REGISTRO DOI: 10.5281/zenodo.10537127
HORACIO, Hariel Sá Pazianoto1
COIMBRA, Juliano Rodrigues1
SILVA, Douglas Fernandes1
ABSTRACT
INTRODUCTION: Meningitis is a worldwide pathology that has a high rate of morbidity and mortality. It consists of an inflammation that affects the meninges, especially in the subarachnoid space, cranial and spinal segments. It can manifest itself in two different forms: the bacterial form, a more serious form that can lead to death in a matter of hours, and the viral form, which is less severe and the individual recovers more quickly. OBJECTIVE: To analyze the existing literature on nurses’ care for patients affected by meningitis in Brazil, in addition to epidemiological trends of the disease. METHODOLOGY: Literature review using the main internet databases to select articles. CONCLUSIONS: Meningitis is a serious public health problem due to its high morbidity and mortality rate, especially in children. It is necessary to emphasize that vaccination is extremely effective in controlling and eradicating diseases, not just individually, but collectively, benefiting the entire community.
Keywords: Meningitis; Epidemiological Profile; Nurse.
1. INTRODUCTION
In the years 1971 and 1975, an epidemic known as Meningococcal Disease began in Brazil, the number of cases was devastating, with a high lethality and with the highest number of cases in the city of São Paulo due to the local health infrastructure (Focaccia & Negra, 2022).
The meningitis disease is a widespread worldwide illness with a high morbidity rate; its physiopathology involves inflammation of the meninges, primarily in the subarachnoid space, the cranial segment, and the medulla. The disease can manifest itself in two different forms: bacterial, which is the most serious variant and can lead to death in a matter of hours, and viral, which has a lower severity and fatality rate, with faster recovery of the individual (SILVA; MEZAROBBA, 2018).
Neisseria meningitidis, Streptococcus pneumoniae, Mycobacterium tuberculosis e Haemophilus influenzae are the main bacteria responsible for the occurrence of bacterial meningitis, the latter being a variant frequently associated with infections in children. However, Mycobacterium tuberculosis is the one with the highest mortality rate, particularly affecting children under the age of five (Dias et al., 2017).
Meningitis is a pathology that presents symptoms like those of the flu, which makes its accurate diagnosis difficult. For this reason, it is crucial that the doctor performs neurological exams and a lumbar puncture to collect cerebrospinal fluid (CSF). Affected individuals may not be able to touch their chin to their chest due to the signs and symptoms of the disease, which include headache, fever, malaise, vomiting, photophobia, petechiae, convulsions and neck stiffness. Consequently, it’s critical to emphasize that children are more likely to experience this final symptom (Amorim et al., 2022).
Due to its high contagion, meningitis is considered a serious public health problem and, therefore, is classified as a notifiable disease and must be reported 24 hours after diagnosis (Amorim et al., 2022). Epidemiological surveillance is responsible for controlling reported cases, this data is available in the Notifiable Diseases Information System (Sistema de Informações de Agravos de Notificação – SINAN) (PAIM; GREGIO; GARCIA, 2019). Meningitis can affect any age but is most common in children aged 1-4 due to their immune system not being fully mature. Treatment consists of antibiotics, and vaccination is the most efficient way to prevent meningitis, it is essential for their protection (Maimaiti et al., 2022).
The pathology known as meningitis has a high morbidity and mortality and has a significant impact on global public health. In Brazil, despite the preventive measures adopted, the disease is still responsible for a high number of cases and deaths, especially in children (Dias et al., 2017). In this context, it becomes imperative to carry out studies that could aid in understanding the epidemiology of meningitis and improving prevention and control strategies. Furthermore, the role of nurses in the clinical management of meningitis cases is essential to guarantee the quality of care provided to patients and minimize the risks of complications and sequelae. This article aimed to analyze the literature on nursing care for meningite patients in Brazil, as well as epidemiological trends of the disease, with the goal of ensuring practices and strategies to prevent complications and ensure the safety of treated patients.
