REGISTRO DOI: 10.69849/revistaft/ni10202410121322
Larissa Tarraf Bertazzo1; Natália Balbo Arantes Nogueira1; Ana Carolina Gomes de Oliveira1; Isadora Vergamini Lamana1; Daniele Costa de Sousa3; Bruno de Paula Lima3; Júlio César Claudino dos Santos2
Abstract
Attention deficit hyperactivity disorder (ADHD) consists of a set of symptoms, such as impulsivity, restlessness, difficulties in relationships with family and colleagues, which disrupt the individual’s social, personal and academic life. The aim of this study was to analyze the state of the art on non-pharmacological treatment and its effectiveness as a first-line treatment and as an adjunct to medication. The research consisted of a synthesis of the literature, presenting different types of non-pharmacological methods and their effects on the manifestations of the disease, consequently improving the social and personal lives of these patients. In this sense, it was possible to observe the importance of non-pharmacological treatment in isolation and in association with pharmacological treatment as an important coping strategy for the symptoms of individuals with ADHD.
Key words: Attention Deficit Disorder with Hyperactivity; non-pharmacological treatment; Neurology.
Introduction
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder with a prevalence of 5% during childhood and adolescence, affecting personal, social and academic performance. It is worth noting that the main symptoms of the disease consist of inattention, impulsivity and hyperactivity, leading to consequences such as learning difficulties, difficult relationships with family and peers, low self-esteem and substance abuse (Martins et al., 2019; Chen et al., 2023; Lecendreux et al., 2015; Chawla et al., 2022; Xue et al., 2021; Desidério et al., 2007).
ADHD is a common diagnosis among children. Studies show that the worldwide prevalence of ADHD is approximately 11.26%, with around 13% in Brazil among children aged 6 to 12, and in the United States 5 to 9% of children aged 5 to 12 have this diagnosis (representing 5.29% of the worldwide prevalence). Furthermore, studies show that in 67% of cases the symptoms remain into adulthood (Ayano et al., 2023; Briars et al., 2016).
There are various drugs used to treat ADHD, including stimulants, such as methylphenidate and mixed amphetamine hydrochloride; non-stimulants, including atomoxetine, clonidine and guanfacine; and some antidepressants, such as bupropion, venlafaxine, reboxetine and amitriptyline. Among the drug treatments, the most widely used is methylphenidate (Ritalin), which shows a significant improvement in 70 to 80% of cases. With the use of medication, especially methylphenidate, it is possible to observe improvements in executive functions, planning and memory (Desidério et al., 2007; Briars et al., 2016; Wu et al., 2021).
With regard to non-drug treatment, the most suitable is psychotherapy, whose main effects are to change the environment, improving the individual’s behavior, such as helping with decision-making and strategies for dealing with day-to-day problems. There are also psychoeducation groups for parents, which help them to better understand their child’s diagnosis. Another strategy that can be used is the Psychomotor Stimulation Program (PEP), which helps with the child’s hyperactivity symptoms. It is worth noting other non-pharmacological measures that are beneficial for improving patients’ symptoms, such as the use of omega 3 associated with red ginseng, Ginkgo biloba and cannabis (Effgem et al., 2017; Lee et al., 2020; Ittiphakorn et al., 2023; Shakibaei et al., 2015; Honorio Neto et al., 2021).
It’s worth pointing out that, according to the Brazilian Attention Deficit Disorder Association (ABDA), the ideal treatment for ADHD is to combine drug and non-drug treatment. Doctors and psychiatrists also believe that combining both treatments is the most effective way of controlling ADHD symptoms. This is because children with this diagnosis require extreme attention so that they can develop with as little difficulty as possible and have an adequate quality of life, thus needing help from their families, schools and a multidisciplinary team. In this way, the child will be more successful in improving the symptoms of the disease (Desidério et al., 2007; Effgem et al., 2017; Honorio Neto et al., 2021).
Thus, although the use of medication is effective in reducing the symptoms of this disorder, carrying out non-drug treatment in parallel is of paramount importance for the well-being of patients with ADHD, helping them to deal with school situations, family relationships and friendships and day-to-day difficulties. It is therefore essential to carry out a more in-depth study showing the benefits of non-pharmacological measures for treating ADHD.
