USE OF PLATELET-RICH FIBRIN (PRF) IN TRAUMATIC SINUS LIFT ASSOCIATED WITH DENTAL IMPLANTS: CASE REPORT
USO DE FIBRINA RICA EN PLAQUETAS (PRF) EN LA ELEVACIÓN TRAUMÁTICA DE SENO ASOCIADO A IMPLANTES DENTALES: REPORTE DE UN CASO
REGISTRO DOI: 10.69849/revistaft/th10249181438
Vanessa Malcher da Silva1
Rafael Reis de Souza2
ABSTRACT
Dentistry has advanced significantly in recent decades, especially in the field of bone and tissue regeneration, with emphasis on Platelet-Rich Fibrin (PRF). This autologous biomaterial has been used in procedures such as maxillary sinus lifting, offering improvements in healing and quality of regenerated bone, crucial in cases of bone atrophy. This article reports the case of a 42-year-old female patient with a history of edentulism and significant bone resorption in the regions of teeth 14, 15, 24 and 25. The patient had chewing difficulties and aesthetic impairment. The treatment plan included the installation of Titaniumfix® osseointegrated implants and the use of PRF to promote bone regeneration. The technique was successfully performed, and was evidenced by radiographic examinations that showed satisfactory bone regeneration and adequate for the installation of implants. The use of PRF accelerated the healing process and improved the stability of the implants, resulting in successful rehabilitation, both functional and aesthetic. The combination of PRF and implants proved to be effective in overcoming the challenges posed by severe bone resorption, confirming the potential of this biomaterial as a viable and efficient solution in maxillary sinus lift procedures. The present clinical case reinforces the importance of PRF in modern surgical practice, demonstrating that its application can significantly transform the results of implantological treatments.
Keywords: Bone Regeneration. Dental Implants. Platelet-Rich Fibrin. Cicatrization.
RESUMEN
La odontología ha avanzado significativamente en las últimas décadas, especialmente en el campo de la regeneración ósea y tisular, con énfasis en la Fibrina Rica en Plaquetas (PRF). Este biomaterial autólogo se ha utilizado en procedimientos como la elevación del seno maxilar, ofreciendo mejoras en la cicatrización y la calidad del hueso regenerado, crucial en casos de atrofia ósea. Presentamos el caso de una paciente femenina de 42 años con antecedentes de edentulismo y reabsorción ósea importante en las regiones de los dientes 14, 15, 24 y 25. El paciente presentaba dificultades para masticar y deterioro estético. El plan de tratamiento incluía la instalación de implantes osteointegrados Titaniumfix® y el uso de PRF para promover la regeneración ósea. La técnica fue realizada con éxito, y se evidenció con exámenes radiográficos que mostraron una regeneración ósea satisfactoria y adecuada para la instalación de implantes. El uso de PRF aceleró el proceso de cicatrización y mejoró la estabilidad de los implantes, lo que resultó en una rehabilitación exitosa, tanto funcional como estética. La combinación de PRF e implantes demostró ser eficaz para superar los desafíos planteados por la resorción ósea severa, lo que confirma el potencial de este biomaterial como una solución viable y eficiente en los procedimientos de elevación de seno maxilar. El presente caso clínico refuerza la importancia de la PRF en la práctica quirúrgica moderna, demostrando que su aplicación puede transformar significativamente los resultados de los tratamientos implantológicos.
Palabras clave: Regeneración ósea. Implantes dentales. Fibrina rica en plaquetas. Cicatrización.