2. EPIDEMIOLOGY IN BRAZIL
2.1. Analysis of regional prevalence
It is estimated that out of 1.2 million people contract meningitis, 135 thousand people die (MAIMAITI et al., 2022a). In Brazil, meningitis is considered a notifiable disease and must be reported within 24 hours of diagnosis. The Neisseria meningitidis (meningococo) is the main etiological microorganism, with a lethality rate of around 20% in Brazil. Meningitis represents an endemic condition within the Brazilian territory, exhibiting more pronounced outbreaks during the winter season and sporadic occurrences in alternative periods throughout the year. In the studies of Rodrigues Santos (RODRIGUES SANTOS, 2021), between 2010 and 2020, 204.5 thousand cases of meningitis were reported to Notifiable Diseases Information System (Sistema de Informações de Agravos de Notificação – SINAN) in Brazil. Children aged 1 to 9 were the most affected age group with around 32.2% of cases, followed by adults aged 20 and 39 with 19.3% of notifications. In total, the country’s rate was 97 cases/100 thousand inhabitants (Amorim et al., 2022).
2.2. Identification of vulnerable groups
Amorim et al., (Amorim et al., 2022) pointed out that meningitis mainly affects males, this is because this population has greater exposure to risk factors, thus contributing to the transmission of the disease. In addition, studies have shown that men are more resistant when it comes to seeking medical care.
Maimaiti et al. (Maimaiti et al., 2022) e Rodrigues (Rodrigues, 2015), report that the disease can affect any age group, being more common in children aged 1-4 years because their immune system is not completely mature. Furthermore, there are some risk factors that may be associated with the occurrence of the disease, such as: malnutrition, immunosuppression and trauma to the central nervous system and some bacterial infectious processes such as bacteremia (pneumonia, empyema, osteomyelitis, and endocarditis), sinusitis, otitis media, encephalitis, myelitis and brain abscess (Dazzi et al., 2014).
2.3. Socioeconomic inequalities and impact on nurses’ performance
Socioeconomic inequality can have a significant impact on patients with meningitis. Low-income patients may face difficulties in accessing adequate medical care, early diagnosis, and effective treatment. In this way, it can lead to serious complications and even increase the risk of mortality. In addition, socioeconomic factors such as early mortality rates and limited access to basic healthcare can increase the risk of infections, including meningitis. Patients with low incomes may have trouble getting access to quality medical care, which could have a detrimental effect on their prognosis and course of treatment (LIMA, 2017).
Therefore, the nursing team is responsible for developing technical and scientific skills, as well as knowledge, skills, and emotional control, adopting new strategies for coping with the disease, specialized psychological support and active listening, always aiming to provide qualified assistance (Dal’bosco et al., 2020).
The initial approach carried out in cases of meningitis is the sum of the Glasgow Coma Scale, which scores and adds three neurological parameters: eye opening (4), verbal response (5) and motor response (6). The maximum score is 15 points and the minimum, which is compatible with brain death, is 3. To consider intubation criteria, the sum is considered 8. In this evaluation, pupillary responses are observed, because if they become mydriatic or anisocoric and /or not responding to light, may be a sign of poor cerebral perfusion (MACHADO; BORGES, 2015).
In addition to the neurological assessment, the nurse must assess the patient’s pain level using the FACES pain scale, as if left untreated, it increases the patient’s Intracranial Pressure (ICP), causing great suffering (MACHADO; BORGES, 2015).
The patient’s vital signs must also be checked, such as blood pressure, which must remain between 120mmHg and 60mmHg; pulse oximetry, which must remain between 90 and 100%; the body temperature which cannot exceed 36.5ºC and the pulse frequency which must vary between 60 and 100 beats per minute. Therefore, to obtain thorough monitoring, all this information must be checked hourly by the nursing team (MACHADO; BORGES, 2015).