Method
A narrative literature review was executed in the medline database (pubmed), from 2014 to 2024, about the role of non-pharmacological treatment strategies for attention-deficit hyperactivity disorder (ADHD). In the medline database (pubmed), 168 articles were found through the mesh descriptor “(((treatment[title/abstract]) and (treatment[text word])) and (attention deficit disorder with hyperactivity[text word])) and (attention deficit disorder with hyperactivity[title/abstract])” of which 89 were included, after the exclusion of articles following the first set of criteria – exclusion of titles that did not address the role of non-pharmacological treatment strategies for attention-deficit hyperactivity disorder (ADHD), articles not included in the research period of 2018-2023, as well as articles that were not originally in english. After this phase, a second set of criteria was applied – exclusion of the abstracts that did not address the role of non-pharmacological treatment strategies for attention-deficit hyperactivity disorder (ADHD), which led to the exclusion of 75 articles. After the selection, 7 new articles were manually selected and added, according to their relevance to the study. finally, aiming to enrich the discussion, 32 articles originally in english were manually selected and added according to their relevance in the synthesis of qualitative evidence.
Discussion
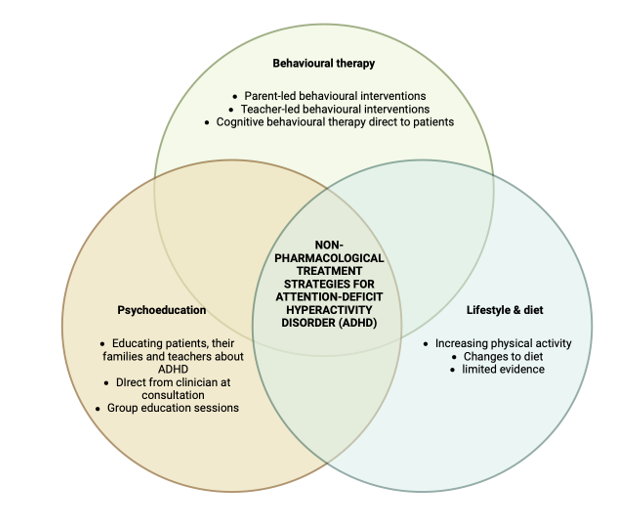
In this most recent literature review, which aimed to update the state of the art on non-pharmacological strategies for attention deficit hyperactivity disorder (figure 1), we shed light on adjunctive treatment strategies for ADHD, such as cognitive-behavioral therapy, family therapy, iron supplementation, Ginkgo Biloba, omega-3 in conjunction with Korean red ginseng, smart glasses, Ma’aljobon, cannabis-based medicines and chiropractic and their impact and degree of evidence on ADHD symptoms. In our review, cognitive-behavioral therapy proved superior to other alternatives, which lack more robust evidence. In addition, studies have shown that melatonin, goal management training, homeopathy and acupuncture did not bring results on the main symptoms of this neurodevelopmental disorder.
Figure 01. Non-pharmacological treatment strategies for attention-deficit hyperactivity disorder (ADHD).
A study was carried out to analyze the symptoms of ADHD patients when they were included in the practice of cognitive behavioral therapy (CBT), which teaches individuals to deal with their emotions, impulsivity and inattention. The study consisted of comparing CBT with supportive psychotherapy, which showed more positive results in relation to the ADHD symptoms reported by the doctor. In addition, CBT in conjunction with pharmacotherapy compared to pharmacotherapy alone proved to be superior in improving symptoms reported by the doctor and self-reported, especially symptoms of depression and anxiety (Lopez et al., 2018; Dittner et al., 2018).
Family therapy, which includes functional family therapy, cognitive-behavioral family therapy or behavioral family therapy, was also discussed as a non-pharmacological treatment for ADHD. This therapy consists of teaching parents to have greater authority and helping them to deal with their child’s disorder. Based on this study, it was identified that family therapy in relation to a placebo medication has better results in reducing ADHD symptoms (Bjornstad et al., 2005).
A study was carried out to analyze the effect of iron supplementation in children taking methylphenidate with ferritin levels below 30 ng/ml, but without anemia. It is worth noting that a lack of iron can lead to memory, psychological and mental problems. Two groups were compared, one receiving a placebo and the other a 300mg iron sulphate capsule containing 80 mg of elemental iron. This study used the Conner Parent Rating Scale, which assesses hyperactivity, attention deficit, conduct disorder, hyperactivity with attention deficit and attention deficit symptoms associated with conduct disorder. It was possible to analyze improvement in all the symptoms that the Conner scale provides, however, they showed significant improvements in conduct disorder compared to the placebo group (Tohidi et al., 2021).