RESUMO
A Odontologia tem avançado significativamente nas últimas décadas, especialmente no campo da regeneração óssea e tecidual, com destaque para a Fibrina Rica em Plaquetas (PRF). Este biomaterial autólogo tem sido utilizado em procedimentos como o levantamento de seio maxilar, oferecendo melhorias na cicatrização e qualidade do osso regenerado, crucial em casos de atrofia óssea. O presente artigo relata o caso de uma paciente de 42 anos, com histórico de edentulismo e reabsorção óssea significativa nas regiões dos dentes 14, 15, 24 e 25. A paciente apresentava dificuldades mastigatórias e comprometimento estético. O plano de tratamento incluiu a instalação de implantes osseointegrados Titaniumfix® e a utilização de PRF para promover a regeneração óssea. A técnica foi executada com sucesso, sendo evidenciada por exames radiográficos que mostraram uma regeneração óssea satisfatória e adequada para a instalação dos implantes. O uso do PRF acelerou o processo de cicatrização e melhorou a estabilidade dos implantes, resultando em uma reabilitação bem-sucedida, tanto funcional quanto estética. A combinação do PRF com os implantes mostrou-se eficaz na superação dos desafios impostos pela reabsorção óssea severa, confirmando o potencial desse biomaterial como uma solução viável e eficiente em procedimentos de levantamento de seio maxilar. O presente caso clínico reforça a importância do PRF na prática cirúrgica moderna, demonstrando que sua aplicação pode transformar significativamente os resultados dos tratamentos implantológicos.
Palavras-chave: Regeneração Óssea. Implantes Dentários. Fibrina Rica em Plaquetas. Cicatrização.
1 INTRODUCTION
Dentistry has advanced significantly in recent decades, especially in the field of bone and tissue regeneration. Innovations in biomaterials and technologies have provided substantial improvements in surgical techniques, expanding therapeutic options and making treatments more effective and predictable. Among these innovations, Platelet-Rich Fibrin (PRF) stands out, a technique that has gained attention due to its promising results in surgical procedures, such as maxillary sinus lift associated with dental implants1,2.
The maxillary sinus lift technique aims to increase bone height in the posterior region of the maxilla, being crucial in cases of bone atrophy or sinus pneumatization, which can make it difficult to install dental implants. Bone loss in the maxillary sinus, often exacerbated by anatomical structure and bone resorption after tooth extractions, presents significant challenges for implant placement. Maxillary sinus elevation is a common approach to create an adequate space for implants, but its effectiveness may be limited by anatomical and technical variables, such as perforations in the Schneiderian membrane and differences in bone thickness3,4.
Traditionally, bone graft materials, such as autogenous, allografts, alloplastics, and xenografts, have been used to promote bone regeneration necessary to support dental implants. However, these biomaterials often present challenges related to cost, availability, and biocompatibility, which has driven the search for more effective and affordable alternatives. The PRF has emerged as an innovative and promising solution in this context5,6.
PRF is an autologous biomaterial obtained from the patient’s blood, which contains a high concentration of platelets, leukocytes, and fibrin, as well as a wide range of growth factors and cytokines. They are essential for promoting healing and tissue regeneration, offering an environment conducive to the formation of new bone tissue. The application of PRF in maxillary sinus elevation can accelerate the healing process, improve the quality of regenerated bone, and reduce the need for additional bone grafts7,8.
PRF’s ability to continuously release growth factors such as PDGF, TGF-β, and VEGF provides additional support for bone regeneration, which is crucial in preparing the bone bed for dental implants. In particular, this ability is important in areas with significant bone impairment, where efficient promotion of healing is essential for implant success. In addition, PRF is considered a low-cost and easy-to-prepare alternative, simplifying the procedure and eliminating the need for anticoagulants or additional substances9,10.
In addition to its benefits in bone regeneration, PRF has also shown advantages in soft tissue healing. In cases of post-trauma maxillary sinus lift, where tissue integrity may be compromised, PRF offers a regenerative approach that minimizes complications and improves clinical outcomes. Bone regeneration facilitated by PRF can result in a more solid bone base for implant installation, increasing stability and success rate11,12.
The combination of PRF with traditional bone grafts can enhance the effects of both, resulting in more robust regeneration and better implant integration. The synergy between these materials creates a favorable environment for bone neoformation and soft tissue recovery, which are essential for the long-term success of dental implants. The use of PRF, as an autologous material, reduces the risk of rejection and immunological complications, making it a safe and effective choice13,14.