Nurses may face challenges when dealing with patients from different socioeconomic backgrounds, such as lack of financial resources, limited access to healthcare services, and lack of knowledge about preventative measures such as vaccination. Therefore, social inequality can directly affect the role of nurses in caring for patients with meningitis. They play a crucial role in the education, prevention and treatment of meningitis, adapting their strategies according to the needs and resources available to each patient (LIMA, 2017).
3. ETIOLOGY AND CAUSING AGENTS IN THE BRAZILIAN CONTEXT
As already mentioned, meningitis is a comprehensive global pathology that has a high morbidity and mortality rate. Its pathophysiological pathology consists of inflammation that affects the meninges, mainly in the subarachnoid space, cranial and spinal segments. This disease can manifest itself in two different forms: bacterial, which is the most serious variant and can lead to death in a matter of hours, and viral, which has a lower severity and fatality rate, with faster recovery of the individual (SILVA; MEZAROBBA, 2018). Figure 1 presents epidemiological data on Meningitis in Brazil between 2010 and 2020 (n=187.508).
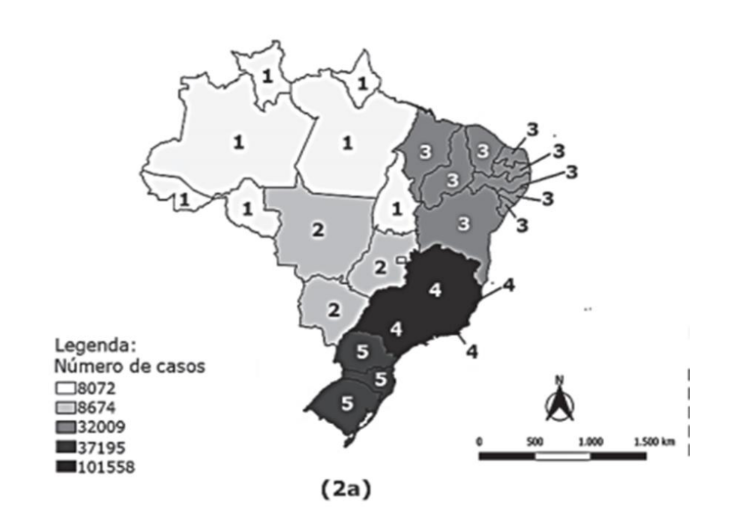
Figure 1: Epidemiological data on Meningitis in Brazil (2010-2020) (MORAES; GALDINO; TEIXEIRA, 2022).
Out of the 187.508 confirmed cases, 54,2% (n=101.558) were observed in the South and 4,3% in the North (n=8.072), correspondingly indicating the more and less affected locations in Brazil, followed by the South (19,8% / n=37.195), the North (17,1% / n=32.009), and the Central-Oeste (4,6% / n=8.674) (MORAES; GALDINO; TEIXEIRA, 2022).
Figure 2 presents epidemiological data on Meningitis in Brazil between 2010 and 2020 by Federative Unit.
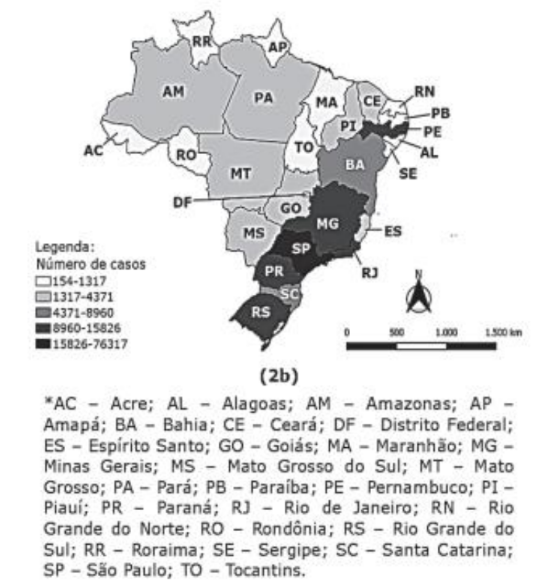
Figure 2: Epidemiological data on Meningitis in Brazil by Federative Unit (2010-2020) (MORAES; GALDINO; TEIXEIRA, 2022).