Ginkgo Biloba is a medicinal plant used in Chinese medicine, the main constituents of which are flavone glycosides and terpene lactones, with clinical efficacy in disorders such as anxiety and depression, Alzheimer’s disease and dementias, impaired menorah and cerebral insufficiency. This plant was used in a study to analyze its effects on ADHD symptoms. In this trial, they compared the combination of methylphenidate and G. biloba with methylphenidate and G. biloba. Biloba with methylphenidate and placebo. The study concluded that G Biloba is an effective complementary treatment for reducing ADHD symptoms, as it showed major improvements in patients’ inattention compared to the placebo group (Shakibaei et al., 2015).
A study was carried out into the effects of omega-3 in combination with Korean red ginseng, an East Asian plant used as food or in medicinal forms, on the symptoms of ADHD patients. In this study, 40 children were given 300 mg of omega-3 and 3 mg of red ginseng, without psychotropic drugs. It is worth noting that omega-3 has several neurological symptoms through anti-inflammation, anti-oxidation, neuroplasticity and modulation of neurotransmitters. Red ginseng has a component called ginsenosides which increases dopamine and norepinephrine in the cerebral cortex. In conclusion, the study inferred that the combination of omega-3 and ginseng has great benefits for reducing ADHD symptoms, such as attention, memory and executive function (Lee et al., 2020).
Smart glasses have been developed to help coordinate the socio-emotional and behavioral symptoms of ADHD patients using sensors that detect attention and interpret other people’s emotions. Through a study, they analyzed the effect of digital smart glasses on ADHD symptoms. In the end, they concluded that the glasses have great potential for the development of people with this disorder and the improvement of symptoms. However, more studies on the subject need to be carried out (Vahabzadeh et al., 2018).
Ma’aljobon is a type of milk protein that is believed to promote immunity and prevent neuropsychiatric disorders. A study was carried out to analyze the effect of this protein on ADHD symptoms. It compared the group with standard treatment combined with Ma’aljobon and the group with standard treatment alone. It was concluded that the protein had benefits for the children’s symptoms of attention, hyperactivity and concentration (Mostajeran et al., 2020).
Cannabis-based medicines have also been analyzed for improving ADHD symptoms. It is important to point out that the cannabis plant contains phytocannabinoids, which are responsible for indirectly increasing anandamide, which when activated releases neurotransmitters and neuronal plasticity, as well as controlling dopamine transmission. The study showed good results in terms of health-related quality of life and improvements in anxiety and sleep quality. However, the effects may not be proven and further studies are needed (Ittiphakorn et al., 2023).
A study was carried out on a 5-year-old patient with ADHD, the symptoms being acting out, ability to follow instructions and poor performance at home and at school. The patient was seen by a chiropractor for a year, with spinal manipulative therapy, soft tissue therapy and stretching. At the end of the treatment, there was an improvement in the symptoms mentioned above, but more studies should be carried out on chiropractic and ADHD treatment (Muir et al., 2012).
A study was carried out to analyze the effects of melatonin on sleep, hyperactivity symptoms and attention deficiency. The drug melatonin is chemically identical to endogenous melatonin, i.e. its function is to regulate the waking cycle, but it is also an antioxidant molecule and has scavenging properties. They were divided into 2 groups, one of which combined methylphenidate with melatonin and the other with methylphenidate and placebo. In the end, there was a limited reduction in sleep disorders, but there was no difference between the groups in terms of attention deficit and hyperactivity (Mohammadi et al., 2012).
To analyze better attention control in adults with ADHD, a study used Goal Management Training (GMT), which is a metacognitive remediation program based on a group that aims to reduce goal management deficiencies, according to Duncan’s goal neglect attentional control theory. This program was used to analyze whether there would be improvements in this symptom. This study showed an improvement in executive control and the orienting network, but no change in the alerting network. It is worth noting that some patients had negative effects after mediation (Jensen et al., 2022).
Homeopathy, which is a medicine based on using natural or artificial substances for treatment, was also addressed in a study to analyze its effectiveness in reducing ADHD symptoms. There are still few reports on the subject and more trials are needed for a better conclusion, but in this study it was possible to conclude that there was no significant improvement in core symptoms, such as inattention, hyperactivity or impulsivity, nor in related symptoms, such as anxiety (Herdeiros et al., 2007).