The application of PRF in maxillary sinus lift procedures associated with dental implants represents a significant evolution in bone regeneration and healing techniques. By promoting efficient regeneration and accelerated healing, PRF allows patients with challenging bone conditions to be treated with greater safety and predictability. The continuity of research and the clinical application of PRF can contribute to the improvement of dental rehabilitation techniques and to the expansion of the therapeutic options available to dental professionals15,16.
Therefore, the use of PRF in maxillary sinus lift associated with dental implants represents a promising and innovative solution, with the potential to transform dental rehabilitation practice and significantly improve the outcomes of implantological treatments. The integration of biomaterials science with surgical practice highlights the importance of continuing to investigate and refine these techniques to maximize their clinical benefits17,18.
In this sense, the objective of this study is to report a clinical case that uses PRF in the lifting of the traumatic maxillary sinus, associated with the installation of dental implants.
2 CASE REPORT
Patient S. C. S., female, 42 years old, attended the specialization clinic in Implantology of the Faculty of Amazonas – IAES with the main complaint of difficulty in chewing and aesthetic impairment due to tooth loss. During the anamnesis, the patient reported a history of edentulism in the regions of teeth 14, 15, 24 and 25, associated with complaints of occasional discomfort and loss of masticatory function. No systemic medical conditions were identified that could contraindicate the proposed treatment.
Extraoral physical examination revealed no significant changes. On intraoral physical examination, teeth 14, 15, 24 and 25 were absent. The corresponding region showed significant bone resorption, especially in the areas of teeth 14 and 15, as evidenced by the analysis of the requested panoramic radiograph. Radiography revealed considerable bone atrophy in the edentulous regions, compromising the installation of dental implants without additional intervention (Figure 1).
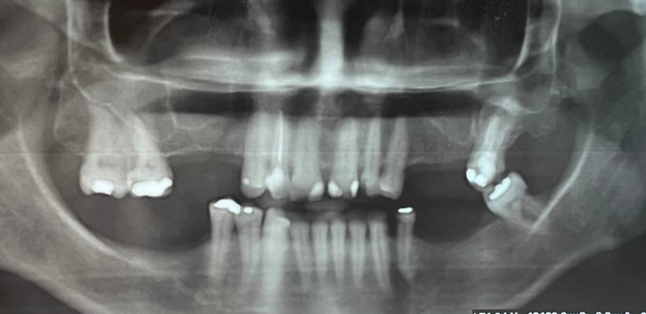
Figure 1 – Initial panoramic radiography
After confirming the diagnosis and discussing treatment options, the patient signed the consent forms and authorization to use the image to participate in the procedure (Appendices A-B). The treatment plan included the installation of Titaniumfix® osseointegrated implants and the use of PRF to promote bone regeneration and accelerate healing.
The surgical procedure was initiated with the application of local anesthesia using 4% articaine with epinephrine 1:100,000 (DFL®) with block of the posterior superior alveolar nerve, middle alveolar nerve and the greater palatine nerve, with a 27 G® long needle. The incision was made in the posterior region of the maxilla, following a curved design that allowed the flap to be reflected in order to adequately expose the area to be prepared for the implant installation (Figure 2). The mucoperiostic flap was gently detached using a periosteal elevator (Hu-Friedy®) to ensure adequate exposure of the bone bed and preserve the vascularization of the tissue (Figure 2).