In Brazil there are 26 federative units, among them, the State with the highest number of confirmed cases was São Paulo (41% / n=76,317) and the one with the lowest number was Amapá (0.1% / n=154). Paraná had the second highest number of notifications (8.4% / n=15,826), followed by Rio Grande do Sul (7% / n=12,879), Rio de Janeiro (6.4% / n=11,942) , Minas Gerais (5.9% / n=11,213), Pernambuco (5.8% / n=10,946), Bahia (4.7% / n=8,960), Santa Catarina (4.5% / n=8,490) , Pará (2.3% / n=4,371), Ceará (2.1% / n=4,080), Goiás (1.7% / n=3,161), Piauí (1.6% / n=3,002), Espírito Santo (1.1% / n=2,086), Mato Grosso (1.1% / n=2,011), Mato Grosso do Sul (1% / n=1,781), Amazonas (1.0% / n=1,742), Federal District (1.0% / n=1,721), Alagoas (0.7% / n=1,317), Rio Grande do Norte (0.6% / n=1,269), Maranhão (0.6% / n=1,256 ), Rondônia (0.3% / n=699), Paraíba (0.3% / n=694), Tocantins (0.4 / n=681), Sergipe (0.2% / n=485), Acre (0.1% / n=226) and Roraima (0.1% / n=199) (figure 2) (MORAES; GALDINO; TEIXEIRA, 2022).
• Viral meningitis in Brazil
Viruses are responsible for most cases of acute meningitis, can be caused by different families of viruses and are often confused with bacterial meningitis. Among the viruses responsible for most cases of acute meningitis, enterovirus stands out as the most common pathogen identified, followed by mumps virus, herpes simplex virus, arboviruses, chickenpox, measles, rubella, and adenoviruses (Santos et al., 2022).
Contamination with the meningitis virus occurs through close contact with an infected person through respiratory droplets when coughing, sneezing, or sharing personal objects. To this end, as it is a pathology that presents symptoms like those of the flu, which makes its accurate diagnosis difficult, neurological examinations and a lumbar puncture are necessary to collect cerebrospinal fluid (CSF) (Amorim et al., 2022).
• Bacterial meningitis in Brazil
The main bacteria responsible for the occurrence of meningitis are Neisseria meningitidis, Streptococcus pneumoniae, Mycobacterium tuberculosis and Haemophilus influenzae, the latter is frequently associated with infections in children (Dias et al., 2017).
On the other hand, Neisseria meningitidis, also known as meningococcus, is known for presenting the highest mortality rate, especially in children from regions of low economic and social status. This bacterium is the main cause of septicemia and meningitis worldwide (Teixeira et al., 2018).
Patients affected by bacterial meningitis are generally quite symptomatic and often present less than 24 hours after the onset of symptoms (ROLDI et al., 2022). Headache, fever, malaise, vomiting, photophobia, petechiae, convulsions and neck stiffness are the most common clinical features. Therefore, it is important to highlight that this last symptom is more prevalent in children (Amorim et al., 2022).
Bacterial meningitis is the most serious form of the disease and can lead to death quickly. The clinical findings of this disease overlap with other types of meningitis and therefore require an examination of CSF parameters and imaging tests when necessary (ROLDI et al., 2022).
The doctor and the nursing team are primarily responsible for direct care for the affected person, therefore, despite such monitoring, it is possible for complications of the disease to occur, especially when its etiology is bacterial, whereas in the case of viral etiology, the Complicated developments are usually associated with immunodeficient patients. Among the most common complications encountered are deafness, cognitive or behavioral deficits, motor abnormalities, hydrocephalus and visual or language disorders (Paim et al., 2019).
