, as observed during ultrasound.
Images B and C: Images of the IUD observed during cystoscopy.
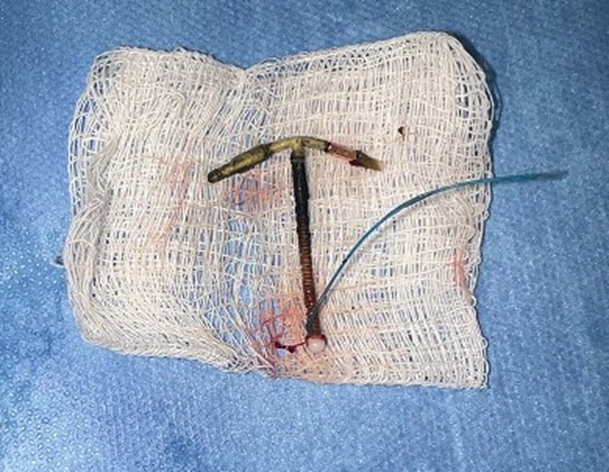
Image D: The IUD removed from the patient.
DISCUSSION
The case described involves an ectopic copper IUD in an intravesical location, with the shaft transfixing both the bladder and the uterine cavity, the arms in the bladder, and the thread visible during a speculum examination of the patient’s cervix. Simultaneously, a viable pregnancy was present, which is a rare and clinically challenging situation. Epidemiological studies indicate that the incidence of ectopic IUDs ranges from 0.1% to 2.2% of pregnancies in patients using IUDs, with most cases being intrauterine, while ectopia to the intravesical cavity is even rarer (Gyasi-Sarpong et al., 2016; Verstraeten, Vossaert & Van den Bosch, 2024). Literature reports various ectopic locations for the IUD, such as intraperitoneal, ovarian, cervical, and tubal (Pereira et al., 2010). Each location presents unique challenges in diagnosis and management, depending on associated symptoms and complications.
Case reports frequently highlight potential complications associated with ectopic IUDs during pregnancy, including miscarriage, uterine rupture, intrauterine infection, and placenta previa (Khan & Ghosh, 2018). Management of these complications requires individualized and multidisciplinary approaches.
However, there are cases in the literature where the pregnancy was monitored without IUD removal due to late diagnosis, and the outcome was favorable (Hoscan et al., 2006), with full-term delivery without complications, and the device was removed postpartum. This underscores the importance of accurate diagnosis and more studies to define protocols for management to ensure the well-being of the maternal-fetal pair.
In most cases, the literature suggests that surgical removal of the ectopic IUD, often through laparoscopy, cystoscopy, or hysteroscopy, is frequently required to reduce complications (Verstraeten et al., 2024; Haiying Niu et al., 2015). The choice of surgical technique depends on the IUD’s location and the patient’s clinical condition. In cases like the one described, where the IUD is located in the bladder wall, cystoscopy is commonly used, as was performed in another case found in the literature (Correia et al., 2022). The literature emphasizes the importance of close monitoring of pregnant women after ectopic IUD removal to track the pregnancy’s evolution and detect any complications early (Gyasi-Sarpong et al., 2016). Favorable outcomes depend on early detection and appropriate management of associated complications.
CONCLUSION
Based on the experience in the service and the literature reviewed, it is clear that monitoring after IUD insertion is essential to evaluate whether it is correctly positioned and functioning properly.
Furthermore, in cases like the one described, it is crucial that the patient be appropriately managed in high-risk prenatal care and in a service capable of offering the appropriate treatment options to ensure the best possible outcome.
Given the clinical outcome of the patient, the importance of multidisciplinary clinical follow-up for decision-making and proper management of ectopic IUDs is evident, ensuring the safety of both the mother and the fetus. Further studies may be needed to fully understand the risk factors and optimize clinical guidelines for this specific condition.
REFERENCES
VERSTRAETEN, V.; VOSSAERT, K.; VAN DEN BOSCH, T. Migration of intra-uterine devices. Open Access Journal of Contraception, 2024. Available at: https://www.dovepress.com/article/download/91167.
PEREIRA, B. J. et al. Spontaneous transuterine transvesical migration of an intrauterine device. 2010. Available at: https://apurologia.pt/wp-content/uploads/2018/10/migracao-transuterina.pdf.
GYASI-SARPONG, C. K. et al. Intravesical migration of an intrauterine device. Journal of Medical Case Reports, 2016. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698325/.
SECRETARIA DE SAÚDE, Prefeitura Municipal de Guarulhos – SP. Protocol Intrauterine Device – IUD. 2024. Available at: https://www.guarulhos.sp.gov.br/sites/default/files/file/arquivos/Protocolo%20DIU%20 finalizado%20%281%29.pdf.
KHAN, K. N.; GHOSH, B. Complications associated with intrauterine device use: A focus on ectopic migration. Contraception, v. 98, n. 5, p. 375-382, 2018. DOI: 10.1016/j.contraception.2018.07.006.
GONZÁLEZ, M. A.; DE LEÓN, G. Ectopic intrauterine device migration: A review of the literature. Journal of Obstetrics and Gynaecology, v. 37, n. 5, p. 615-620, 2017. DOI: 10.1080/01443615.2017.1304578.
CORREIA, M. J.; LOPES, A. M. Migration of intrauterine device: Case report. Revista Portuguesa de Medicina Geral e Familiar, [S. l.], v. 38, n. 1, p. 104–107, 2022. DOI: 10.32385/rpmgf.v38i1.13079. Available at: https://rpmgf.pt/ojs/index.php/rpmgf/article/view/13079.
HOSCAN, M. B. et al. Intravesical migration of intrauterine device resulting in pregnancy. International Journal of Urology, v. 13, p. 301–302, 2006.
NIU, H. et al. Partial perforation of the bladder by an intrauterine device in a pregnant woman: A case report.