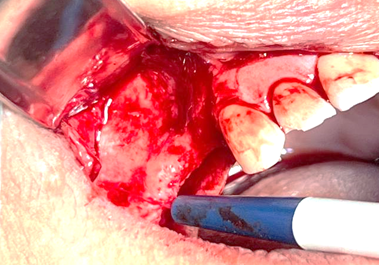
Figure 2 – Incision made and tissue detachment
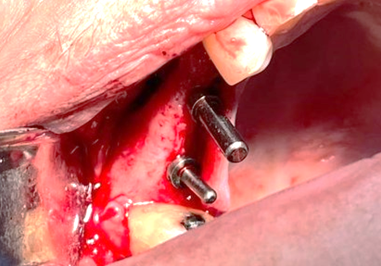
Figure 3 – Incision made and tissue detachment
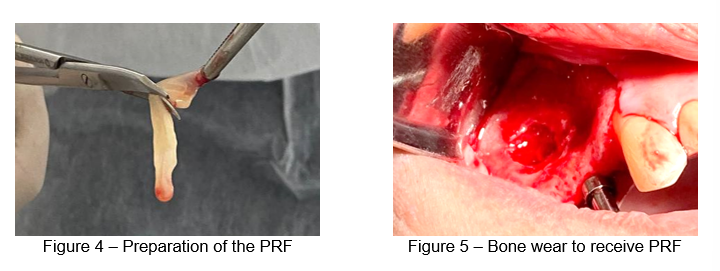
Prior to bone preparation, the preparation of the PRF began. The patient’s blood was collected in 20 ml of tubes containing sodium citrate as an anticoagulant and processed in a centrifuge at 2,700 rpm for 12 minutes. Centrifugation resulted in the separation of the blood into three distinct layers: red blood cells at the bottom, PRF at the middle layer, and plasma at the top. The PRF layer was carefully removed and prepared for application. Then, bone preparation was carefully performed to receive the PRF. The bone surface was smoothed and debrided using bone curettes (Hu-Friedy®) to remove any necrotic tissue and provide an ideal surface for PRF adhesion and implant installation (Figure 4).
The synthetic bone was adhered to and on top, with a straight forceps, the fibrin membranes were placed inside the bone cavity, lining it to receive the Sticky cap. After insertion of the bone graft, it was covered by PRF membranes (Figure 6). At the end, a simple suture was performed with 3-0 nylon thread (Figure 7). Afterwards, a panoramic X-ray was performed to visualize the final position of the implants and ensure their correct installation. Radiographic imaging confirmed the proper positioning of the implants and the integrity of the grafted areas, demonstrating a successful and uncomplicated insertion (Figure 8). The same procedures were performed on teeth 24 and 25. The patient was provided with a postoperative care protocol, including analgesia, antibiotics, and guidance on oral hygiene.
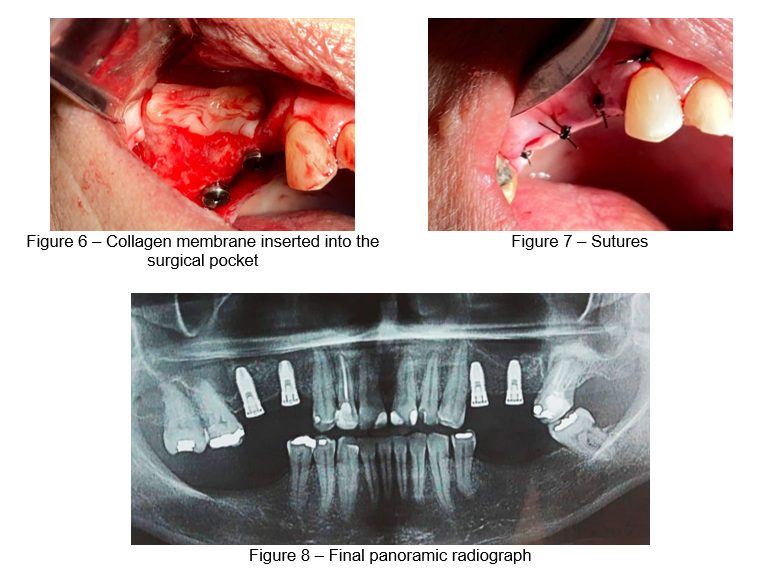
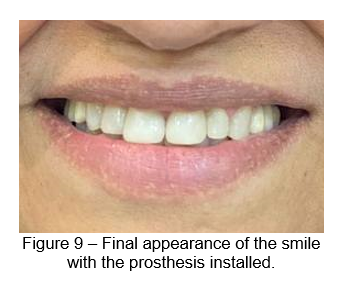
Postoperative follow-up was scheduled for six months in order to monitor healing and implant integration. After this period, the prosthetic phase was performed, based on subsequent radiographic and clinical evaluations. The patient returned for follow-up, demonstrating satisfaction with the procedure and with the aesthetic result of her smile (Figure 9).