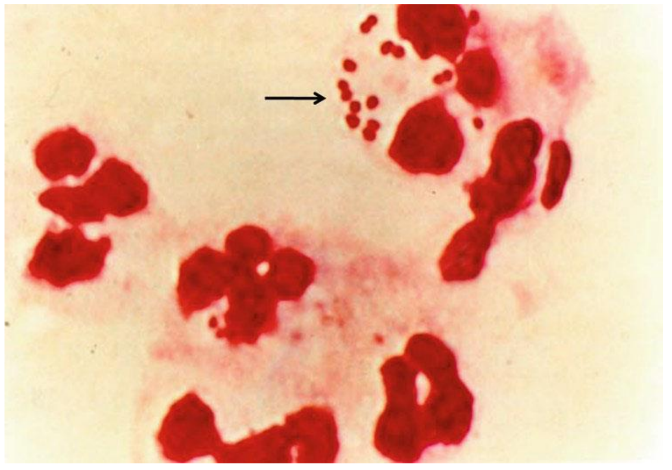
Figure 3: Nisseria meningitidis – Intracellular gram-negative diplococci and leukocytes in the CSF from a patient with meningococcal meningitis. The arrow denotes diplococci in proximity and within leukocytes (NADINE; DAVID, 2012).
o Nurse’s inventions in prevention and identification
The nurse’s role is to develop awareness policies to broaden society’s view of the severity of the disease. Primary prevention is the key to more effective control. Nurses play an important role in promoting care, recognizing, and perceiving various changes. Therefore, you must have extensive and skilled knowledge for the patient’s recovery, to ensure quick and responsible care (Silva et al., 2020).
Professional nurses must always seek knowledge and training, as they are responsible for making and implementing scientifically based decisions, actions and care for the patient’s recovery. In addition, he is responsible for planning, coordination and implementation aimed at preventing this pathology, increasing the patient’s chances of improvement (Silva et al., 2020).
4. TREATMENT, COMPLICATIONS AND SEQUELARES IN THE NATIONAL CONTEXT
• Antibiotic therapy and challenges in access to medicines
A quick and careful initial approach to suspected cases of meningitis is very important for the patient’s improvement. Immediate hospitalization, respiratory isolation, collection of samples for diagnostic tests and the institution of empirical antibiotic therapy proportional to clinical suspicion are crucial measures for the effective treatment of the disease. General support, such as fluid replacement, is essential for patient care, as well as adjusting antibiotic therapy according to the results of sensitivity tests are also essential steps in the treatment of meningitis. Notification to the Municipal Health Department for epidemiological investigation and implementation of appropriate prevention measures also contributes to controlling the disease (CARVALHO et al., 2022).
Treatment of bacterial meningitis with medication varies depending on the patient’s age. For newborns, the use of ampicillin in combination with ceftriaxone is indicated. Between 1 and 23 months, ceftriaxone is the medication of choice. For patients aged between 2 and 50 years, in addition to ampicillin associated with ceftriaxone, vancomycin can be used together with cefepime, ceftazidime or meropenem (CARVALHO et al., 2022).
The use of corticosteroids, such as dexamethasone, has been shown to be effective in children with H. influenzae, reducing neural damage and hearing loss. The use for S. pneumoniae is not yet consensual, but it is considered an option due to the reduction in morbidity and mortality. It should be administered before or simultaneously with the initial dose of antibiotic (CARVALHO et al., 2022).
Challenges to accessing medicines may include limited availability of medicines in certain regions, high treatment costs, lack of adequate infrastructure for storage and distribution of essential medicines (CARVALHO et al., 2022).
• Available antivirals and their distribution in the country
In most cases, treatment with antiviral medications is not carried out. Hospitalization, monitoring of signs of greater severity, careful evaluation and clinical follow-up are generally necessary.