A study was carried out to analyze the effect of acupuncture, a technique that mostly consists of inserting needles into key points on the skin that are associated with certain organs, as a treatment for ADHD, but due to the lack of trials, no conclusion could be drawn. In addition, it was also not possible to reach a conclusion due to the lack of studies on the effect of psychoeducation on ADHD symptoms (Li S., et al 2011; Hafstad et al., 2016).
With this information, it was possible to observe the importance of combining pharmacological strategies with non-pharmacological measures to enhance the treatment of ADHD. In addition, in view of the above results, it was possible to note that it is essential to combine cognitive behavioral therapy – a non-pharmacological strategy – with the use of medication in order to strengthen the approach to people with this disorder to develop a better quality of life and help them cope with the symptoms of this neurodevelopmental condition. With this in mind, it is of the utmost importance to increase the field of research in this area, in other words, as well as looking for more non-pharmacological measures to help reduce symptoms, we should also carry out larger studies over a longer period of time, so that the results really show whether or not there is an improvement.
Table 1. Methodological description of the sleep disorders described in this review.
AUTHOR STUDY TYPE NON-PHARMACOLOGICAL THERAPY THAT REDUCED SYMPTOMS WHAT IT CONSISTS OF Lopez et al., 2018 Systematic Review Cognitive Behavioral Therapy It consists of teaching the individual to deal with their emotions, impulsiveness and inattention. Bjornstad et al., 2005 Systematic Review Family Therapy Teaching parents to have greater authority and helping them to deal with their child’s disorder. Tohidi et al., 2021 Control case Iron supplementation The lack of iron can lead to myelination of the myelin sheath, and alter memory, motor and psychological abilities, as well as psychological and mental disorders. Shakibaei et al., 2015 Control case Ginkgo Biloba A medicinal plant used in Chinese medicine, the main constituents of which are flavone glycosides and terpene lactones, with clinical efficacy in disorders such as anxiety and depression, Alzheimer’s disease and dementias, impaired menorah and cerebral insufficiency. Lee et al., 2020 Clinical Trial Omega-3 together with Korean red ginseng Omega-3 has various neurological symptoms through anti-inflammation, anti-oxidation, neuroplasticity and modulation of neurotransmitters. Red Ginseng has a component called ginsenosides which increases dopamine and norepinephrine in the cerebral cortex. Vahabzadeh et al., 2018 Clinical Trial Smart glasses Developed to help coordinate the socio-emotional and behavioral symptoms of ADHD patients through sensors that detect attention and interpret other people’s emotions. Mostajeran et al., 2020 Control case Ma’aljobon It is a type of milk protein that is believed to promote immunity and prevent neuropsychiatric disorders. Ittiphakorn et al., 2023 Transversal Cannabis-based medicines The cannabis plant has phytocannabinoids, which are responsible for indirectly increasing anandamide, which when activated releases neurotransmitters and neuronal plasticity, as well as controlling dopamine transmission. Muir et al., 2012 Case Report Chiropractic Perform spinal manipulative therapy, soft tissue therapy and stretching AUTHOR STUDY TYPE NON-PHARMACOLOGICAL THERAPY THAT DOES NOT SHOW SIGNIFICANT RESULTS WHAT IT CONSISTS OF Mohammadi et al., 2012 Clinical Trial Melatonin The drug melatonin is chemically identical to endogenous melatonin, i.e. its function is to regulate the waking cycle, but it is also an antioxidant molecule and has scavenging properties. Jensen et al., 2022 Clinical Trial Goal Management Training – GMT GMT is a metacognitive remediation program based on a group that aims to reduce goal management deficiencies, according to Duncan’s attentional control theory of goal neglect. Herdeiros et al., 2007 Systematic Review Homeopathy It is a medicine based on using natural or artificial substances for treatment. Li S., et al 2011 Systematic Review Acupuncture It’s a technique that most often consists of inserting needles into key points on the skin that are associated with certain organs. Hafstad et al., 2016 Narrative Review Psychoeducation It consists of presenting the patient’s condition in detail to them and their family, with the aim of increasing adherence to treatment.
Conclusion
Through this work, it was possible to observe the importance of non-pharmacological measures in the treatment of ADHD. However, the lack of studies on the subject, studies with small samples and studies carried out in a short time limited the results of the work. This makes it necessary to carry out more studies on the subject.