This report highlights the successful integration of bone regeneration techniques with the use of PRF and osseointegrated implants, evidencing the efficacy of PRF in promoting healing and improving clinical outcomes in cases of severe bone resorption.
3 DISCUSSION
The analysis of the results obtained in this clinical case, involving the use of PRF and osseointegrated implants for the rehabilitation of the atrophic maxilla, is in line with the findings of previous studies that highlight the efficacy of PRF in promoting bone healing and in the integration of implants. Malzoni et al.19 and Idiri et al.20 showed that PRF, due to its autologous properties and its ability to gradually release growth factors, plays a crucial role in the acceleration of osteogenesis, which was also observed in the present case. The combination of PRF with osseointegrated implants, as shown in this report, offers additional support for primary stability and bone regeneration, corroborating the conclusions of these authors about the benefits of PRF in implant dentistryprocedures 21.
Additionally, as demonstrated by Elsheikh et al.22 suggest that the application of PRF in maxillary sinus lift surgeries not only increases the rate of bone formation, but also reduces postoperative morbidity. These effects were consistent with the results of the case reported, in which the patient presented rapid healing and minimal inflammatory reaction, attributes frequently associated with the use of PRF, as pointed out by these authors. The efficacy observed in this case also reflects the evidence that PRF can improve local vascularization, providing a more favorable environment for osseointegration, as discussed by Ozeki et al.23.
On the other hand, the work of Malcangi et al.24 highlights the variability of clinical outcomes with the use of PRF, depending on the preparation technique and the individual characteristics of the patients. In the present case, the centrifugation technique was rigorously standardized, which may have contributed to the positive results obtained. The literature mentions that failures in the standardization of PRF can lead to an inconsistency in clinical results20,25, which was not observed here, reinforcing the importance of well-controlled techniques to maximize the benefits of PRF in regenerative procedures.
In addition, studies such as those by Afifi et al.16 and Malzoni et al.19 indicate that the use of PRF in conjunction with synthetic bone grafts can enhance the effects of both materials, promoting greater bone regeneration in areas with significant bone loss. In the clinical case reported here, the combination of PRF with synthetic bone graft resulted in a satisfactory bone density for implant placement, suggesting that this combined approach may be an effective strategy in similar cases of severe bone resorption, as supported by the findings of these authors.
The report by Koç et al.15 also points to the importance of proper torque and precise alignment during implant installation to ensure primary stability and long-term bone integration. These factors were strictly controlled in the present case, which, together with the use of PRF, may have contributed to the absence of complications and to the success of the treatment. The relevance of this technical care is widely discussed in the literature as fundamental for the success of dental implants, especially in cases of atrophic maxillary rehabilitation20,23.
In turn, the literature also addresses the potential limitations of the use of PRF, especially in patients with systemic conditions that may compromise healing6,12. In the case reported here, the absence of significant comorbidities in the patient may have favored the positive results, in line with the observations of these studies, which suggest that PRF may not be equally effective in all patients. This highlights the need for a careful evaluation before opting for the use of PRF, considering the individuality of each clinical case7.
It is important to mention that while PRF has shown clear benefits in healing and implant integration, authors such as Hartlev et al.18 and Garg et al.21 argue that there is still a need for long-term clinical studies that validate these results in broader populations. The clinical case presented contributes to this discussion by providing additional evidence of the success of PRF in a specific context, but reinforces the need for further research to establish more comprehensive clinical guidelines for the use of this biomaterial in different clinical situations.