The conduct is always determined by the medical team, however, in specific cases, such as Herpes Simplex Virus (HSV), treatments with intravenous acyclovir are used, where it is used to treat viral infections by inhibiting the replication of the virus. (SANTOS et al., 2022).
In general, the more serious the infection, the greater the chances of complications. Neurological damage seen includes hearing and vision loss, problems with memory, loss of concentration and motor coordination, epilepsy, and cerebral palsy (CARVALHO et al., 2022).
5. VACCINATION IN BRAZIL
• Specific vaccination programs
The preventive form, which is vaccination, the first dose begins at 2 months of age with the Pentavalent vaccine, which prevents infections caused by Haemophilus influenzae type B, with a booster dose at 4 and 6 months. The meningococcal conjugate vaccine is given at 3, 5 and a booster at 12 months, protecting the child against infections with Neisseria meningitidis serogroup C (SILVA; MEZAROBBA, 2018).
The World Health Organization (WHO) recommends a meningococcal vaccine in the expanded immunization program (EPI) to prevent meningitis, especially in countries with a high disease burden. Vaccination strategies differ between countries due to diverse meningococcal groups and disease burden, cost-effectiveness, budgetary impact, and public health priority (Maimaiti et al., 2022).
Prevention measures must be strictly followed, and epidemiological surveillance is primarily responsible for ensuring their implementation. Therefore, it is necessary to control this disease through patient isolation, chemoprophylaxis of contacts, contact surveillance, immunization, timely identification and control of outbreaks and health education actions. These control measures aim to reduce the incidence of the disease and prevent the occurrence of secondary cases (Liphaus et al., 2021).
• Challenges and successes in implementing immunization programs
The National Immunization Program (PNI) was created in 1973 by the state and municipal health departments. According to the Domingues et al. (DOMINGUES et al., 2020), authorities, the PNI aims to comply with the principle of decentralization of the
Unified Health System (SUS), acting in an articulated, hierarchical, and integrated way. Therefore, constant discussions about standards, goals and results are necessary, as it enables implementation in all spheres of SUS management. The PNI contributes to reducing regional and social inequalities, guaranteeing access to vaccination for all Brazilians, in all locations.
The implementation of meningitis immunization programs in Brazil faced challenges such as ensuring adequate vaccination coverage, distributing vaccines in all regions of the country, and raising awareness among the population about the importance of vaccination. However, according to the authors Gonçalves e Assis (GONÇALVES E ASSIS, 2022), there have been significant successes, such as the reduction in cases and deaths from meningitis, the increase in the supply of vaccines through the National Immunization Program and the inclusion of new vaccines in the national calendar.
Currently, there is still hesitation among the population about vaccination. Therefore, it is the nurse’s role to develop strategies and training for other health professionals who work in this service. Over the years, the Ministry of Health has developed several campaigns. The vaccination calendar has become more complex and complete today, thus requiring extensive knowledge from professionals about vaccination schedules. The PNI has invested in various training courses to increase the number of doses of vaccines administered and raise awareness among the population about their importance. It is important to have qualified professionals who know how to make good recommendations about the need for vaccination and answer the population’s doubts.
The main challenge facing health units is caused by the presence of fake news on social media, which circulates daily. To obtain accurate information about vaccines and their effectiveness in preventing diseases, it is crucial to always check the veracity of the information and seek reliable sources, such as health bodies and scientific institutions. The Ministry of Health points out that the drop in numbers related to immunization in the country is mainly due to fake news.