References
Ayano, G., Demelash, S., Gizachew, Y., Tsegay, L., & Alati, R. (2023). The global prevalence of attention deficit hyperactivity disorder in children and adolescents: An umbrella review of meta-analyses. Journal of affective disorders, 339, 860–866. https://doi.org/10.1016/j.jad.2023.07.071
Bjornstad GJ, Montgomery P. Terapia familiar para transtorno de déficit de atenção ou transtorno de déficit de atenção/hiperatividade em crianças e adolescentes. Banco de Dados Cochrane de Revisões Sistemáticas 2005, Edição 2. Art. Nº: CD005042. DOI: 10.1002/14651858.CD005042.pub2. Acessado em 30 de março de 2024.
Briars, L., & Todd, T. (2016). A Review of Pharmacological Management of Attention-Deficit/Hyperactivity Disorder. The journal of pediatric pharmacology and therapeutics : JPPT : the official journal of PPAG, 21(3), 192–206. https://doi.org/10.5863/1551-6776-21.3.192
Chawla, G. K., Juyal, R., Shikha, D., Semwal, J., Tripathi, S., & Bhattacharya, S. (2022). Attention deficit hyperactivity disorder and associated learning difficulties among primary school children in district Dehradun, Uttarakhand, India. Journal of education and health promotion, 11, 98. https://doi.org/10.4103/jehp.jehp_922_21
Desidério, R. C. S., & Miyazaki, M. C. de O. S.. (2007). Transtorno de Déficit de Atenção / Hiperatividade (TDAH): orientações para a família. Psicologia Escolar e Educacional, 11(1), 165‑176. https://doi.org/10.1590/S1413-85572007000100018
Dittner, A. J., Hodsoll, J., Rimes, K. A., Russell, A. J., & Chalder, T. (2018). Cognitive-behavioural therapy for adult attention-deficit hyperactivity disorder: a proof of concept randomised controlled trial. Acta psychiatrica Scandinavica, 137(2), 125–137. https://doi.org/10.1111/acps.12836
Effgem, Virginia, Canal, Cláudia Patrocínio Pedroza, Missawa, Daniela Dadalto Ambrozine, & Rossetti, Claudia Broetto. (2017). A visão de profissionais de saúde acerca do TDAH – processo diagnóstico e práticas de tratamento. Construção psicopedagógica, 25(26), 34-45. Recuperado em 09 de maro de 2024, de http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1415-69542017000100005&lng=pt&tlng=pt.
Hafstad, E., & Leiknes, K. A. (2016). Psychoeducation for Adults with Attention Deficit Hyperactivity Disorder (ADHD): Rapid Review. Knowledge Centre for the Health Services at The Norwegian Institute of Public Health (NIPH).
Herdeiros M, Dean ME. Homeopatia para transtorno de déficit de atenção/hiperatividade ou transtorno hipercinético. Banco de Dados Cochrane de Revisões Sistemáticas 2007, Edição 4. Art. Nº: CD005648. DOI: 10.1002/14651858.CD005648.pub2. Acessado em 29 de março de 2024.
Honorio Neto, F., Camargo, A. P., Polanczyk, G., Adamis, D., & McNicholas, F. (2021). A mixed methods study of clinician reported challenges in the assessment of ADHD and treatment decisions for children with ADHD in Brazil. Clinical child psychology and psychiatry, 26(2), 505–517. https://doi.org/10.1177/1359104521994634
Ittiphakorn, P., Erridge, S., Holvey, C., Coomber, R., Rucker, J. J., & Sodergren, M. H. (2023). UK Medical Cannabis Registry: An analysis of clinical outcomes of medicinal cannabis therapy for attention-deficit/hyperactivity disorder. Neuropsychopharmacology reports, 43(4), 596–606. https://doi.org/10.1002/npr2.12400
Jensen, D. A., Lundervold, A. J., Stubberud, J., Halmøy, A., Haavik, J., & Sørensen, L. (2022). Goal management training improves executive control in adults with ADHD: an open trial employing attention network theory to examine effects on attention. BMC psychology, 10(1), 207. https://doi.org/10.1186/s40359-022-00902-9
Lee, J., Lee, A., Kim, J. H., Shin, Y. M., Kim, S. J., Cho, W. D., & Lee, S. I. (2020). Effect of Omega-3 and Korean Red Ginseng on Children with Attention Deficit Hyperactivity Disorder: An Open-Label Pilot Study. Clinical psychopharmacology and neuroscience : the official scientific journal of the Korean College of Neuropsychopharmacology, 18(1), 75–80. https://doi.org/10.9758/cpn.2020.18.1.75
Li S, Yu B, Zhou D, He C, Kang L, Wang X, Jiang S, Chen X. Acupuntura para Transtorno de Déficit de Atenção e Hiperatividade (TDAH) em crianças e adolescentes. Banco de Dados Cochrane de Revisões Sistemáticas 2011, Edição 4. Art. Nº: CD007839. DOI: 10.1002/14651858.CD007839.pub2. Acesso em 29 de março de 2024.