The present clinical case is in line with a vast literature that supports the use of PRF as an effective tool in maxillary sinus lift surgeries and implant installation in cases of severe bone resorption. At the same time, it contributes to the body of knowledge by confirming the benefits of PRF in healing and implant integration, while highlighting the importance of an accurate technique and individualized patient assessment, essential elements for successful treatment.
4 CONCLUSION
The present clinical case confirmed the efficacy of the use of PRF associated with the installation of Titaniumfix® osseointegrated implants in a patient with severe bone resorption in the maxilla, demonstrating that this approach provides accelerated healing and satisfactory bone integration. The technique employed, including the proper preparation of the PRF and the precise control of the torque and alignment of the implants, resulted in a successful rehabilitation, meeting the objective of reestablishing the patient’s masticatory function and aesthetics.
REFERENCES
1. Iviglia G, Kargozar S, Baino F. Biomaterials, Current Strategies, and Novel Nano-Technological Approaches for Periodontal Regeneration. J Funct Biomater [Internet]. 2019;10(1). Available from: https://www.mdpi.com/2079-4983/10/1/3
2. Yazdanian M, Rahmani A, Tahmasebi E, Tebyanian H, Yazdanian A, Mosaddad SA. Current and Advanced Nanomaterials in Dentistry as Regeneration Agents: An Update. Mini-Reviews Med Chem. 2022;21(7):899–918.
3. Ucer C, Khan RS. Alveolar Ridge Preservation with Autologous Platelet-Rich Fibrin (PRF): Case Reports and the Rationale. Dent J. 2023 Oct;11(10).
4. Agrawal AA. Platelet rich fibrin is not a barrier membrane! Or is it? World J Clin cases. 2023 Apr;11(11):2396–404.
5. Al-Maawi S, Becker K, Schwarz F, Sader R, Ghanaati S. Efficacy of platelet-rich fibrin in promoting the healing of extraction sockets: a systematic review. Int J Implant Dent. 2021 Dec;7(1):117.
6. Miron RJ, Pikos MA, Estrin NE, Kobayashi-Fujioka M, Espinoza AR, Basma H, et al. Extended platelet-rich fibrin. Periodontol 2000. 2024 Feb;94(1):114–30.
7. Miron RJ, Fujioka-Kobayashi M, Sculean A, Zhang Y. Optimization of platelet-rich fibrin. Periodontol 2000. 2024 Feb;94(1):79–91.
8. Zwittnig K, Mukaddam K, Vegh D, Herber V, Jakse N, Schlenke P, et al. Platelet-Rich Fibrin in Oral Surgery and Implantology: A Narrative Review. Transfus Med hemotherapy Off Organ der Dtsch Gesellschaft fur Transfusionsmedizin und Immunhamatologie. 2023 Aug;50(4):348–59.
9. Oliveira ES de, Ribas-Filho JM, Sigwalt M, Lourenço ES, Figueiredo FP, Czeczko NG, et al. Platelet-rich fibrin improves the osteoneogenesis in non-critical defects in calvaria: a histological and histometric study. Acta Cir Bras. 2023;38:e383423.
10. Sybil D, Sawai M, Faisal M, Singh S, Jain V. Platelet-Rich Fibrin for Hard- and Soft-Tissue Healing in Mandibular Third Molar Extraction Socket. Ann Maxillofac Surg. 2020;10(1):102–7.
11. Shah R, Gowda TM, Thomas R, Kumar T, Mehta DS. Biological activation of bone grafts using injectable platelet-rich fibrin. J Prosthet Dent. 2019 Mar;121(3):391–3.
12. Naqvi A, Mishra G, Shahi S, Shakarwal P, Singh A, Singh R. Comparison between Platelet-rich Fibrin and Saline Filling after Sinus Elevation without Adjunctive Bone Graft in Dental Implants Insertion Using CBCT. J Contemp Dent Pract. 2023 Jan;24(1):9–15.