6. CONCLUSION
In this work, using scientific literature as a basis, it was observed that meningitis is a serious public health problem due to its intensity of spread and its high rate of morbidity and mortality, especially in children. Therefore, it is necessary to highlight the importance of prophylactic methods such as vaccination, which are extremely effective in controlling and eradicating diseases, not only individually, but collectively, as they lead to a reduction in the circulation of the disease, benefiting the entire population. In addition, the literature also states that historically the Brazilian population has confidence in the efficacy and safety of vaccines, however adherence has been decreasing in recent years, mainly due to the growth of the anti-vaccine movement and the circulation of erroneous and/or false information without scientific basis that circulate mainly on social media. There are currently several Federal Government programs that deal with this topic. These guidelines are implemented through vaccination campaigns and health education programs, which can be found on the Ministry of Health portal. Therefore, it can be concluded that despite all these strategies developed, there are still several barriers that make access and eradication of meningitis difficult. It is necessary to obtain quality scientific information in an accessible and clear way to combat denialist movements, so that science is democratized and available to the entire population. It is worth mentioning that health professionals must be educators and health promoters, being essential for the population to be aware of the importance of vaccination.
7. Acknowledgements
The authors wish to University Center of the Integrated Faculties of Ourinhos – Unifio, Ourinhos, SP, Brazil.
8. REFERENCES
AMORIM, A. K. A. P. et al. Perfil epidemiológico da meningite no Tocantins entre 2012 e 2021. Research, Society and Development, v. 11, n. 14, p. e552111436888, 6 nov. 2022a.
AMORIM, A. K. A. P. et al. Perfil epidemiológico da meningite no Tocantins entre 2012 e 2021. Research, Society and Development, v. 11, n. 14, p. e552111436888, 6 nov. 2022b.
CARVALHO, L. DO C. et al. O perfil clínico do paciente com meningite bacteriana: uma abordagem neurológica. Revista Eletrônica Acervo Médico, v. 2, p. 1–7, 2022.
CERUTTI DAZZI, M.; ADRIANO ZATTI, C.; BALDISSERA, R. Perfil dos casos de meningites ocorridas no Brasil de 2009 à 2012. Revista UNINGÁ Review, v. 19, n. 3, p. 33–36, 2014.
CRISTINA BERTOLINI PAIM, A.; MORENO GREGIO, M.; PICCOLI GARCIA, S. Perfil epidemiológico da meningite no estado de Santa Catarina no período de 2008 a 2018. Arq. Catarin Med., v. 48, n. 4, p. 111–125, 2019.
DAL’BOSCO, E. B. et al. A saúde mental da enfermagem no enfrentamento da COVID-19 em um hospital universitário regional. Revista Brasileira de Enfermagem, v. 73, p. 1–7, 2020.
DE, E.; RODRIGUES, M. B. CENTRO UNIVERSITÁRIO DE BRASÍLIA FACULDADE DE CIÊNCIAS DA EDUCAÇÃO E SAÚDE GRADUAÇÃO EM BIOMEDICINA MENINGITE: PERFIL EPIDEMIOLÓGICO DA DOENÇA NO BRASIL NOS ANOS DE 2007 A 2013. [s.l: s.n.].
DIAS, F. C. F. et al. MENINGITE: ASPECTOS EPIDEMIOLÓGICOS DA DOENÇA NA REGIÃO NORTE DO BRASIL. Revista de Patologia do Tocantins, v. 4, n. 2, p. 46–49, 20 jun. 2017a.
DIAS, F. C. F. et al. Meningite: aspectos epidemiológicos da doença na região Norte do Brasil. Revista de Patologia do Tocantins, v. 4, n. 2, p. 46–49, 20 jun. 2017b.
DOMINGUES, C. M. A. S. et al. 46 anos do Programa Nacional de Imunizações: uma história repleta de conquistas e desafios a serem superados. Cadernos de Saúde Pública, v. 36, n. suppl 2, 2020.
FOCACCIA, R.; NEGRA, M. DELLA. MENINGITE-1970/ COVID-2019. A HISTÓRIA REPETIDA. The Brazilian Journal of Infectious Diseases, v. 26, p. 102443, set. 2022.
GONÇALVES E ASSIS. Ciências da Terra, do ambiente e da epidemia de Covid 19. História da Ciência e Ensino, v. 25, p. 221–249, 2022.