Lopez PL, Torrente FM, Ciapponi A, Lischinsky AG, Cetkovich-Bakmas M, Rojas JI, Romano M, Manes FF. Intervenções cognitivo-comportamentais para transtorno de déficit de atenção e hiperatividade (TDAH) em adultos. Banco de Dados Cochrane de Revisões Sistemáticas 2018, Edição 3. Art. Nº: CD010840. DOI: 10.1002/14651858.CD010840.pub2. Acessado em 29 de março de 2024.
Mohammadi, M. R., Mostafavi, S. A., Keshavarz, S. A., Eshraghian, M. R., Hosseinzadeh, P., Hosseinzadeh-Attar, M. J., Kooshesh, S. M., Chamari, M., & Akhondzadeh, S. (2012). Melatonin effects in methylphenidate treated children with attention deficit hyperactivity disorder: a randomized double blind clinical trial. Iranian journal of psychiatry, 7(2), 87–92.
Mostajeran, Z., Mosavat, S. H., Najafi, M., Emtiazy, M., & Hashempur, M. H. (2020). Whey Protein (Ma’aljobon) as a Complementary Therapy for Treatment of Attention-deficit/ Hyperactivity Disorder (ADHD): A Randomized Open-label Controlled Clinical Trial. Galen medical journal, 9, e1690. https://doi.org/10.31661/gmj.v9i0.1690
Muir J. M. (2012). Chiropractic management of a patient with symptoms of attention-deficit/hyperactivity disorder. Journal of chiropractic medicine, 11(3), 221–224. https://doi.org/10.1016/j.jcm.2011.10.009
Shakibaei, F., Radmanesh, M., Salari, E., & Mahaki, B. (2015). Ginkgo biloba in the treatment of attention-deficit/hyperactivity disorder in children and adolescents. A randomized, placebo-controlled, trial. Complementary therapies in clinical practice, 21(2), 61–67. https://doi.org/10.1016/j.ctcp.2015.04.001
Tohidi, S., Bidabadi, E., Khosousi, M. J., Amoukhteh, M., Kousha, M., Mashouf, P., & Shahraki, T. (2021). Effects of Iron Supplementation on Attention Deficit Hyperactivity Disorder in Children Treated with Methylphenidate. Clinical psychopharmacology and neuroscience : the official scientific journal of the Korean College of Neuropsychopharmacology, 19(4), 712–720. https://doi.org/10.9758/cpn.2021.19.4.712
Vahabzadeh, A., Keshav, N. U., Salisbury, J. P., & Sahin, N. T. (2018). Improvement of Attention-Deficit/Hyperactivity Disorder Symptoms in School-Aged Children, Adolescents, and Young Adults With Autism via a Digital Smartglasses-Based Socioemotional Coaching Aid: Short-Term, Uncontrolled Pilot Study. JMIR mental health, 5(2), e25. https://doi.org/10.2196/mental.9631
Wu, C. S., Shang, C. Y., Lin, H. Y., & Gau, S. S. (2021). Differential Treatment Effects of Methylphenidate and Atomoxetine on Executive Functions in Children with Attention-Deficit/Hyperactivity Disorder. Journal of child and adolescent psychopharmacology, 31(3), 187–196. https://doi.org/10.1089/cap.2020.0146
Xue, J., Hao, Y., Li, X., Guan, R., Wang, Y., Li, Y., & Tian, H. (2021). Meta-Analysis Study on Treatment of Children’s Attention Deficit Disorder with Hyperactivity. Journal of healthcare engineering, 2021, 8229039. https://doi.org/10.1155/2021/8229039 (Retraction published J Healthc Eng. 2023 Nov 1;2023:9781805)
1Centro universitário Barão de Mauá, CBM, Ribeirão Preto, São Paulo, Brasil.
2Universidade Federal do Ceará, UFC, Fortaleza, Ceará, Brasil.
3Universidade Federal do Amapá, UNIFAP, Macapá, Amapá, Brasil.