13. Polak D, Falcoff D, Chackartchi T, Asher R, Assad R. Sustainability and Release Pattern of Growth Factors from Bone Grafts Prepared with Platelet-Rich Fibrin. Int J Oral Maxillofac Implants. 2024 Jun;(3):473–8.
14. Pavani MP, Reddy KRKM, Reddy BH, Biraggari SK, Babu CHC, Chavan V. Evaluation of platelet-rich fibrin and tricalcium phosphate bone graft in bone fill of intrabony defects using cone-beam computed tomography: A randomized clinical trial. J Indian Soc Periodontol. 2021;25(2):138–43.
15. Koç S, Çakmak S, Gümüşderelioğlu M, Ertekin TS, Çalış M, Yılmaz MM, et al. Three dimensional nanofibrous and compressible poly(L-lactic acid) bone grafts loaded with platelet-rich plasma. Biomed Mater. 2021 Apr;16(4).
16. Afifi HHAL, Nasr SS, BinShabaib MS, Alharthi SS, Shoeib M. Socket Preservation Using Platelet-Rich Fibrin and Free Gingival Grafts. Int Dent J. 2024 Jul;
17. Blinstein B, Bojarskas S. Efficacy of autologous platelet rich fibrin in bone augmentation and bone regeneration at extraction socket. Stomatologija. 2018;20(4):111–8.
18. Hartlev J, Schou S, Isidor F, Nørholt SE. A clinical and radiographic study of implants placed in autogenous bone grafts covered by either a platelet-rich fibrin membrane or deproteinised bovine bone mineral and a collagen membrane: a pilot randomised controlled clinical trial with a 2-year foll. Int J Implant Dent. 2021 Feb;7(1):8.
19. Malzoni CM, Pichotano EC, Freitas de Paula LG, de Souza RV, Okamoto R, Austin RS, et al. Combination of leukocyte and platelet-rich fibrin and demineralized bovine bone graft enhanced bone formation and healing after maxillary sinus augmentation: a randomized clinical trial. Clin Oral Investig. 2023 Sep;27(9):5485–98.
20. Idiri K, Bandiaky O, Soueidan A, Verner C, Renard E, Struillou X. The Effectiveness of the Addition of Platelet-Rich Fibrin to Bovine Xenografts in Sinus and Bone Ridge Augmentation: A Systematic Review. J Funct Biomater. 2023 Jul;14(7).
21. Garg M, Srivastava V, Chauhan R, Pramanik S, Khanna R. Application of platelet-rich fibrin and freeze-dried bone allograft following apicoectomy: A comparative assessment of radiographic healing. Indian J Dent Res Off Publ Indian Soc Dent Res. 2023;34(1):40–4.
22. Elsheikh HAE, Abdelsameaa SE, Elbahnasi AA, Abdel-Rahman FH. Comparison between platelet rich fibrin as space filling material versus xenograft and alloplastic bone grafting materials in immediate implant placement: a randomized clinical trial. BMC Oral Health. 2023 Dec;23(1):977.
23. Ozeki N, Seil R, Krych AJ, Koga H. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS Jt Disord Orthop Sport Med. 2021 Jan;6(1):35–45.
24. Malcangi G, Patano A, Palmieri G, Di Pede C, Latini G, Inchingolo AD, et al. Maxillary Sinus Augmentation Using Autologous Platelet Concentrates (Platelet-Rich Plasma, Platelet-Rich Fibrin, and Concentrated Growth Factor) Combined with Bone Graft: A Systematic Review. Cells. 2023 Jul;12(13).
25. Amaral Valladão CAJ, Freitas Monteiro M, Joly JC. Guided bone regeneration in staged vertical and horizontal bone augmentation using platelet-rich fibrin associated with bone grafts: a retrospective clinical study. Int J Implant Dent. 2020 Oct;6(1):72.
1 Especialista em Implantodontia
Instituição: Faculdade do Amazonas – IAES (Manaus, AM)
2 Doutorando em Odontologia
Instituição: ILAPEO (Curitiba, PR)