LIMA, R. A. A OCORRÊNCIA DA MENINGITE APÓS O ADVENTO DA VACINAÇÃO COMO POLÍTICA PÚBLICA DE SAÚDE. [s.l: s.n.].
LIPHAUS, B. L. et al. Meningites Bacterianas: Diagnóstico e
Caracterização Laboratorial dos Agentes EtiológicosBoletim Epidemiológico Paulista • Ano. [s.l: s.n.].
MACHADO, C. F. T.; BORGES, B. L. C. Meningite Bacteriana na Unidade de Terapia Intensiva: um Protocolo de Cuidados de Enfermagem Bacterial Meningitis in the Intensive Care Unit: a Nursing Care Protocol. [s.l: s.n.]. Disponível em: <http://bases.bireme.br>.
MAIMAITI, H. et al. Vaccine Uptake to Prevent Meningitis and Encephalitis in Shanghai, China. Vaccines, v. 10, n. 12, 1 dez. 2022a.
MAIMAITI, H. et al. Vaccine Uptake to Prevent Meningitis and Encephalitis in Shanghai, China. Vaccines, v. 10, n. 12, p. 2–15, 1 dez. 2022b.
MORAES, G. F. Q.; GALDINO, M. A. O.; TEIXEIRA, A. P. DE C. Impacto da meningite entre os anos de 2010 a 2020 no Brasil: um estudo documental. Revista de Ciências Médicas e Biológicas, v. 21, n. 3, p. 505–513, 29 dez. 2022.
NADINE, G. R.; DAVID, S. S. Neisseria meningitidis: Biology, Microbiology, and Epidemiology. Totowa, NJ: Humana Press, 2012. v. 799
PAIM, A. C. B.; GREGIO, M. M.; GARCIA, S. P. Perfil epidemiológico da meningite no Estado de Santa Catarina no período de 2008 a 2018. [s.l: s.n.].
RODRIGUES SANTOS, A. S. PREVALÊNCIA DE CASOS DE MENINGITE NO BRASIL DURANTE OS ANOS DE 2009 A 2019. The Brazilian Journal of Infectious Diseases, v. 25, p. 101195, jan. 2021.
ROLDI, L. L. et al. Revisão bibliográfica: meningite bacteriana em adultos / Literature review: bacterial meningitis in adults. Brazilian Journal of Development, v. 8, n. 4, p. 24703–24710, 7 abr. 2022.
SANTOS, K. A. DOS et al. Fisiopatologia das Meningites de origem viral: uma revisão bibliográfica / Pathophysiology of Meningitis of viral origin: a bibliografic review. Brazilian Journal of Development, v. 8, n. 6, p. 47322–47333, 22 jun. 2022.
SILVA, E. F. G. DA C. et al. Atuação do enfermeiro na unidade de terapia intensiva identificação dos sinais e sintomas da sepse. Research, Society and Development, v. 9, n. 8, p. e949986094, 2 ago. 2020.
SILVA, H. C. G.; MEZAROBBA, N. ARTIGO ORIGINAL MENINGITE NO BRASIL EM 2015: O PANORAMA DA ATUALIDADE MENINGITIS IN BRAZIL IN 2015: OVERVIEW OF CURRENT. [s.l: s.n.].
TEIXEIRA, A. B. et al. Meningite bacteriana: uma atualização. Brazilian Journal of Clinical Analyses, v. 50, n. 4, p. 327–329, 2018.
1Department of Nursing – University Center of the Integrated Faculties of Ourinhos – Unifio, Ourinhos, SP, Brazil.
Hariel Sá Pazianoto Horacio (ORCID: 0009-0004-4697-4828) harielpazianoto@gmail.com (Corresponding author)
Juliano Rodrigues Coimbra (ORCID: 0000-0002-3227-452X) juliano.coimbra@unifio.edu.br
Douglas Fernandes da Silva (ORCID: 0000-0002-0252-1112) douglas.silva@unifio.edu.br
